
Audit reveals supplement regulation and oversight is lacking
A Canadian audit of dietary supplements shows serious problems with the quality and safety of the products you may be buying.

Some essential oils may trigger seizures
Some essential oils appear to trigger seizures in people with no history of epilepsy.
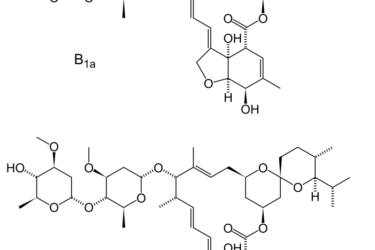
Ivermectin is the new hydroxychloroquine
Ivermectin has been touted as a potential antiviral to treat COVID-19 infections. There is no good evidence it is effective.

The “Disinformation Dozen” spreading anti-vaccine messaging on social media
Just twelve individuals are generating two-thirds of all of the anti-vaccine messaging on Twitter and Facebook.

Vitamin D shows no efficacy against moderate to severe COVID-19 infections
A new trial failed to find evidence that a massive dose of vitamin D improves outcomes in patients with moderate to severe COVID-19 infections.

The effectiveness of zinc and vitamin C on the duration of COVID-19 infections
Vitamin C and zinc have been heralded as treatments for colds for decades, but how well do they work against COVID-19? A new clinical trial provides the answer.

Conspirituality: Where New Age wellness meets right wing conspiracy thinking
Conspiracy theorists and QAnon may sound miles apart from wellness, yoga and GOOP, but they're converging into "conspirituality", the integration of spirituality and conspiracy theories.

The Anti-Vaxxer Playbook to Destroy Confidence in COVID-19 Vaccines
Major anti-vaccination voices and organizations have coalesced around three key messages to keep people from accepting the COVID-19 vaccine. Their playbook has now been exposed.
Deliberately Spoiled Vaccines: Conspiracy thinking and health professionals
A Wisconsin pharmacist is facing charges after deliberately tampering with a batch of COVID-19 vaccines, demonstrating that a health professional's education is no vaccine against conspiracy beliefs.
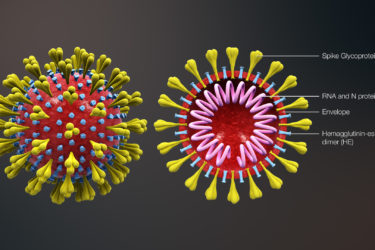
Deciding between a vaccine and…an infection?
A handy comparison of COVID-19 vaccines compared to COVID-19 infections.

