Category: Cancer
Cancer Deaths Continue to Decline
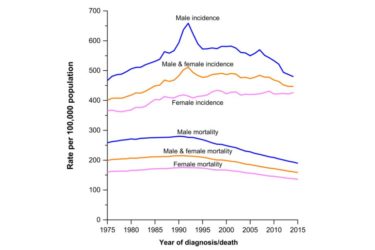
Overall cancer incidence has been stable in women and declining steadily in men. Changes in specific cancers reflect known risk factors and the effect of screening methods. What is not seen in this data is any mysterious increase in any specific cancer or cancers overall.

Snake-Based Medicine? Another Salmonella Infection Linked to Rattlesnake Pills
Rattlesnake pills, another entry in a long line of bogus cancer cures, have been linked (again) to a potentially deadly Salmonella infection.

What is “integrative oncology”? Even the Society for Integrative Oncology doesn’t seem to know for sure
Last week, the Society for Integrative Oncology published an article attempting to define what "integrative oncology" is. The definition, when it isn't totally vague, ignores the pseudoscience at the heart of integrative oncology and medicine.

Why do some women refuse treatments for their breast cancer?
Adjuvant therapy after surgery, such as chemotherapy, hormonal therapy, and radiation therapy, has contributed to a 39% decrease in breast cancer mortality since 1989. Unfortunately, a significant number of women decline evidence-based adjuvant therapy. A recent study suggests that distrust of the medical system plays a significant role in such refusal.
Complementary and Alternative Medicines and Cancer
Does complementary and alternative medicine offer any meaningful benefits to cancer patients?

Rigvir strikes back, or: A conversation with a Rigvir flack
My skeptical analysis of Rigvir, a "Virotherapy" from Latvia being promoted by alternative medicine clinics as a cancer cure, caught the attention of the International Virotherapy Center (IVC). The result was a long and very telling e-mail exchange between its Assistant of Business Development and myself. I post it because the arguments used in the discussion are very telling about where the...

CAM Promotion in Adolescent and Young Adult Cancer Programs
Cancer in the 18-39 age range is uncommon, but still occurs. When they should be dealing with school, friends, new jobs, and starting families, instead they must worry about medical bills, appointments, and infertility. Added to this are the costs of "integrative" treatments often foisted upon cancer patients, or built-in to the few adolescent and young adult-focussed centers that currently exist.
Ty Bollinger’s “The Truth About Cancer” and the unethical marketing of the unproven cancer virotherapy Rigvir
Last week, I wrote about Rigvir, a "virotherapy" promoted by the International Virotherapy Center (IVC) in Latvia, which did not like what I had to say. When a representative called me to task for referring to the marketing of Rigvir using patient testimonials as irresponsbile, it prompted me to look at how Ty Bollinger's The Truth About Cancer series promoted Rigvir through...

Rigvir: Another unproven and dubious cancer therapy to be avoided
Recently, the Hope4Cancer Institute, a quack clinic in Mexico, has added a treatment known as Rigvir to its coffee enemas and other offerings. But what is Rigvir? It turns out that it's an import from Latvia with a mysterious history. Proponents claim that it is an oncolytic virus that targets cancer specifically and leaves normal cells alone. Unfortunately, there is a profound...


