Category: Medical Ethics
Threats to science-based medicine: Big pharma pays a publisher to produce a fake journal
It’s times like these when I’m happy that I haven’t published in too many Elsevier Journals during the course of my career. Actually, I’m not sure if I’ve ever published in an Elsevier journal, although I have reviewed manuscripts for them. In any case, I say that because on Thursday, it was revealed that pharmaceutical company Merck, Sharp & Dohme paid Elsevier...
Harvard Medical School: Veritas for Sale (Part VI)
Loose Ends: Dr. Koh and More After Dr. Federman’s letter and my reply, posted in Part V of this series,† there seemed little point in pursuing the matter further. Although Dr. Federman never answered my reply, he did send, at my request, a copy of Commissioner of Public Health Howard Koh‘s written “construction of the events in the Massachusetts Special Commission.” As you may recall, those events...
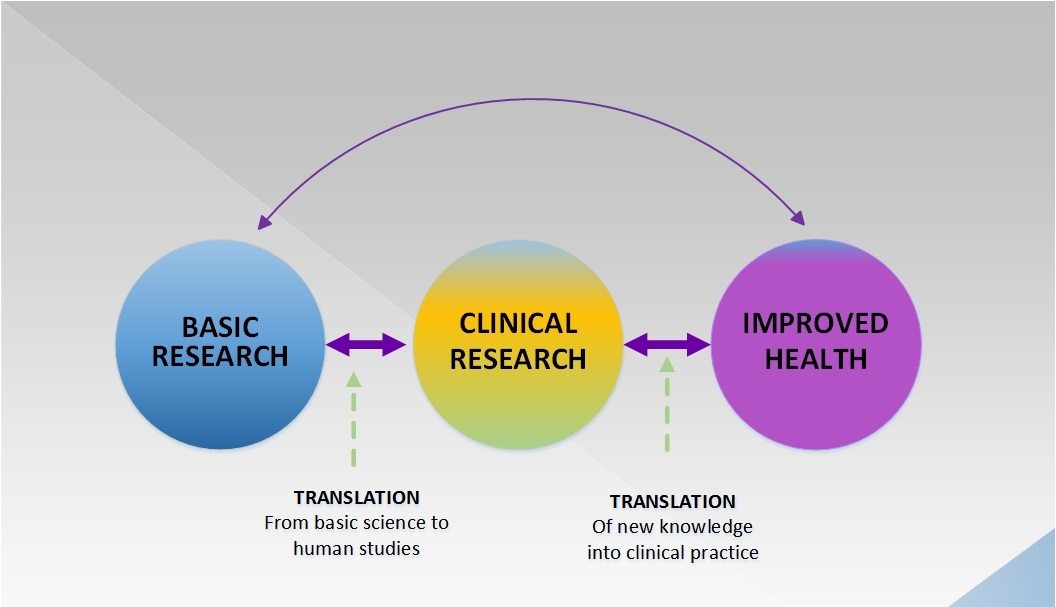
Human subjects protections and research ethics: Where the rubber hits the road for science-based medicine
Although clinical trials are science, they often can't be controlled as well as experiments in most branches of science. The reason is that the experimental subjects are human, and ethics demands that risks and harms be minimized and benefits maximized.
Harvard Medical School: Veritas for Sale (Part V)
September 26, 2002 Kimball Atwood, M.D. xxxxxxxxxxxxxxx xxxxxxxxxxxxxxxxx Dear Kim, I have now had time to look into the allegations in your letter of June 14th which, incidentally, I shared with Dr. David Eisenberg and he with several others. I have sought consultation about our exchanges and the gist of my response follows. Some of your concerns and allegations are very helpful and...
Response to a “CAM on campus” post
I only recently began contributing to SBM, bringing not any particular expertise or scholarship but rather the perspective of a student. My goal in blogging is not to focus on issues specific to my school, of which I am quite fond and proud in general. Instead I hope to use my experiences, which SBM editors and readers tell me are not unique, to illustrate...
Harvard Medical School: Veritas for Sale (Part III)
In Parts I and II of this series* we saw that from 2000 to 2002, key members of the Harvard Medical School “CAM” program, including the Director, had promoted quackery to the legislature of the Commonwealth of Massachusetts. We also saw other explicit or tacit promotions by Harvard institutions and professors, and embarrassing examples of such promotions on InteliHealth, a consumer health...
Harvard Medical School: Veritas for Sale (Part II)
In Part I of this series† we saw that in 2001 Dr. David Eisenberg, the Director of the Harvard Medical School Center for Alternative Medicine Research and Education (CAMRE), and Atty Michael Cohen, the CAMRE’s Director of Legal Programs, had contributed to a report commissioned by the Commonwealth of Massachusetts that would, if accepted as valid by the legislature, provide state protection for a...
Medical students actively recruited for CAM
Here at Science-Based Medicine we’ve been getting a lot of letters from medical students. This is a good thing and a bad thing. I’m glad people see us a a resource for SBM, but I’m unhappy that medical students: 1) need us; 2) don’t have someone to approach on campus. Let’s explore some of the more subtle ways cult medical practices...
When “CAM” is mandatory: A science-based medical student’s dilemma
Early in the history of this blog, I wrote a rather long post expressing my dismay at the infiltration of unscientific “complementary and alternative medicine” (CAM) or “integrative medicine” (IM) modalities into American medical schools. In it, I listed the medical schools that had embraced pseudoscience through having started a CAM/IM program (a list desperately in need of an update). Moreover, we...
IRBs, Conflicts of Interest, and Witch Hunts
When beginning a discussion of a controversial topic I like to establish the common ground upon which most or all people can agree. Everyone seems to agree that real conflicts of interest in medical research and practice is a bad thing and steps should be taken to minimize, eliminate, and illuminate any such conflicts. The controversy revolves around what constitutes a real...

