If there’s one medical treatment that proponents of “alternative medicine” love to hate, it’s chemotherapy. Rants against “poisoning” are a regular staple on “alternative health” websites, usually coupled with insinuations or outright accusations that the only reason oncologists administer chemotherapy is because of the “cancer industrial complex” in which big pharma profits massively from selling chemotherapeutic agents and oncologists and hospitals profit massively from administering them. Indeed, I’ve lost track of the number of such rants I’ve deconstructed over the years. Usually, they boil down to two claims: (1) that chemotherapy doesn’t work against cancer (or, as I’ve called it before, the “2% gambit“) and (2) that the only reason it’s given is because doctors are brainwashed in medical school or because of the profit motive or, of course, because of a combination of the two. Of course, the 2% gambit is based on a fallacious cherry picking of data and confusing primary versus adjuvant chemotherapy, and chemotherapy does actually work rather well for many malignancies, but none of this stops the flow of misinformation.
Misinformation and demonization aside, it is also important to realize that the term “chemotherapy,” which was originally coined by German chemist Paul Ehrlich, was originally intended to mean the use of chemicals to treat disease. By this definition, virtually any drug is “chemotherapy,” including antibiotics. Indeed, one could argue that by this expansive definition, even the herbal remedies that some alternative medicine practitioners like to use to treat cancer would be chemotherapy for the simple reason that they contain chemicals and are being used to treat disease. Granted, the expansive definition evolved over the years, and these days the term “chemotherapy” is rarely used to describe anything other than the cytotoxic chemotherapy of cancer that in the popular mind causes so many horrific side effects. But in reality virtually any drug used to treat cancer is chemotherapy, which is why I like to point out to fans of Stanislaw Burzynski that his antineoplastons, if they actually worked against cancer, would be rightly considered chemotherapy, every bit as much as cyclophosphamide, 5-fluorouracil, and other common chemotherapeutics.
Chemotherapy, not surprisingly, is easy to demonize. There are few treatments that cause such odious side effects, and when taken to its fullest extreme, such as complete ablation of a cancer patient’s bone marrow in preparation for a bone marrow transplant, chemotherapy can be brutal. It’s also true that for advanced solid malignancies, it only tends to produce palliation or a prolongation in survival, not a cure, and people with cancer want a cure. Palliation just isn’t that appealing, for obvious reasons. When people think of chemotherapy, they think of hair falling out, nausea and vomiting, fatigue, and death. Since chemotherapy is often given for more advanced malignancies, it’s sometimes hard to tell how many of these symptoms (other than the hair loss) are due to the cancer and how much they are due to side effects of the chemotherapy, and many people incorrectly blame chemotherapy for the deaths of their loved ones with cancer. Also, because, like radiation therapy, chemotherapy is often given in the adjuvant setting (i.e., in addition to curative surgery in order to decrease the risk of recurrence and death), it’s very easy to produce stories in which people with cancer refuse chemotherapy and/or radiation therapy after surgery and attribute their survival not to the conventional therapy (surgery) but to whatever quackery they chose to use. When used in early stage cancer, although its relative efficacy can seem large, for example a 30% decrease in the risk of dying, if the risk of dying of cancer is only 10% to begin with, that’s only a 3% survival benefit on an absolute basis.
I’ve made it a habit of discussing many of these alternative cancer cure anecdotes, such as one about Chris Wark that I did just a couple of weeks ago. It’s a theme of mine that goes back to the very beginning of this blog. Sometimes little or no quackery is involved, but rather patients are pushed away from chemotherapy by major news outlets publishing irresponsible news stories that offer misguided justifications for refusing chemotherapy, making treatment sound as though it will irrevocably destroy lives. In reality, the use of alternative medicine instead of effective treatment for cancer is, where it’s been studied, is always associated much poorer survival, even in pancreatic cancer, for which conventional treatments don’t do so well. Still, among the treatments in the “cut, poison, burn” terminology that believers in alternative medicine like to use to describe conventional cancer therapy, it is the “poison” that causes the most fear and is most viciously demonized in the alt-med “literature.”
It’s for those reasons that I thought that now would be a good time to do a post on the history of chemotherapy by Vincent DeVita (one of the pioneers of chemotherapy) and Edward Chu. It’s also a good time because I came across an article from about five years ago that describes this history quite well. There’s much to be learned there, and this history also explains some of the quotes of scientists often trotted out in an effort to attack chemotherapy.
The early days
For centuries, for solid tumors like breast cancer and colon cancer at least, the only “cure” was surgery. Moreover, because there was no adjuvant therapy, these surgical cures were often radical, because if the tumor recurred after surgery there was close to zero chance of salvaging the patient’s life. In addition, because there were no screening tests, most cancers were not discovered until they were relatively advanced; it was rare back then to find a breast cancer less than 2 cm in diameter. One example that I like to point to is that of William Stewart Halsted, the American surgeon who now stands as almost a god of surgery. In the late 1800s, Halsted developed the radical mastectomy, a procedure that involved taking not only the breast, but the underlying pectoralis major muscle, as well as all the axillary lymph nodes (under the arm). This procedure produced survival rates considerably higher than what were previously achieved at the time, and it relatively rapidly became the standard of care for around 80 years. (Unfortunately, that was probably about 20-30 years longer than it should have.) DeVita describes it thusly:
Surgery and radiotherapy dominated the field of cancer therapy into the 1960s until it became clear that cure rates after ever more radical local treatments had plateaued at about 33% due to the presence of heretofore-unappreciated micrometastases and new data showed that combination chemotherapy could cure patients with various advanced cancers. The latter observation opened up the opportunity to apply drugs in conjunction with surgery and/or radiation treatments to deal with the issue of micrometastases, initially in breast cancer patients, and the field of adjuvant chemotherapy was born. Combined modality treatment, the tailoring of each of the three modalities so their antitumor effect could be maximized with minimal toxicity to normal tissues, then became standard clinical practice.
As the 20th century dawned (and for quite some time thereafter), there really was no effective treatment for cancer except for surgery, which limited cancer treatments to tumors that could be excised and left people with hematological malignancies (leukemias and lymphomas) pretty much out of luck. Leukemias and lymphomas were treated mainly with arsenic, which didn’t actually work very well, if at all; they were thus generally considered to be chronic, incurable diseases.
The first major advance that helped with the development of chemotherapy as we know it today occurred in the 1910s, when George Clowes of the Roswell Park Memorial Institute developed the first transplantable rodent tumor systems. This advance allowed the testing of compounds in animal models before trying them in humans. At the time, tissue culture techniques were in their infancy, having only just been described a few years before, and would not become commonplace in laboratories for another three or four decades. Early systems included sarcomas and Erlich’s ascites tumor. These were all induced by carcinogens in mice and could be transplanted from mouse to mouse.
Decades passed, and the development of chemotherapy didn’t really go anywhere until the 1930s, when, as DeVita describes:
It was Murray Shear, at the Office of Cancer Investigations of the USPHS, a program that was later combined in 1937 with the NIH Laboratory of Pharmacology to become the National Cancer Institute (NCI), who in 1935 set up the most organized program that would became a model for cancer drug screening ( 7). Shear’s program was the first to test a broad array of compounds, including natural products, and had both interinstitutional and international collaborations. He ultimately screened over 3,000 compounds using the murine S37 as his model system. However, because only two drugs ever made it to clinical trials and were eventually dropped because of unacceptable toxicity, the program was dissolved in 1953 just as discussions began about establishing an organized national effort in drug screening. This failure was in part due to the antipathy toward the testing of drugs to treat cancer but also to a lack of information and experience on how to test potentially toxic chemicals in humans.
The failure of this drug screening initiative is part of what contributed to the pessimism with respect to chemotherapy and cancer that developed in the 1950s. Prior, in the 1940s, there had been a great deal of enthusiasm for chemotherapy based on the breakthroughs of Alfred Gilman and Louis Goodman, who tested the effects of nitrogen mustards on lymphoma based on observations that an accidental spill of sulfur mustards on troops from a bombed ship in Bari Harbor, Italy, in WWII had led to the observation that the bone marrow and lymph nodes were markedly depleted in men exposed to the mustard gas. Experiments in mice bearing a transplanted lymphoid tumor with nitrogen mustard resulted in marked regression, which led Goodman and Gilman ask Gustaf Lindskog, a thoracic surgeon, to administer nitrogen mustard to a patient with non–Hodgkin’s lymphoma and severe airway obstruction. The tumor regressed, and the same results were seen in several other patients treated this way. Publication of these results in 1946 led to widespread enthusiasm for the use of drugs related to the chemicals in nitrogen mustard, such as chlorambucil and cyclophosphamide, the latter of which is still commonly used for breast cancer and several other cancers today.
Here’s where the optimism turned sour:
The use of nitrogen mustard for lymphomas spread rapidly throughout the United States after the publication of the Lindskog article in 1946. If one reads the literature of the time, there was a real sense of excitement that perhaps drugs could cure patients with cancer ( 19). Unfortunately, remissions turned out to be brief and incomplete, and this realization then created an air of pessimism that pervaded the subsequent literature of the 1950s. A cadre of academic physicians, led by the famous hematologist William Dameshek, who having seen apparent success turn to failure could never again be persuaded that cancer was curable by drugs (20), became harsh critics of a national drug development program and the effort to prove that drugs could cure advanced cancers.
And it is here where many of the anti-chemotherapy quotes by reputable scientists and physicians originate, albeit often in exaggerated forms. For instance, one of the most famous of these statements is from a man named Hardin Jones, who is quoted as saying, “My studies have proved conclusively that untreated cancer victims actually live up to four times longer than treated individuals.” (Indeed, if you Google Hardin Jones’ name and this statement—or just his name—you will find this quote cited in many different contexts. Frequently articles quoting Jones on these issues will claim that he published these statistics in his article in Transactions, New York Academy of Science, series 2, v. 18, n.3, p.322. As our frequent commenter Peter Moran has pointed out, however, this particular study dates back to 1956 and says no such thing.
There’s no doubt, however, that Jones had a dim view of cancer treatments of his day, but he was not alone. Five or six decades ago, after the hope of the late 1940s that using alkylating agents would cure many cancers had been crushed and improvements in survival from cancer had been shown to be frustratingly elusive, there were a lot of cancer doctors who were despairing that cancer could ever be cured with chemotherapy. Interestingly, Jones used his data to build a statistical model proposing that “…the death rate for all kinds of cancer remains nearly fixed from the moment when cancer is identified…” That sounds a lot like lead time bias. Jones was, however, somewhat prescient in proposing that the biology of the tumor is arguably the prime determinant of survival, even with treatment. In any case, I tend to agree with Dr. Moran that Jones’ pessimistic view was a product of his times.
This pessimism continued into the 1960s. Indeed, one of the more interesting aspects of DeVita’s article is a series of anecdotes about how dimly the medical profession viewed chemotherapy in the 1960s and how skeptical most doctors were that any cancer would ever be cured with chemotherapy. At the time, there was no specialty known as medical oncology, and doctors who administered chemotherapy at hospitals were viewed as “underachievers, at best.” As DeVita describes, very respected physicians and chairs of departments viewed chemotherapists as the “lunatic fringe.” Louis K. Alpert, who had published one of the earliest reports using nitrogen mustards to treat lymphoma was routinely referred to by the house staff and the faculty as “Louis the Hawk and his poisons.” Here is more evidence of the low esteem with which doctors administering chemotherapy for cancer were viewed at the time:
At Yale, the first institution to test chemotherapy in humans in the modern era, the chemotherapist Paul Calabresi, a distinguished professor and founding father in the field, was forced to leave because he was involved in too much early testing of new anticancer drugs, an exercise as unpopular with the faculty and house staff at Yale as it was at Columbia.
At the Clinical Center of the NCI, where so many of the early breakthroughs with chemotherapy occurred, the well-known hematologist George Brecher, who read all the bone marrow slides of the leukemic patients, routinely referred to the Leukemia Service as the “butcher shop” at rounds.
And these are only the stories that can be told. It took plain old courage to be a chemotherapist in the 1960s and certainly the courage of the conviction that cancer would eventually succumb to drugs. Clearly, proof was necessary, and that proof would come in the form of the cure of patients with childhood acute leukemia and in adults with advanced Hodgkin’s disease.
It took the success of studies like the ones described in detail by DeVita to start to change the tide. For instance, new protocols for Hodgkin’s lymphoma increased the complete remission rate from near zero to 80%, with 60% of patients with advanced Hodgkin’s disease who attained a complete remission never relapsing. Follow-up is now well-beyond 40 years. By 1970, Hodgkin’s disease went from a death sentence to being viewed as largely curable with drugs, the first adult malignancy cured by chemotherapy. Add to this the amazing progress being made in childhood cancers at the time, and the tide was turning. Successes in hematological malignancies piled on successes, and the principle that some cancers could be cured with drugs became accepted. What amazes me is that this acceptance didn’t really take hold widely until the mid-1970s, which in the scheme of things is really not that long ago. It is also ironic to me that the attitude towards chemotherapy exhibited by believers in alternative medicine is very much akin to the attitude towards chemotherapy exhibited by mainstream science 50-60 years ago. The difference is that science has evolved; chemotherapy critics in the antiscience fringe have not.
Adjuvant chemotherapy
Hematological malignancies (such as leukemias and lymphomas) are much less common in adults than solid malignancies (e.g., breast, colon, lung, and other “solid” organ cancers). Many of these solid malignancies are treated primarily with surgery and have been for many decades. Breast and colon cancer are the most prominent (and among the most common) examples. From the 1970s on, the primary rise in the use of chemotherapy has been as adjuvant therapy; i.e., as therapy added to the curative therapy (surgery) to decrease the rate of recurrence and death. Ironically, using chemotherapy for adjuvant treatment met almost the same level of resistance as the use of chemotherapy to try to cure advanced hematological malignancies. In this, Bernie Fisher at the University of Pittsburgh was a pioneer, and DeVita tells us why:
The main problem was where to test these treatment regimens as adjuvants to surgery. Despite the excitement over the new chemotherapy data, most surgeons in the United States were still reluctant to participate in clinical trials testing its use postoperatively. The courageous Bernard Fisher was the first choice (Fig. 8). He and his group, the National Surgical Adjuvant Breast Project (NSABP), had done an early adjuvant study, sponsored by the CCNSC, testing the use of the alkylating agent thiotepa postoperatively to kill cancer cells dislodged at surgery (81). They were also in the process of challenging the status quo, questioning the need for radical mastectomy and postoperative radiotherapy, and were in position to test chemotherapy. The late Paul Carbone of NCI contacted Bernard Fisher, and he agreed to test L-PAM in a randomized controlled trial. But still no person or institution in the United States was prepared to test combination chemotherapy as an adjunct to surgery in breast cancer. Paul Carbone then contacted Gianni Bonadonna of the Istituto Nazionale Tumori, in Milan, Italy, about doing the study. Under its director, the surgical pioneer Umberto Veronesi, the Istituto was treating a large number of breast cancer patients and, like Fisher, was exploring the use of lesser operations than the radical mastectomy. Bonadonna came to the NIH Clinical Center to review the results of the CMF protocol, which had not yet been published and agreed along with Veronesi to conduct a randomized controlled trial of a slightly dose-reduced version of CMF versus no therapy. The U.S. NCI Chemotherapy program, under Zubrod, paid for the study through a contract with the Istituto Tumori. This contract also provided for costs of a permanent statistical center and was the beginning of long time collaboration between the two National Cancer Centers.
In other words, the National Cancer Institute had to look outside of the U.S. to find an investigator willing to do a trial of adjuvant chemotherapy with a regimen containing more than one drug. Both of these studies were positive and set off a flurry of studies trying to see if the addition of adjuvant chemotherapy could decrease recurrence and prolong survival after curative surgery for cancer. It was also around this time that Lawrence Einhorn developed a chemotherapy regimen that resulted in the cure rate of metastatic testicular cancer going from 10% to 60%. By 1981, Dr. Norman D. Nigro, a colorectal surgeon at my home institution, developed the protocol named after him to treat anal cancer in many cases without having to do an abdominoperineal resection (APR). This was considered a major advance, because an APR basically involves removing the rectum and anus, sewing the hole shut, and leaving the patient with a permanent colostomy.
Chemotherapy and breast cancer
There’s one study that I like to cite to people who claim that chemotherapy doesn’t work, and this post seems as good a place to do it as any. It’s a large meta-analysis from two years ago. Funded by Cancer Research UK, the British Heart Foundation and the UK Medical Research Council, this study was carried out by the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) at the Clinical Trial Service Unit at the University of Oxford, United Kingdom and entitled “Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials.”
It’s really quite an incredible effort to collate patient-level data for so many women in so many clinical trials. I sometimes say about meta-analyses the prototypical complaint about meta-analyses, namely that the quality of the output is critically dependent on the quality of the input. In other words, “garbage in, garbage out.” However, the inclusion criteria for the EBCTCG are actually pretty stringent. More importantly, the EBCTCG has access to unpublished data and patient-level information, as is explained here. The EBCTCG also goes to great lengths to try to include data from every randomized trial ever published, or an unbiased subset of them, in order to try to minimize selection bias that all-too-often results from too-rigid selection criteria used for meta-analyses. All in all, it’s an enormous effort.
Overall, this meta-analysis involved over 100,000 patients involved in 123 randomized trials over 40 years, and the authors made these comparisons: (1) taxane-based versus non-taxane-based regimens (data for 33 trials, begun in 1994-2003); (2) any anthracycline-based regimen versus standard or near-standard (cyclophosphamide/methotrexate/5-fluorouracil (CMF, 20 trials, begun in 1978-97); (3) higher versus lower anthracycline dosage (six trials, begun in 1985-94); and (4) polychemotherapy versus no adjuvant chemotherapy (64 trials, begun in 1973-96, including 22 of various anthracycline-based regimens and 12 of standard or near-standard CMF). Several meta-analyses were performed, which produced five main findings:
- Standard CMF and standard 4AC (ACT without the “T,” which is an older chemotherapy regimen used before taxanes were developed) were roughly equivalent in efficacy. Both of them roughly halved two-year recurrence rates and resulted in a proportional decrease in recurrence over the next eight years by approximately one-third. Overall, breast cancer mortality rates were reduced proportionally by 20-25%.
- Regimens with lower chemotherapy doses per cycle were less effective.
- Regimens with a lot more chemotherapy than the old standard 4AC (but not so nasty that they required stem-cell rescue) were somewhat more effective. They further decreased breast cancer mortality by 15-20%. The most prominent of these regimens is 4AC plus four cycles of “T” (a taxane), which became the standard of care for node-positive breast cancer after taxanes were developed.
- In all chemotherapy comparisons, the ten year overall mortality was reduced because there was not very much excess mortality due to causes other than breast cancer during the first year.
- In all meta-analyses looking at taxane-based regimens or anthracycline-based regimens (doxorubicin is an anthracycline), the proportional reductions in early recurrence, any recurrence, and breast cancer mortality were more or less independent of age, nodal status, tumor size, or even estrogen receptor status.
The authors conclude:
While awaiting the results of these new trials, it appears that ER status, differentiation, and the other tumour characteristics available for the present meta-analyses had little effect on the proportional risk reductions with taxane-based or anthracycline-based regimens. The more effective of these regimens offer on average a one-third reduction in 10-year breast cancer mortality, roughly independently of the available characteristics. The absolute gain from a one-third breast cancer mortality reduction depends, however, on the absolute risks without chemotherapy (which, for ER-positive disease, are the risks remaining with appropriate endocrine therapy). Although nodal status and tumour diameter and differentiation are of little relevance to the proportional risk reductions produced by such chemotherapy (and by tamoxifen therapy), they can help in treatment decisions as they are strongly predictive of the absolute risk without chemotherapy, and hence of the absolute benefit that would be obtained by a one-third reduction in that risk.
The bottom line is that, contrary to what you will hear from cranks and alt-med supporters who believe in “alternative” cancer cures, in the case of early stage breast cancer, chemotherapy saves lives. In women with breast cancer, it decreases the risk of their dying from breast cancer by approximately one-third. This is nothing to sneeze at, as it means thousands upon thousands of women who would have died but did not, thanks to chemotherapy. This study simply represents yet another in a long line of studies, another strand in the web of evidence that support the efficacy of chemotherapy in prolonging the lives of women with breast cancer. It’s not perfect, and it has a lot of potential complications, but it works. This is but one example.
Indeed, as DeVita points out, besides its well-demonstrated role in treating hematological malignancies, chemotherapy now has a role in the primary treatment of advanced malignancies such as bladder cancer, breast cancer, cervical cancer, colorectal cancer, esophageal cancer, gastric cancer, head and neck cancer, nasopharyngeal cancer, non-small cell lung cancer, ovarian cancer, pancreatic cancer, and prostate cancer. It’s also used to prolong survival in the adjuvant setting for breast cancer, colorectal cancer, cervical cancer, gastric cancer, head and neck cancer, pancreas cancer, melanoma, non-small cell lung cancer, osteogenic sarcoma, and ovarian cancer. I must admit, though, I’m a bit surprised that other soft tissue sarcomas weren’t included on the list.
Chemotherapy and cancer
I’m no Pollyanna, as I’m sure regular readers realize. You just have to read my posts over the years about screening for cancer or how little better newer drugs seem to be than old drugs used to treat cancer to see that. I realize that chemotherapy is imperfect and doesn’t work well for a lot of cancers. Many of the drugs cause bad side effects, and, as I’ve explained before, in the adjuvant setting you have to treat a lot of patients to benefit relatively few. I also realize that chemotherapy is sometimes oversold. At the same time, I also know that now is the best time there has ever been for treating cancer with drugs. Targeted agents allow us to attack more precisely the molecular derangements driving cancer growth with lower toxicity. Molecular profiling is paving the way for precision medicine, in which someday (or so we hope) we will be able to target treatments to the specific abnormalities in a specific patient’s tumor. Certainly, I have no illusion of how difficult this is to accomplish, but I do believe that over time we will find ways to do it.
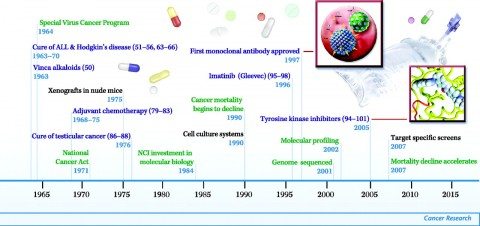
It’s helpful to look at the scope of advances over the last 100 years or so, as provided in these helpful diagrams in DeVita’s article:
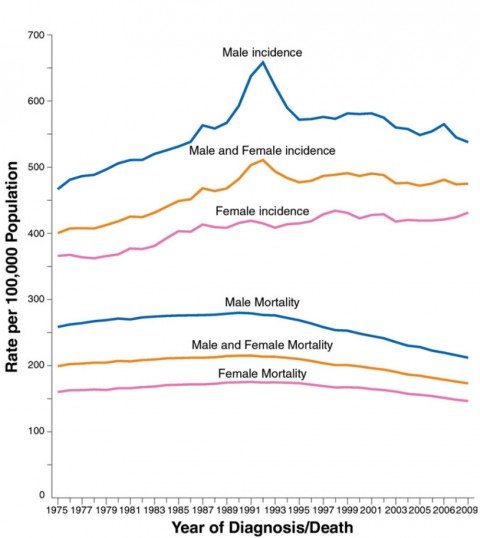
As slow as it seems to those of us living it, cancer research has produced a lot of breakthroughs. Those who wonder why we haven’t cured “cancer” yet should read earlier posts I’ve written on the topic. Cancer is hard. Real hard. It is also hundreds of diseases, not some monolithic disease, just as chemotherapy is dozens of drugs and hundreds of drug combinations, not some monolithic mythical “chemotherapy.” It is not reasonable to expect that a span of a mere few decades or even a century is enough to cure all cancer. We have, however, brought the cure of several cancers within reach and do actually cure many cancers. Also, contrary to popular belief, the death rate from cancer is decreasing. In the US, it’s been decreasing for nearly the last 25 years, as shown in this graph from the most recent American Cancer Society statistics:
Note that this is happening even as the age-adjusted incidence of cancer is remaining steady or slightly increasing. Fewer and fewer people with cancer die of their disease. I realize that this is no consolation to anyone who has lost loved ones to the disease (as I have), but it does give hope for the future.
And, yes, promoters of alternative cancer cures can deny it all they like, but chemotherapy is indeed a major part of the reason for better outcomes and more hope in cancer. “Cut, poison, burn”? Well, yes. Unfortunately, that’s what works, including the “poison” part. Until we find something that works without as much morbidity, “cut, poison, burn” will have to do.
That reminds me. I really need to review the movie of the same title.