“CHEMOTHERAPY DOESN’T WORK!!!!!”
“CHEMOTHERAPY IS POISON!!!!”
“CHEMOTHERAPY WILL KILL YOU!!!!”
I’ve lost count of how many times I’ve come across statements like the ones above, often in all caps, quite frequently with more than one exclamation point, on the websites of “natural healers,” purveyors of “alternative medicine.” In fact, if you Google “chemotherapy doesn’t work,” “chemotherapy is poison,” or “chemotherapy kills,” you’ll get thousands upon thousands of hits. In the case of “chemotherapy kills,” Google will even start autofilling it to read “chemotherapy kills more than it saves.” The vast majority of the hits from these searches usually come from websites hostile to science-based medicine. Examples include Mercola.com, the website of “alternative medicine entrepreneur” Dr. Joe Mercola and NaturalNews.com, the website of Mike Adams, where you will find cartoons like this one, which likens the administration of chemotherapy to a Nazi death camp:
Here’s another example, entitled The truth about chemotherapy and the cancer industry:
Note how Adams portrays screening for cancer and chemotherapy as a deadly scam designed solely to enrich the “cancer industry” as it kills patients.
As my final example, there’s this cartoon:
An article by Mike Adams entitled Chemotherapy Stickup that accompanies the cartoon above makes this astounding claim:
There is not a single cancer patient that has ever been cured by chemotherapy. Zero. They don’t exist. Not a single documented case in the history of western medicine.
And why is that? Because conventional medicine operates from the false belief that there is no cure for cancer! Thus, anyone offering a cure (or assisting in the body’s own natural reversal of the disease) is immediately dismissed as a quack. Meanwhile, the real quackery is found in the pushing of toxic chemotherapy chemicals that are injected into the bodies of patients and called “treatment” when they should really be called “torture.” (Nancy Pelosi, by the way, was never briefed on the fact that chemotherapy is torture…)
When I first encountered that cartoon a few years ago, I was a bit surprised that even Mike Adams would go so far as to make such an absolutist statement that not a single person has ever been cured of cancer by chemotherapy in the entire history of “western medicine.” All it would take is a single example to prove him wrong, like—oh, you know—Lance Armstrong, the patients cared for by my pediatric oncology colleagues, or the patients I saw during my training cured of anal cancer by the Nigro protocol. The Nigro protocol, by the way, consists of combined chemotherapy and radiation and is still the standard of care for anal cancer. That doesn’t even count all the patients with leukemia or lymphoma cured primarily by chemotherapy.
Unfortunately, this attitude isn’t just limited to cranks. There are legitimate scientists, even those who have published in magazines devoted to skepticism, who make very similar statements, although perhaps not quite as absolutist. Not quite, but close. For example, there’s Reynold Spector, whom Mark Crislip and I took to task for his article earlier this year in Skeptical Inquirer entitled Seven Deadly Medical Hypotheses. One of his “seven deadly medical hypotheses” read thusly:
From a cancer patient population and public health perspective, cancer chemotherapy (chemo) has been a major medical advance.
In other words, to Dr. Spector, the very idea that chemotherapy is a notable advance in the treatment of cancer is a “deadly medical hypothesis.” Of course, his statement is not a hypothesis at all, deadly or otherwise, as what one means by a “major medical advance” is very subjective (Dr. Spector really needs to get himself hence to a medical dictionary) and the weasel words of “from a patient population and public health perspective” give Dr. Spector wiggle room, but it’s very clear what his intent is. He doesn’t think chemotherapy works very well, if at all, even as he admits:
However, it cannot be denied that there are a few populations for which chemotherapy is marvelously effective, as noted above, and must be used.
So which is it?
In previous posts, such as Why haven’t we cured cancer yet? and Skepticism versus nihilism about cancer in science-based medicine, I explored some of these questions. In the former article, I pointed out just how complex the problem is, with cancer being hundreds of different diseases and using the example of just how messed up the prostate cancer genome is to provide an idea of the magnitude of the problem. In the second article, I pointed out an example of a specific cancer for which advances in chemotherapy have made a meaningful difference in both survival and quality of life outcomes. What I haven’t yet done is to look at the arguments cancer cranks use to try to convince people that chemotherapy doesn’t work.
Attacking chemotherapy
Any rational assessment of the efficacy of chemotherapy must be forced to include an admission that chemotherapy is only rarely curative in solid malignancies, particularly advanced solid malignancies. Notable exceptions include testicular cancer (which is what Lance Armstrong was cured of) and anal cancer. In contrast, for hematological malignancies, such as leukemia and lymphoma, chemotherapy is usually the mainstay of therapy. However, not being curative doesn’t mean that chemotherapy is useless anymore than the fact that beta blockers don’t cure hypertension and metformin doesn’t cure diabetes makes them “useless” drugs. Before we take a rational look at what chemotherapy can and can’t do, let me just point out that there are three studies that are frequently used by cranks to try to argue that chemotherapy is useless.
The first one is easily dismissed, but you’ll see it a lot anyway. It’s frequently cited in articles with titles like 75% of MDs Refuse Chemotherapy Themselves and the claim will go something like this:
Several full-time scientists at the McGill Cancer Center sent to 118 doctors, all experts on lung cancer, a questionnaire to determine the level of trust they had in the therapies they were applying; they were asked to imagine that they themselves had contracted the disease and which of the six current experimental therapies they would choose. 79 doctors answered, 64 of them said that they would not consent to undergo any treatment containing cis-platinum – one of the common chemotherapy drugs they used – while 58 out of 79 believed that all the experimental therapies above were not accepted because of the ineffectiveness and the elevated level of toxicity of chemotherapy. (Source: Philip Day, “Cancer: Why we’re still dying to know the truth”, Credence Publications, 2000)
Wow! This sounds really damning, doesn’t it? What hypocrites those oncologists are! Right?
It turns out that this survey is over 25 years old and was about a specific kind of chemotherapy, cisplatin for non-small cell lung cancer, which was a new therapy at the time and didn’t have a lot of evidence for it. As Anaximperator describes, a followup survey was conducted in 1997 at a session on the National Comprehensive Cancer Network (NCCN) clinical practice guidelines. Participants were asked to respond to the same question regarding chemotherapy:
You are a 60-year-old oncologist with non-small-cell lung cancer, one liver metastasis, and bone metastases.
Your performance status is 1. Would you take chemotherapy? Yes or no?
The results? Let Anaximperator tell the tale:
The overall results of the 1997 follow-up survey show that 64.5% would now take chemotherapy – which is almost a doubling from 34% to 64.5% of those willing to have chemotherapy and radiotherapy and a quadrupling from 17% to 64.5% of those who would take chemotherapy alone.
Anaximperator adds:
The study from 1991, “Oncologists vary in their willingness to undertake anti-cancer therapies,” pertains to many kinds of cancer and cancer stages, from early stage to terminal, as well as to experimental therapies. It shows percentages as high as 98% of doctors willing to undergo chemotherapy, while the remaining 2 % were uncertain, and none answered “definitely no” or “probably no” to chemotherapy.
Should another survey be conducted today, there’s a good chance the results would be even higher in favour of chemotherapy, given that over the years chemotherapy has shown enhanced clinical benefit and less side effects.
Indeed. One should also note that this question was constructed such that the clinical presentation of the cancer was incurable. Participants were presented with a scenario in which they are diagnosed with stage IV metastatic disease, a situation where opting for palliative care rather than aggressive treatment often makes sense, which makes the results even more striking. Also, I know from personal experience that it is not true that oncologists tend to turn down chemotherapy, even for advanced disease. having known oncologists who developed various cancers and underwent standard-of-care chemotherapy. Indeed, just this week, I was saddened to learn that an oncologist I used to know at my old job recently developed cancer and is currently undergoing chemotherapy. He’s also lost all his hair, just like many of his patients. In the end, this particular ploy serves two purposes. First, it implies that oncologists are hypocrites who don’t believe that the treatments they are giving patients are worthwhile. Second, it feeds into the conspiracy theories beloved of quacks with the implication that oncologists are hiding something about chemotherapy effectiveness. They’re not.
My favorite example of the use of the next study beloved of anti-chemotherapy cranks is by Andreas Moritz, who describes himself as “a medical intuitive; a practitioner of Ayurveda, iridology, shiatsu, and vibrational medicine; a writer; and an artist.” The article is entitled Can you trust chemotherapy to cure your cancer? and in it Moritz cites a study from Australia published in 2004:
An investigation by the Department of Radiation Oncology, Northern Sydney Cancer Centre, Australia, into the contribution of chemotherapy to 5-year survival in 22 major adult malignancies, showed startling results: The overall contribution of curative and adjuvant cytotoxic chemotherapy to 5-year survival in adults was estimated to be 2.3% in Australia and 2.1% in the USA.” [Royal North Shore Hospital Clin Oncol (R Coll Radiol) 2005 Jun;17(4):294.]
The research covered data from the Cancer Registry in Australia and the Surveillance Epidemiology and End Results in the USA for the year 1998. The current 5-year relative adult survival rate for cancer in Australia is over 60%, and no less than that in the USA. By comparison, a mere 2.3% contribution of chemotherapy to cancer survival does not justify the massive expense involved and the tremendous suffering patients experience because of severe, toxic side effects resulting from this treatment. With a meager success rate of 2.3%, selling chemotherapy as a medical treatment (instead of a scam), is one of the greatest fraudulent acts ever committed. The average chemotherapy earns the medical establishment a whopping $300,000 to $1,000,000 each year, and has so far earned those who promote this pseudo-medication (poison) over 1 trillion dollars. It’s no surprise that the medical establishment tries to keep this scam alive for as long as possible.
Here is the study to which Moritz refers and which is the origin of the claim that “chemotherapy only provides 2% benefit,” a favorite talking point used by cancer quacks. I’ve seen it on websites ranging from Moritz’s website to NaturalNews.com, to Mercola.com, to Whale.to (my favorite), to I forget how many others. Always it’s the same thing, a variant of a statement claiming that chemotherapy only contributes 2% to five year survival in adult malignancies, followed by conspiracy-mongering of the sort above in which chemotherapy is portrayed as a huge scam designed to enrich big pharma. Indeed, so common is this particular favorite that I proclaim it “The 2% Gambit.” It turns out that this is not such an impressive study. Indeed, it appears almost intentionally designed to have left out the very types of cancers for which chemotherapy provides the most benefit, and it uses 5 year survival exclusively, completely neglecting that in some common cancers (such as breast cancer) chemotherapy can prevent late relapses. There were also a lot of inconsistencies and omissions in that leukemias were not included, while leukemia is one type of cancer against which chemotherapy is most efficacious. Indeed, the very technique of lumping all newly diagnosed adult cancers together is guaranteed to obscure benefits of chemotherapy among subgroups by lumping in patients for whom chemotherapy is not even indicated. A letter to the editor listed these problems and several really egregious errors and omissions, too:
The authors omitted leukaemias, which they curiously justify in part by citing the fact that it is usually treated by clinical haematologists rather than medical oncologists. They also wrongly state that only intermediate and high-grade non-Hodgkin’s lymphoma of large-B cell type can be cured with chemotherapy, and ignore T-cell lymphomas and the highly curable Burkitt’s lymphoma. They neglect to mention the significant survival benefit achievable with high-dose chemotherapy and autologous stem-cell transplantation to treat newly-diagnosed multiple myeloma [4]. In ovarian cancer, they quote a survival benefit from chemotherapy of 11% at 5 years, based on a single randomised-controlled trial (RCT), in which chemotherapy was given in both arms [5]; however, subsequent trials have reported higher 5-year survival rates. In cancers such as myeloma and ovarian cancer, in which chemotherapy has been used long before our current era of well-designed RCTs, the lack of RCT comparing chemotherapy to best supportive care should not be misconstrued to dismiss or minimise any survival benefit. In head and neck cancer, the authors erroneously claim the benefit from chemotherapy given concomitantly with radiotherapy in a meta-analysis to be 4%, when 8% was in fact reported [6].
The authors do not address the important benefits from chemotherapy to treat advanced cancer. Many patients with cancers such as lung and colon present or relapse with advanced incurable disease. For these conditions, chemotherapy significantly improves median survival rates, and may also improve quality of life by reducing symptoms and complications of cancer.
Of course, those using this particular gambit almost invariably never include the criticism of this particular article. Another aspect of this particular study that always bothered me is that it appeared to lump patients undergoing adjuvant chemotherapy in with those undergoing chemotherapy for cure or palliation. Adjuvant chemotherapy is given after surgery in order to decrease the rate of recurrence, but the truly curative modality is the surgery itself. In early stage cancer, the absolute benefit of chemotherapy in terms of prolonging survival tends to be modest, often single digit percentages. Lumping adjuvant therapy in with other uses of chemotherapy again appears custom-designed to minimize the survival benefit due to chemotherapy observed.
The second study frequently cited by cancer quacks as evidence that “chemotherapy doesn’t work” is, not surprisingly, also cited by Moritz:
In 1990, the highly respected German epidemiologist, Dr. Ulrich Abel from the Tumor Clinic of the University of Heidelberg, conducted the most comprehensive investigation of every major clinical study on chemotherapy drugs ever done. Abel contacted 350 medical centers and asked them to send him anything they had ever published on chemotherapy. He also reviewed and analyzed thousands of scientific articles published in the most prestigious medical journals. It took Abel several years to collect and evaluate the data. Abel’s epidemiological study, which was published on August 10, 1991 in The Lancet, should have alerted every doctor and cancer patient about the risks of one of the most common treatments used for cancer and other diseases. In his paper, Abel came to the conclusion that the overall success rate of chemotherapy was “appalling.” According to this report, there was no scientific evidence available in any existing study to show that chemotherapy can “extend in any appreciable way the lives of patients suffering from the most common organic cancers.”
I looked for this study. In fact, I went to The Lancet’s website and looked up the August 10, 1991 issue. I could find no study by Ulrich Abel or anything about chemotherapy other than this study on stroke after chemotherapy for testicular cancer. So I went to PubMed and searched on Ulrich Abel’s name for 1991. All I could find were two articles, one on common infections in chemotherapy patients and another on Crohn’s disease. Nor was I the only blogger who couldn’t find this ethereal Lancet paper by Dr. Abel. So I started searching other years, and then I found what appears to be the paper to which Moritz referred, only it wasn’t published in 1991 but rather in 1992 and it wasn’t published in The Lancet but rather in Biomedicine & Pharmacotherapy, a much lower tier journal. Somehow, through the magic of playing “telephone” over the Internet, this article has morphed from being in a lower tier journal to having been in The Lancet—even published on a specific date!
It turns out that the Dr. Abel’s article is rather odd. It’s not really a study, and it’s definitely not a meta-analysis. Nor is it really a particularly good systematic review, given that the methodology of selecting papers isn’t exactly transparent, and the larger “review” to which he refers readers appears to be in German and not readily available on the web, as far as I can tell. In the abstract, Dr. Abel states that “as a result of the analysis and the comments received from hundreds of oncologists in reply to a request for information, the following facts can be noted.” More importantly, Dr. Abel was addressing a fairly limited situation that excludes two of the most effective uses of chemotherapy, as described in this English translation of a Der Spiegel article describing his work:
- Abel’s verdict against the medicinal treatment of cancer is emphatically untrue for various kinds of lymph cancer, Hodgkin’s disease, leukemias, sarcomas, and testicular cancers in the male. These kinds of malignancies can be cured by chemotherapy with a high degree of probability, especially in children — an undisputed success. But these are, in any case, only a very small part of the new cases of cancer diagnosed every year.
- Abel’s doubts are not directed against chemotherapy when it is used in support of a curative operation, in order to shrink the tumor beforehand; nor do they apply to chemotherapy used prophylactically after an operation, to prevent a relapse (as an adjuvant).
These are, of course, the two most effective uses of chemotherapy that there are. I’ll grant critics that the types of tumors that can be cured with chemotherapy with a high degree of probability are a minority of tumors, but, contrary to what is implied in many uses of Dr. Abel’s work, they are not insignificant. For example, leukemias and lymphomas (Hodgkins and non-Hodgkins) add up to almost 10% of newly diagnosed cancers every year, and they are cured primarily with chemotherapy. Sarcomas and testicular cancers are much less common, but add them in and the total exceeds 10%. A distinct minority, yes, but the fact that many of these cancers can be cured with chemotherapy puts the lie to statements like the one by Mike Adams quoted above, which, not surprisingly, is parroted in Andreas Moritz’s little screed.
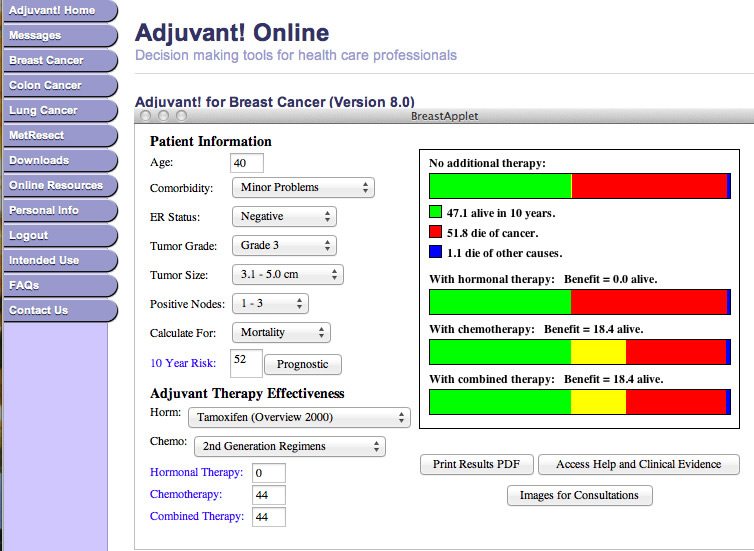
The second indication left out of Dr. Abel’s analysis, adjuvant chemotherapy, can, depending on the circumstance and tumor, be highly effective. Admittedly in early stage breast cancer adjuvant chemotherapy adds on an absolute basis only low single digit percentages to five and ten year survivals, but in more locally advanced breast cancer, particularly so-called “triple negative” breast cancer, the benefit is much more substantial. For instance, using Adjuvant Online, it’s possible to use the latest literature to estimate the benefit of chemotherapy in specific clinical situations. Here’s an example of a hypothetical 40 year old woman with an estrogen receptor negative tumor measuring between 3 and 5 cm with 1-3 axillary lymph nodes positive for metastatic disease:
Note that standard chemotherapy increases this woman’s chance of survival by 18% on an absolute basis and by 35% on a relative basis. Either way, the survival benefit is substantial. These are women who otherwise would have died but did not, thanks to chemotherapy. These women could be your mother, your wife, your sister, or even your daughter. The bottom line is that, even though I wasn’t particularly impressed with his methodology, Dr. Abel was actually reasonably nuanced in his discussion in that he discussed overdiagnosis and stage migration as confounders that can make a treatment seem more effective than it is, as I myself have discussed many times on this blog, starting with this post.
Besides, few oncologists would disagree with this statement at the end of Dr. Abel’s abstract, “With few exceptions, there is no good scientific basis for the application of chemotherapy in symptom-free patients with advanced epithelial malignancy.” And, indeed, most oncologists do not recommend chemotherapy for patients with stage IV epithelial malignancies who are asymptomatic, because at that point all treatment is palliative, and you can’t palliate symptoms that don’t exist. That’s why chemotherapy is, in most cases, reserved for when tumor progression leads to symptoms. Moreover, this study only examined epithelial malignancies. These are cancers for which surgery can be curative if the tumor has not metastasized. Since 1991, also, we have made significant advances in improving survival using chemotherapy. I’ve used the example of colorectal cancer before, where, thanks to newer and better chemotherapy regimens developed over the last couple of decades that have improved survival in patients with liver metastases from 6 months to close to two years.
I also note that since 1992, Dr. Abel has been co-author on a number of studies involving chemotherapy, for instance, a trial in nephroblastoma and a clinical trial of high dose chemotherapy in aggressive lymphoma. As recently as 2009, Dr. Abel was co-author on a randomized multicenter study comparing two different chemotherapy regimens in pancreatic cancer. Yes, pancreatic cancer, that most intractable of cancer problems with a five-year survival rate of only around 20% in the most favorable cases; i.e., the ones that can be completely resected surgically. Clearly, Dr. Abel buys into the evil big pharma propaganda that chemotherapy can cure at least some forms of cancer and, as far as I can tell, has never written a followup to his 1992 paper.
The bottom line is that the “evidence” used by cranks and quacks to prove that “chemotherapy doesn’t work” is most often based on intellectually dishonest tactics. They either misrepresent studies, as they frequently do with the McGill study claiming that oncologists won’t use chemotherapy. True, thanks to the way these studies have been misrepresented over the years, many of these quacks probably honestly think they’re accurately representing them, but that just goes to show how lazy they are about going back to the primary sources to back up their claims. As for the rest, the Australian study was custom-designed to minimize the apparent utility of chemotherapy, while Dr. Abel’s study intentionally left out the types of situations where chemotherapy is most useful and looked at primarily advanced malignancies. In this latter case, there’s nothing wrong with that approach; the problem comes when the quacks either intentionally or unintentionally fail to disclose that qualification, lose any hint at nuance, and use the results to imply that chemotherapy doesn’t work for anything.
Framing the question
Considering the question of whether chemotherapy “works” or not is very similar to asking the question, “Why haven’t we cured cancer yet?” The reason is that it’s a question that’s so vague as to be almost meaningless. Cancer is, as I have pointed out, hundreds of diseases, each driven by a plethora of different combinations of disruptions in cell growth control mechanisms. A more appropriate question is whether we’ve cured this cancer or that cancer, not whether we’ve cured cancer. Similarly, asking the question of whether chemotherapy “works” is similarly vague and meaningless. The real questions are (1) whether this specific chemotherapy regimen “works” for this cancer, although there are some examples that in aggregate we can make some conclusions about and (2) whether specific chemotherapy regimens can cure specific cancers. As noted above, even some “skeptics” of chemotherapy admit that chemotherapy can be “marvelously effective” for some cancers; the argument that usually follows is that the cancers for which chemotherapy is effective are so few as not to matter. The other issue is that few cancers are treated only with chemotherapy. Multidisciplinary and multimodality therapy are more the rule than the exception, particularly for solid malignancies and includes chemotherapy, radiation therapy, surgery, hormonal therapy, and a variety of other less common therapies.
What needs to be understood is that chemotherapy is very good for some things. For instance, it’s very good for treating and curing leukemias and lymphomas. For certain cancers, it’s also very good at decreasing the chance of relapse after curative surgery. When given before curative surgery, chemotherapy can also make organ-preserving surgery possible. Prominent examples include using neoadjuvant chemotherapy (chemotherapy before surgery) to shrink breast cancers so that they can be removed without mastectomy and shrinking rectal cancers so that sphincter-sparing surgery is possible (i.e., surgery that leaves the anal sphincter intact and thereby spares the patient having to have a permanent colostomy). For specific tumors, chemotherapy has also contributed to significant increases in survival, but it is not a panacea. For example, chemotherapy usually does very little for pancreatic cancer, and metastatic melanoma laughs at most chemotherapy (although there are newer agents that provide hope that this will no longer be the case). For all its uses and advantages, chemotherapy alone is not very good at prolonging survival in advanced epithelial malignancies, and it’s not at all unreasonable to ask whether it is overused in such patients, who are, for the most part, currently incurable.
This reasonable skepticism devolves into nihilism or crankery, however, when tactics such as those used by Mike Adams, Andreas Moritz, or, yes, even the esteemed Reynold Spector are used to “prove” that chemotherapy is “useless.” Moreover, such “skepticism” completely dismisses as worthless survival benefits of a few months, which certainly aren’t “worthless” to many patients. Such briefly lengthened survival times can mean the difference between seeing a child graduate from college or not, seeing a child get married or not, or seeing the birth of a grandchild or not. It must also be remembered that the measured improvements in survival due to chemotherapy are usually medians. Not uncommonly, buried in that median are “outliers” who derive a huge survival benefit from the chemotherapy and survive many more months than expected, sometimes many more years than expected. Moreover, it does patients no favor to try to use the observation that chemotherapy has at best relatively modest benefits in patients with advanced epithelial malignancies to try to imply that chemotherapy doesn’t work for all patients. In particular, patients have to remember that just because chemotherapy doesn’t do that well against advanced malignancies does not, as the quacks would have you believe, imply that “alternative medicine” can do better.