I’m one of those odd people that enjoys distance running. I end up spending a lot of time in the company of other runners. And when we’re not running, we’re usually griping about our running injuries. As the cohort that I run with ages, the injuries are getting more prevalent. Besides the acute conditions, the chronic problems are starting to appear. Our osteoarthritis years are here.
As the available pharmacist, I get a lot of questions about joint pain. What’s reassuring, I tell them, is that they shouldn’t blame running. Osteoarthritis is common — the most frequent cause of joint pain. For some, it starts in our twenties, and by our seventies, osteoarthritis is virtually certain. Regardless of your level of exercise, the passage of time means the classic osteoarthritis symptoms — joint pain and morning stiffness, that worsens over time.
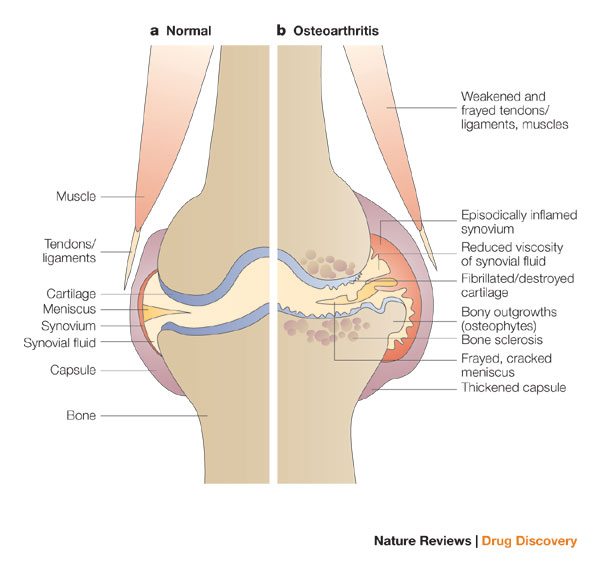
Osteoarthritis progresses gradually. Blame biomechanics and biochemistry. It starts with a breakdown of the cartilage matrix. Stage 2 progresses to erosion of the cartilage and a release of collagen fragments. Stage 3 is a chronic inflammatory response. The goals of treatment are to reduce inflammation and pain, and stop progressive disease. There’s no drug therapy that’s been show to actually improve joint function. Reduce pain, or slow inflammation, yes. Analgesics, like Tylenol, and anti-inflammatories are mainstays. But repair damage? Sorry: you lose it, it’s gone. Chondrocytes don’t seem to be able to repair the overall matrix — which is made mainly of collagen.
I don’t advise people with joint pain and morning stiffness to stop running. (It’s futile to suggest this to a runner, anyway.) The idea you can “wear out” your joints is is a popular image, but it’s inaccurate. In most cases exercise can continue — exercise doesn’t seem to accelerate the rate of osteoarthritis development. When the pain is persistent, I’ll suggest a physician evaluation, and describe some non-drug and non-prescription approaches to symptom management that might be appropriate.
I’m prepared now, for the inevitable question that follows: “But what about supplements? What do you think of X?” Glucosamine is a common inquiry (discussed at length here) as is chondroitin (which it is often co-packaged with). As with most supplements, their popularity is not related to good clinical evidence. Rather it seems to be secondary to perceptions of efficacy, driven by lots of anecdotes and general awareness. But the message that it’s ineffective may be getting out — I’m getting fewer inquiries about it these days. The market has shifted, and there are new products on the shelves for those with sore joints.
The latest supplement trend for joint pain may be collagen. Collagen supplements have been around for years, and their traditional popularity has been its purported effects on skin and nails. There are regional trends, with collagen-rich foods and even restaurants gaining popularity in Japan. (Anyone want a meal of pig’s feet?) The enthusiasm for collagen is now being more actively tapped for the arthritis market – perhaps it’s a way to drive demand among all ages.
Genacol, a collagen supplement, is currently being actively marketed here in Toronto, and seemingly distributed worldwide. This particular brand caught my attention not just because I see the giant image of Indy care driver and spokesperson Alex Tagliani) everywhere, but because of an explicit efficacy claim made in the advertisements and on the website: “Scientifically proven to reduce joint pain.” There’s no other supplement with convincing evidence for any type joint pain. So I went looking for the proof.
Why collagen, and what does it have to do with our joints? Collagen is the major component of connective tissue in the body — it’s about a quarter of our body mass, and is found in skin, muscle, tendons, etc. Hence the pig’s feet. All animals are mainly collagen: it’s the most abundant protein in the animal kingdom. Your leather coat? Think of it as a collagen coat. In fact, that’s where your Genacol is coming from: the collagen source for this particular supplement is European bovine skin collagen.
If we don’t have enough collagen, we’re in big trouble. There’s several different types in the body, each with their own role. Remember that M. Night Shyamalan movie Unbreakable with Bruce Willis and Samuel L. Jackson? Jackson’s character had Lobstein syndrome (osteogenesis imperfecta), a congenital disease that results in the failure to produce type 1 collagen, which results in exceptionally brittle bones.
Or think of scurvy — now rare, but once the worst thing about extended sea voyages. Vitamin C is a necessary cofactor for collagen synthesis. Without it, multiple systems are affected, and biological disaster ensues, starting with your teeth falling out. History’s first clinical trial was performed by James Lind, a British Royal Navy physician, to compare a variety of scurvy cures, including the one that worked: fresh lemons.
Both scurvy and Lobstein’s are basically collagen shortage diseases. But, interestingly, guess what doesn’t work for either scurvy or Lobstein’s? Eating collagen. That’s because collagen is a protein: a triple-helix, long chain protein. It’s the product of an elaborate synthesis process that occurs throughout the body. When we consume collagen, usually in the form of food, the long chain proteins are broken down during digestion to their original amino acids. Only then can they be absorbed. Once absorbed, these amino acids are available as building blocks to support collagen synthesis throughout the body. So from a dietary perspective, your body doesn’t care (and can’t tell) if you ate a collagen supplement, cheese, quinoa, beef, or chick peas — they’re all sources of protein, and indistinguishable by the time they hit the bloodstream. The body doesn’t treat amino acids derived from collagen any differently than any other protein source. For this reason, the idea that collagen supplementation can be an effective treatment for joint pain, osteoarthritis, or any other condition, is highly implausible, if not impossible in principle.
But about that proof …
The company links to a press release with its scientific evidence for Genacol. Two clinical trials are described. A search of PubMed reveals neither have been published. That doesn’t prevent the efficacy claims:
With Genacol, a “statistically significant” beneficial effect with relation to pain was observed in the subjects: the best result that can be obtained during a clinical trial. “These two new trials demonstrate without a doubt that millions of people suffer less with Genacol, proving the impeccable quality of the products under this brand,” says Guy Michaud, President of Groupe Genacol.
Not quite. Setting aside the grandiose claims, statistical significance isn’t enough — we want clinical significance. A tiny change in pain may be enough to be statistically significant — but is it relevant in the real world? We only have the abstracts, so the information is incomplete. However, as a general rule, if study authors don’t mention effect size in the abstract, it’s probably because they are not worth mentioning.
The first trial, A 6-month randomised, double-blind, placebo controlled study to assess the clinical benefit of a food supplement made of a proprietary collagen hydrolysate in subjects with joint pain at the lower or upper limbs or at the lumbar spine randomized 200 patients to 1200mg of collagen daily, or placebo. The results don’t sound promising:
At 6 months, the proportion of clinical responders to the treatment, according to VAS scores, was significantly higher in the collagen hydrolysate (CH) group 51.6%, compared to the placebo group 36.5% (p<0.05) , .[sic] However, even if there was no significant difference in the number of clinical responders at 3 months (44.1% vs 39.6%, p=0.53), there was still a higher proportion of responder in the group using collagen hydrolysate demonstrating a certain evolution. Using other pain and function assessment tools (i.e. questionnaires Lequesne, DASH or EIFEL) no significant effect of collagen hydrolysate was observed compared to placebo.
The second trial is also lacking in information. A randomized controlled trial on the efficacy of oral collagen treatment on the medial knee joint space and functional outcome among veterans memorial medical center patients diagnosed with osteoarthritis of the knee: open label and single blind (the blinding is not described) this trial randomized 150 patients, with 113 completing the trial. Right away, that many patient dropouts is a massive red flag, as patients that drop out usually are not responding to treatment. Patients were randomized to collagen, 1200mg per day, or the anti-inflammatory aclofenac (which I’ve never heard of) 100mg daily for five days, then as required. Both groups could use ketoprofen gel as desired. The results?
Patients in Group A significantly scored lower in the average WOMAC score from baseline to the sixth month follow up. On the other hand, patients in Group B had no significant change in their average WOMAC score after six months. There was no significant difference in the medial knee joint space measured at baseline and after six months in both groups.
There’s no additional data, so there’s no way to determine if the groups were properly matched, or if the effect observed was both real and clinically meaningful. Given the trial was single-blind, the risk of bias is large. Perhaps not surprisingly, when objective measurements (joint spaces) were taken, there were no differences between the groups.
It could be that collagen supplements provide a meaningful clinical benefit to arthritis and joint pain, but there’s certainly no persuasive evidence to suggest that’s the case. Based on what collagen is, how it’s absorbed, and how we know collagen is actually synthesized in the body, it’s highly implausible that 1200mg of additional protein consumed daily will have any meaningful therapeutic effects. Genacol, like other collagen supplements, appears to be little more than an expensive protein supplement. If you want to supplement with collagen, my suggestion is to skip the supplements, and go for a well-marbled steak. Enjoy it, but don’t expect the steak, or any collagen supplement, to relieve your joint pain.
