 Most people know about hepatitis B; babies get vaccinated for it at birth. But fewer people know about hepatitis C. C is actually more common than B, but most chronically infected people don’t know they have it. You might think ignorance is bliss, but patients who have no symptoms today may have liver cancer or a liver transplant in their future. Until recently, treatment for this stealth disease was disappointing, but according to three recent, large controlled studies published in The New England Journal of Medicine, the virus has been tamed. A short course of a new antiviral drug with few side effects was 99% effective in removing the virus from the blood.
Most people know about hepatitis B; babies get vaccinated for it at birth. But fewer people know about hepatitis C. C is actually more common than B, but most chronically infected people don’t know they have it. You might think ignorance is bliss, but patients who have no symptoms today may have liver cancer or a liver transplant in their future. Until recently, treatment for this stealth disease was disappointing, but according to three recent, large controlled studies published in The New England Journal of Medicine, the virus has been tamed. A short course of a new antiviral drug with few side effects was 99% effective in removing the virus from the blood.
History
In the beginning, there was jaundice. Patients turned yellow, developed flu-like symptoms, and sometimes died. Eventually doctors figured out that jaundice was a sign of liver disease and the condition was named hepatitis; and by the time I graduated from medical school in 1970, scientists had identified two viruses that caused infectious hepatitis: hepatitis A and B. Hepatitis A infection was transmitted by the fecal-oral route, usually by contamination of food; hepatitis B was transmitted by needles and blood products. Prevention was limited to good hygienic practices; treatment of acute hepatitis was limited to bed rest, supportive care, and IV fluids. Contacts could be given gamma globulin. In fulminant cases and chronic hepatitis, steroids were used. No treatment was very effective. Death and cirrhosis often ensued.
Non-C hepatitis today
Fast forward to 2014. Scientists have identified five hepatitis viruses: A, B, C, D, and E, along with numerous serotypes and genotypes. Antigen and antibody tests are available for accurate diagnosis.
Hepatitis A still infects 1.4 million people and kills around 100,000 people around the world every year. There is still no specific treatment available. A vaccine is available, but hygiene, sanitation, and food safety precautions are the mainstays of prevention.
Hepatitis B has infected about a third of the world’s inhabitants, and an estimated 350 million people are chronic carriers. The disease is transmitted through blood, sexual intercourse, semen, saliva, and childbirth. Chronic disease can lead to cirrhosis and causes about half of all liver cancers. The virus was first seen with an electron microscope in 1970, and by the early 1980s its genome had been sequenced. By 1991 an effective vaccine was being recommended for all infants at birth. Early vaccination is important because young children are particularly vulnerable. Only 5% of newborns infected by their mother will clear the infection, and they have a 40% lifetime risk of cirrhosis and liver cancer. Acute infection in older children and adults usually clears spontaneously, but treatment of chronic infection is necessary to prevent cirrhosis and liver cancer. Five antiviral drugs and two immune system modulators (interferons) are available; they don’t cure the infection but they reduce replication and liver damage.
Hepatitis D occurs only in those also infected with HBV, and it increases the risk of complications.
Hepatitis E infects 20 million people a year and causes 57,000 deaths. It’s more common in developing countries, and there are animal reservoirs. Vaccines have been developed but are not licensed in the US due to the low risk of infection in developed countries.
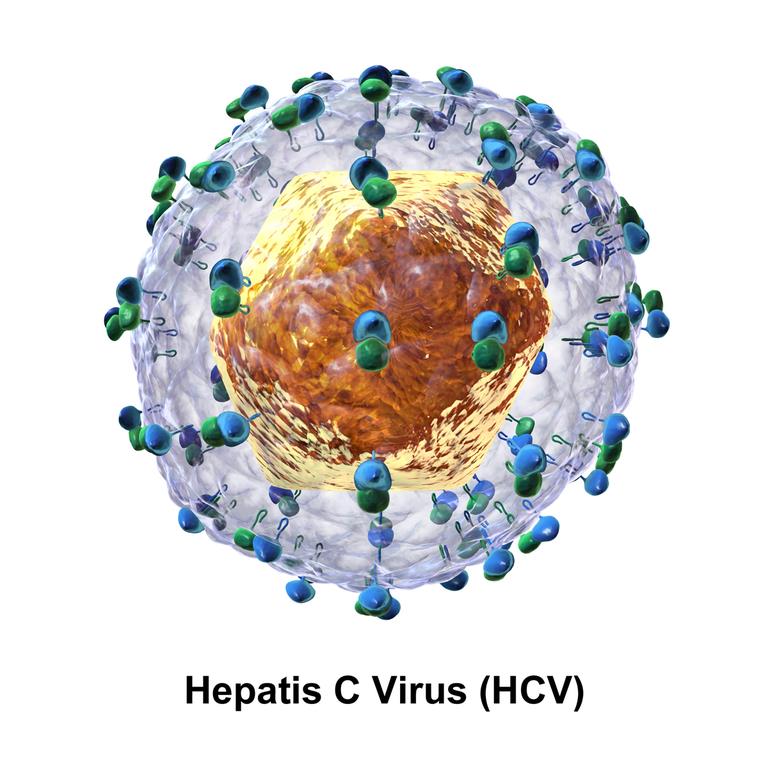
Hepatitis C
Hepatitis C was identified in 1989. It has been found in humans and chimpanzees and is transmitted by intravenous drug use, tattoos, transfusions and other exposures to blood, and by sexual intercourse. Only 15% of patients develop symptoms, but the virus persists in the liver in 85% of those infected; it causes 27% of all cirrhosis cases and 25% of all liver cancers, and is the number one reason for liver transplants. No vaccine is available. More than 3 million Americans are infected, and most of them don’t know it. 75% of cases are in baby boomers, so the CDC recently recommended a one-time screening blood test for those born between 1945 and 1965. Patients with positive tests are monitored with ultrasound, vaccinated against hepatitis A and B, and warned to avoid alcohol and hepatotoxic drugs.
Treatment
The first study of a treatment for hepatitis C was published in 1986, when it was still known only as “non-A non-B hepatitis.” It was a small pilot study (10 patients); treatment with interferon normalized liver function tests, but when treatment was discontinued, patients relapsed. Eventually, an interferon/ribavirin combination became the standard treatment; they were given for 24 or 48 weeks. Cure rates varied from 45% to 80% depending on the HCV genotype. Interferon is contraindicated in patients with certain medical conditions, and serious side effects are common. A systematic review in 2013 showed that a sustained virologic response reduced the risk of liver cancer by 75%. Despite the availability of treatment, the mortality rate from hepatitis C continued to increase until it exceeded the rate for HIV infection.
The new studies
Newer antiviral agents were developed. Three new studies of the combination of ledipasvir and sofosbuvir were published in April of 2014. They were large, randomized open-label studies comparing different antiviral regimens. Placebo controls would have been unethical, since that would have denied subjects the known benefits of treatment.
A four-arm study by Afdhal et al. of 865 previously-untreated patients found high response rates: ledipasvir and sofosbuvir for 12 weeks produced a sustained virologic response in 99% of subjects; for 24 weeks, 98%; with ribavirin added, the rates were 97% after 12 weeks treatment and 99% after 24 weeks.
A similar four-arm study by Afdhal et al. enrolled 404 patients who had already failed treatment with peginterferon and ribavirin. It showed similar results (96-99% response rates).
A study by Kowdley et al. of 647 previously-untreated patients found that 8 weeks treatment with lepipasvir and sofosbuvir was as good as 12 weeks, and adding ribavirin did not improve response.
Virologic response was defined as the absence of quantifiable HCV RNA in serum (less than 25 IU/ml). Side effects were mild, including fatigue, headache, and nausea; no subject in any of these studies had to discontinue treatment because of side effects. The medication was given as a convenient, once-daily pill.
Considering the typical response rates in published studies, these results are astounding. It appears that simply taking a single pill once a day for 8 weeks will safely and effectively protect patients from liver failure and liver cancer. Further studies will be needed to show whether death and transplantation rates will actually decrease, but there is very good reason to expect that they will.
High price tag
There’s only one problem: sofosbuvir pills alone cost $1,000 each, or $84,000 for a 12-week course of treatment; and the addition of ledipasvir will add to the costs. Can society afford the billions of dollars needed to identify and treat everyone at risk? Will we revisit the early days of dialysis when “death panels” rationed treatment and decided which lives were worthy of saving? Today, dialysis is more effective, less expensive, more readily available, and is covered by Medicare for patients of all ages. We solved that problem, and I am optimistic that we will solve the hepatitis C problem as well.
Alternative treatments
Several alternative medicine options have been recommended for the treatment of hepatitis C, including milk thistle, licorice root, ginseng, thymus extract, zinc, SAMe, colloidal silver, probiotics, shisandra, TJ-108 (an herbal mixture used in Japanese Kampo medicine), massage, chiropractic care, and relaxation techniques. The NIH has reviewed the scant available evidence. There is evidence that some of these don’t work, and some of them have not been studied at all. There have been a few mildly positive but questionable studies; but certainly nothing that could even begin to compete with the kind of results achieved in the NEJM studies.
Conclusion: Science works (but does cost money)
The new antiviral treatments for hepatitis C are a great example of science-based medicine in action. We can anticipate that they will save a lot of lives, especially if the economic problems can be overcome.
