[Editor’s Note: I’m pleased to announce that Grant Ritchey has agreed to join SBM as a regular. He’ll be writing about dental science and pseudoscience every four weeks on Sunday. (I swear, we’ll get up to seven day a week publishing if it kills me—or the other bloggers.) Grant will be starting with science, but I’m sure he’ll soon be discussing all the sorts of claims about dentistry and dental disease that are—how shall I put it?—less than science-based soon enough.]
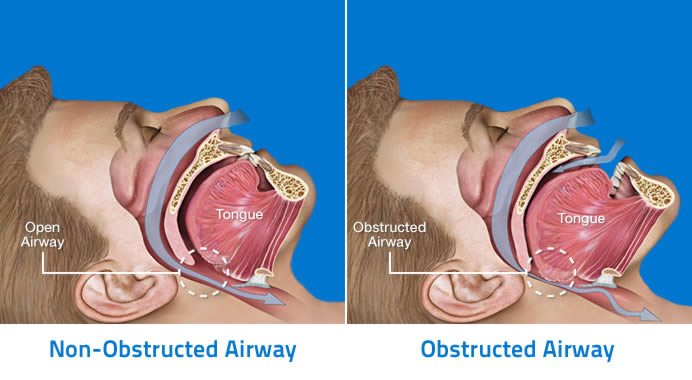
Obstructive sleep apnea (OSA) is a sleep-related breathing disorder in which the airway is partially or completely blocked during sleep. Although little or no air is flowing, the person continues to attempt to breathe. Typically, cessations in breathing last longer than 10 seconds per episode, but can last over a minute and usually occur multiple times during sleep. This can lead to poor sleep quality and precipitous drops in blood oxygenation levels over an extended period of time. This potentially life-threatening condition is frighteningly prevalent, especially in adults over 40, and it is estimated that 80-90% of OSA goes undiagnosed, further compounding the problem.
When a person experiences multiple apneic episodes during the night, the brain responds by alerting the body, resulting in increased efforts to breathe, gasping, and arousal from sleep. These frequent waking events, combined with lowered oxygen levels, can lead to the signs, symptoms, and sequelae of obstructive sleep apnea. Typically, OSA sufferers snore loudly, then are silent for 10-30 seconds as the airway is blocked. This is followed by choking, snorting, or gasping sounds when their airway reopens.
This illustration shows the relationship between the oro-pharyngeal structures and the airway:
Signs and symptoms
According to the American Academy of Dental Sleep Medicine (AADSM) and others, the most common signs and symptoms of OSA are:
- Unintentionally falling asleep during the day
- General daytime sleepiness
- Unrefreshed sleep
- Fatigue
- Insomnia
- Waking from sleep with a choking sound or gasping for breath
- Loud snoring
- Bruxism (tooth grinding). This has been definitively shown in children; it is correlated in adults, but the literature is still inconclusive.
Prevalence
Data from the American Academy of Sleep Medicine (AASM) state:
- OSA is most prevalent in middle aged and older individuals.
- Approximately 2-5% of children exhibit OSA signs and symptoms, but it peaks at approximately 9% for girls and 7% for boys at around age 4 when the tonsils and adenoids are largest relative to head size.
- Approximately 24% of men and 9% of women have obstructive sleep apnea.
As stated above, an estimated 80-90% of OSA remains undiagnosed. OSA in children is primarily due to enlarged tonsils and adenoids, which can impede air flow. As they mature, the tonsils and adenoids usually shrink in conjunction with the growth and development of the head and OSA rates plummet. In adults, sleep apnea is caused by other risk factors.
Risk factors
There are several risk factors that together or separately are predictive for sleep apnea. This list isn’t comprehensive, and a person may have several of these risk factors and not have OSA.
- Overweight individuals
- Men and women with large neck sizes (size 16-17 or larger)
- Ethnic minorities
- Children with enlarged tonsils and adenoids
- Structural abnormalities of the head and neck (e.g. deviated septum)
- Middle aged and older men; post-menopausal women
- Smoking
- People with a family history of OSA
- People who suffer from allergies, rhinitis, and the like.
Diagnosis
The definitive diagnosis of obstructive sleep apnea is made on the basis of an overnight sleep study, monitored by a sleep technologist (when done in a sleep center) and interpreted by a sleep physician. The test, called a Polysomnogram, will chart a patient’s brain waves, heartbeat, and breathing during sleep. It also records arm and leg movements. Traditionally this has been in a sleep center (an “attended study”), but home sleep tests are becoming more common due to convenience and financial considerations. Of paramount importance is the total number of partial (hypopnea) or complete (apnea) cessation of breathing for greater than 10 seconds. Last, the sleep study will monitor the blood oxygen saturation level using a pulse oximeter.
Another thing a sleep physician will assess are any other medical considerations that may mimic or co-exist with OSA, including other sleep apneas (e.g. central sleep apnea, in which the cessation of breathing during sleep is due to a neurological problem, not an obstruction of the airway), medication side effects (many medications cause respiratory depression), substance abuse, or a mental illness (e.g. depression).
Once the sleep study is concluded, an index known as the Apnea Hypopnea Index (AHI), combined with the oxygen desaturation level, is created and a diagnosis is made. The number of apneas and hypopneas are averaged and a score is assigned. Roughly speaking, the classification is broken down as follows:
- AHI < 5: Mild to no OSA
- AHI 5-15: Mild OSA
- AHI 15-30: Moderate OSA
- AHI > 30: Severe OSA
Regarding oxygen saturation, at sea level normal waking blood oxygenation level is around 96-97%. This drops about 5% during sleep. Any blood oxygenation level under 90% is considered problematic; anything under 80% is considered severe.
Sequelae of obstructive sleep apnea
The following is a partial list of adverse effects of long-term OSA. When doctors start talking about the various issues associated with sleep apnea, it is tempting to assume that they think of OSA as a “One True Cause” of a plethora of illnesses. I assure you this isn’t the case. Just as a sedentary lifestyle can cause a breakdown in a wide ranging variety of body systems, so too can chronic hypoxia and interrupted sleep cycles. So please don’t read too much into it, but still appreciate the seriousness of the condition.
- Increased heart rate – the lack of oxygen due to breathing cessation causes the heart to beat faster to supply oxygen to the body’s tissues.
- Elevated blood pressure – the heart has to work harder to get oxygen to the tissues.
- Increased risk of stroke and heart disease.
- Impaired concentration and chronic drowsiness.
- Reduced glucose tolerance and increased insulin resistance.
- Mood changes, depression.
- Disturbance of bed partner’s sleep cycle.
- Erectile dysfunction.
- Increased risk of motor vehicle accidents.
Treatment
After the proper diagnosis is made, OSA patients can be treated in various ways. The three broad classifications of treatment are:
PAP therapy: This has been the gold standard for treating OSA for over 30 years. PAP stands for “positive airway pressure” and it comes in many flavors, with the CPAP (continuous positive airway pressure) being the most popular and familiar. There are also BiPAP (bilevel positive airway pressure) and VPAP (variable positive airway pressure) machines, which deliver variable pressures of air. PAP therapy involves the delivery of pressurized air through a mask or nasal pillows in order to force the obstructed airway open to maintain adequate blood oxygenation throughout sleep. The advantages of PAP therapy are that there is a lot of good data attesting to its efficacy; the main disadvantage is that it is unwieldy and uncomfortable to wear and operate for most people.
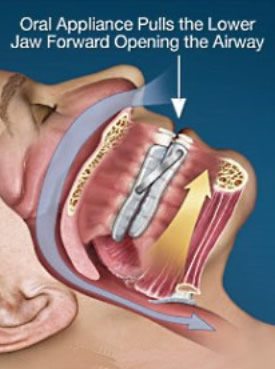
Dental appliance therapy: Oral appliances can be used in many cases of mild to moderate OSA, and in severe cases where the patient is intolerant to PAP therapy. There are many makes and models of appliances, but the vast majority of them are variations on a theme in which upper and lower rigid mouthguards are worn which keep the mandible (lower jaw) postured forward in order to open the airway (see diagram below). I will discuss them in more depth later, but the main advantages of oral appliances are that they are more easily tolerated than PAP machines and are more convenient, especially when traveling. The disadvantages include they are not 100% effective, especially in more severe cases, and in some instances they can be uncomfortable to wear.
Surgery: Not used as often as the other two, there are different surgical techniques employed to open the airway. The most common is the uvulopalatopharyngoplasty (UPPP), in which excess tissue in the throat is removed, widening the airway space. Jokingly referred to as the “Roto-Rooter” approach, it is a fairly aggressive and uncomfortable procedure, and its success rate is marginal at best. Nasal surgeries to correct a deviated septum, genioplasty (tongue reduction), tracheostomy, orthognathic surgery (jaw advancement), and others are also employed. The main advantage of surgery is that it is permanent when successful, and the patient often doesn’t have to be married to a PAP machine or oral appliance for life. The disadvantages are obvious: surgeries are costly, can be risky, uncomfortable, and there is the potential of post-operative complications. Moreover, the efficacy and success rate for most surgeries pale in comparison to the other two alternatives, with the exception of the tracheostomy, which bypasses the obstruction altogether.
In children who are diagnosed with OSA, the removal of tonsils and/or adenoids is usually sufficient to treat the apnea. In the past tonsils and adenoids were usually removed only in cases of persistent infections, but fortunately pediatricians and otolaryngologists (ENTs) recognize the importance of managing children’s airways, even in the absence of infection.
Adjunctive therapies: There are other measures an OSA sufferer can take to help reduce the severity of their disease. In rare cases, the apnea may resolve completely after trying them. Among these therapies are losing weight, training oneself not to sleep on one’s back, medications for allergies, and others. One caveat is that there are many scam therapies out there that should be avoided: acupuncture, herbal remedies, and most of the other CAM therapies that promise to cure everything but don’t have any evidence to support their claims are foisted upon an unsuspecting public. Over the counter appliances are sold at retail stores, online, and on late night TV shows. They are usually marketed as “anti-snoring” devices because they cannot claim to treat an illness or disease, but don’t be fooled. Without a medical diagnosis and proper follow-up, it is impossible to determine if the person indeed has OSA, and if so, if the appliance is effective. Just because the snoring goes away, that doesn’t mean the apnea is gone. And no, I’m not a shill for Big Sleep. You get what you pay for.
More about dental management of obstructive sleep apnea
OK, now you’re a pseudo-expert on OSA, what the signs and symptoms are, how it’s diagnosed, and treatment options. Now I’d like to delve a little deeper into what “sleep dentists” do (note: sleep dentistry is only a special area of interest of some dentists, not a recognized specialty). Of course, as mentioned above, it all starts with a referral to a sleep center where a sleep study under the supervision of a physician is done and a diagnosis made. If the patient does not want to try PAP therapy, or if he or she has tried PAP therapy and found it to be intolerable, an oral appliance may be just what they need.
After an appropriate taking of a medical and dental history, an exam is performed to check for dental pathology or other issues. The polysomnogram is reviewed by the dentist, the patient is informed of the risks and benefits of treatment, and consent is given. The dentist will then take impressions of the upper and lower teeth, as well as registering the proposed initial jaw position so that the laboratory can properly fabricate the appliance. The models are then sent to the laboratory and are ready about 2-3 weeks later. When it returns, it is fitted properly to the patient and instructions are given. A follow-up study is performed (the patient is instructed to calibrate the appliance themselves, looking for silence and an improvement in fatigue), either at a sleep center or (as is more frequently happening) with a home sleep test to confirm that the appliance is effective. If it doesn’t resolve the apnea, the patient returns to the dental office for a reevaluation, and the appliance is adjusted to move the mandible further forward. At some point, a position is determined where the apnea is controlled and the patient is comfortable with the appliance.
I know what you’re thinking. What does that thing look like? The following illustration shows a representative appliance called a Somnodent (By way of disclosure, I have no financial interest in any product I discuss).

As you can see, this appliance fits over the upper and lower teeth. The “wings” on the lower appliance contact the upper extensions, which keep the lower jaw forward to maintain an open airway. There is a screw on each side that can be adjusted to bring the jaw further forward if necessary. After wearing the appliance for a while, the appliance is adjusted and calibrated, moving the jaw forward only as far as necessary to stop the apnea. Other proprietary appliances on the market have an adjustable “strut” connecting the upper and lower members, but the principle is the same for all of them.
Conclusion
Dentists can play a major role in the management of obstructive sleep apnea. We work in conjunction with sleep physicians and technicians to find the most successful means to control a patient’s OSA. Oral appliances have been shown to be very effective when used properly in the appropriate cases. They are not panaceas, however. In many cases, PAP therapy remains the treatment of choice. To learn more about OSA, follow the links given earlier in this post for the dental and medical sleep apnea organizations. In a recent podcast, I interviewed a prominent sleep dentist (Shameless Plug here), who goes into more detail than I was able to in this blog post.
Sweet dreams!

Dr. Grant Ritchey received his Bachelor’s degree in Human Biology from the University of Kansas in 1982, and his Doctor of Dental Surgery degree from the University of Oklahoma in 1986. He lives in Kansas City, is married, and has two grown daughters. Since 1986, he has maintained a general dental practice in Tonganoxie, Kansas, and was awarded a Fellowship in the Academy of General Dentistry in 1998. Currently, he is working toward his Master in Education degree from the University at Buffalo in the Science and the Public program, with an emphasis on the prevalence of alternative medical practices in dentistry. He is also the co-host of The Prism Podcast, a science-based podcast.
