One of these things is not like the other
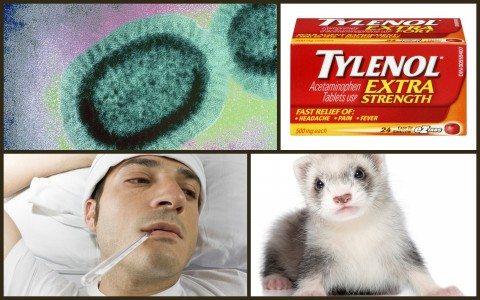
Treating a fever with medication like Advil or Tylenol is reflex action when we come down with colds and influenza. But could treating fevers actually worsen an illness and contribute to its spread in the population? That’s the impression you may have gained from the headlines and press last week, where antipyretics (fever-reducing medications) were described as some type of “anti-vaccine”:
Fever-reducing meds encourage spread of flu: McMaster report
Taking over-the-counter flu medication to cut your fever might help you feel better, but it might not be so good for the people you come into contact with.
When it comes to fever, your mother really did know what’s best
Who would have thought that the simple giving of a fever reducing agent, to either one of our family members or ourselves before we go off to school or work, may inadvertently lead to the death of someone that we see that day?
Use of fever-reducing drugs may lead to tens of thousands more influenza cases
The bottom line is that fever suppression increases the number of annual cases by approximately five per cent, corresponding to more than 1,000 additional deaths from influenza in a typical year across North America.
The paper, published in Proceedings of the Royal Society B, entitled “Population-level effects of suppressing fever“, got a lot of press: Google says 116+ news articles. And it’s not surprising. Who can resist an “Everything you know is wrong” story? It’s a great hook and it seems to call into question one of the most frequent reasons we take medication. Treating fever, especially in children, has been the norm for decades. I can still recall some of my childhood cold- and flu-related feverish nights, 30+ years on. The vivid dreams that felt like hallucinations, the sweating and shivering, and tossing and turning for hours. I’d lie awake waiting for the next dose of Tylenol so I could sleep. Influenza infections can be miserable and exhausting, and have the potential to do serious harm, killing thousands each year. Analgesics that reduce fever, aches and pains may help people get to sleep and to stay asleep – something you covet when you’re bedridden and ill, or caring for your sick child who’s radiating heat.
David Earn, the lead author of the paper, is a professor of mathematics at McMaster University in Hamilton, Ontario. The analysis considers the impact of treating the fever of influenza infections and the population-level consequences. (It’s not available free online, unfortunately.) There is no new medical data in this paper. It is, in the authors’ own words, a “theoretical argument” – a mathematical model based on a series of assumptions:
- Fever is beneficial, not harmful
- Suppressing fever with antipyretics may increase the extent and duration to which the virus is shed
- Treating fever with antipyretics (drugs that reduce fever) increases the probability that the sick will interact with the well
- Sick people using antipyretics will therefore shed more viruses to more people, causing larger epidemics, and more deaths from influenza
Let’s look at these assertions sequentially to assess their validity.
Fever – is it beneficial?
While reaching for analgesics to treat a fever is a reflex action for many, there is some evidence to suggest that fever is a beneficial adaptive response in the infected. Clay Jones discussed fever phobia in 2012 and while he argues that it’s often unnecessarily over-treated, he’s not convinced there’s a sound medical basis for leaving it untreated.
There is merit to the idea that fever has a beneficial purpose but it remains somewhat controversial. Elevating our core body temperature in response to infection is a primitive and almost universal response, seen even in cold-blooded species. Lizards have been observed staying in the sun longer and fish seeking out warmer water when ill for example. This implies at least that there is some degree of survival advantage in being able to develop a fever. Some bacteria and viruses do grow poorly when exposed to higher temperatures. Iron is required for growth by many pathogenic bacteria, and it appears that fever decreases availability of it in the blood. Test tube studies have shown that elevated temperatures may increase the activity of various components of the immune system. There are a few non-primate experiments, particularly in rats and rabbits, that have shown improved outcomes with fever and even some human studies showing prolonged symptoms when fever is treated aggressively. But everything seems to increase the activity of various components of the immune system in test tubes, and those studies were small and difficult to extrapolate to all humans or to all specific fever causing infections. Plus there is also data showing that the immune system may actually become impaired during high fevers above 104-105 degrees. And there is also evidence in animals and human patients that raises concerns of poorer outcomes from some illnesses, particularly in critically ill patients, with very high fever. It is a mixed picture essentially and the jury is still out. Regardless, any benefit of fever is likely so minimal that it would not preclude treatment of a miserable toddler with a temperature of 102.
Mark Crislip has written about the merits of fever as well:
There are numerous beneficial physiologic effects that occur as part of the febrile response. Virtually all aspects of the physiologic response to infection are, dare I say it, boosted, and many wings of the immune system function better at higher temperatures. I feel the naturalistic fallacy creeping over me: fever is an almost universal response to infection that evolved millions of years ago and helps enhance the response to infection. So suppressing a fever during infection should be bad. Right? This becomes a little less clear cut. There are issues as to how the fever is suppressed: mechanical, such as ice or alcohol baths. Pharmacologic: acetaminophen, steroids, aspirin or nonsteroidal anti-inflammatories, all of which have effects that go beyond suppressing fevers. What infection is occurring? A response that has evolved as a response to the infections found on the plains of East Africa could be counter productive against diseases of modernity like Pseudomonas sepsis in the ICU or MRSA endocarditis in a heroin user.
With respect to data on influenza and fevers, Crislip points to this review which notes the following:
In animal models, treatment with antipyretics for influenza infection increases the risk of mortality. There are no randomized placebo-controlled trials of antipyretic use in influenza infection in humans that reported data on mortality and a paucity of clinical data by which to assess their efficacy. We suggest that randomized placebo-controlled trials of antipyretic use in human influenza infection are urgently required, and that these are sufficiently powered to investigate a potential effect on mortality.
The bottom line in the medical literature, nicely summarized by these two SBM authors, is that fevers may offer beneficial effects, but there is no clear evidence of harm from treating them. So it seems premature to conclude that fevers in influenza confer meaningful beneficial effects.
Does suppressing a fever lead to more virus shedding?
The authors make the following statement to support their claim that treating fevers lead to more virus shedding:
To our knowledge, the only published experiment concerning the effects of antipyretic treatment on influenza viral shedding was conducted in ferrets (considered the best animal model for human influenza).
And they’re absolutely correct. There is no published evidence in humans to demonstrate that treating the fevers of influenza leads to more virus shedding. The authors cite what they believe to be supporting evidence in colds and chicken pox infections, but their relevance to influenza is unclear. The only other indirect evidence that seems relevant is a paper that they state shows a correlation between antipyretics and influenza A, but the abstract notes this was due to a second, bacterial infection, so it’s not relevant to this argument. I’m not a fan of relying on animal models to make conclusions about human outcomes, especially when I can easily find contradictory information, such as mice models that find acetaminophen reduces the morbidity associated with influenza without compromising immune responses. On balance it seems reasonable to conclude that there’s no convincing evidence to suggest that treating fevers will lead to more virus shedding.
Does treating a fever increase the likelihood that the sick will interact with the well?
The authors argue that a proportion of infected individuals will treat their fever. This proportion (“p”) will therefore increase their probability of infecting others to some extent (“fp“). The reproduction number (“R”) is the number of secondary infections caused by a primary infection. (In short, how many people does each sick person infect?) R is therefore proposed to increase by a factor of fp because of antipyretic use. The net effect is that treating fevers will increase that reproduction number, and therefore the overall size of the influenza pandemic (“Z”). These calculations are described in detail in a free supplement to the paper.
Are those with influenza infections more likely to interact with the well? The authors offer no justification for this assumption, perhaps believing it to be self-evident. They simply state:
An individual whose fever has been reduced is likely to feel better and is therefore more likely to interact with others.
But there’s no evidence provided to support this statement. It’s a hypothesis that’s completely unsubstantiated. It’s possible, yes. But it’s also speculation. It could be that those with treated infections don’t change their habits enough to increase their contact with others. There is no evidence to answer the question.
Will more viral shedding lead to larger epidemics, and deaths from influenza?
The authors try to establish a relationship between the illness, viral shedding, and transmission of the influenza virus. Their approach is as follows:
In order to infer the overall transmission implications, we need an estimate of the natural infectivity of influenza, i.e. the probability that a susceptible contacted by an (nonantipyretic-using) infectious individual will become infected. We are not aware of direct measurements of this probability, so we use published estimates [42] of the household secondary attack rate (SAR) as a proxy.
Yet another estimate in the absence of direct evidence. It’s not clear that infections within a household are a relevant comparator to the broader population. So this another assumption based on indirect data of questionable relevance. There is some research in this area which is somewhat supportive of the idea that virus shedding is generally correlated with the severity of the infection. However, it’s been established that virus shedding starts before symptoms like fever appear, and children start shedding earlier than adults. In addition, shedding can continue for days or even weeks after the symptoms have disappeared. It’s also important to note that 30-50% of influenza infection may not cause illness. And if they don’t cause illness, there’s no need to treat a fever. On balance, there’s no substantive or persuasive evidence to demonstrate that the antipyretics will have any meaningful influence on the degree to which influenza is spread in a population.
The remainder of the paper is the description of a population-based model estimating the negative consequences of treating the fevers of influenza. The authors estimate that most influenza fevers are treated with antipyretics (and again, don’t provide any direct evidence), ultimately concluding that treating fevers with antipyretics increases the spread of influenza by “at least 1%”, and suggesting that “at least 700 deaths per year” could be prevented in the United States alone by avoiding antipyretic medication when treating influenza. To the authors’ credit, they use a range of probabilities for each of their estimates. But in the absence of establishing cause-and-effect to any meaningful degree, this reminded me more of tooth fairy science than of a serious discussion of epidemiology. The authors paint a correlation between the harms of antipyretic use with the indiscriminate use of antibiotics, a comparison that falls flat given the good evidence of harms with antibiotic use, and the speculation throughout this analysis.
Conclusion
The idea that treating the fever of influenza with medication leads to more deaths in a population is a hypothesis. Critically, the authors fail to provide adequate scientific justification for their approach, nor do they substantiate any of their key assumptions with real world data. While successful in gaining media impressions and potentially frightening people away from treating the fevers associated with influenza, the paper fails to offer any credible evidence to support their claim that antipyretics have serious, negative population-level consequences. While it’s perfectly fine not to treat a fever, there is no convincing evidence to suggest that you’re putting others in the population at risk if you choose to do so.
Reference
Earn D.J.D., Andrews P.W. & Bolker B.M. (2014). Population-level effects of suppressing fever, Proceedings of the Royal Society B: Biological Sciences, 281 (1778) 20132570-20132570. DOI: 10.1098/rspb.2013.2570
