We spend a lot time at SBM discussing different elements of the art and science of medicine, and how we believe that practice can be improve. Yet our science-based intentions can be thwarted at the last possible moment – in the form of dosing errors. The workup may have been comprehensive, the diagnosis could be correct, the most clinically and cost-effective intervention chosen, and whammo. An overdose or underdose, possible toxicity, and a failure to achieve the desired outcome. It’s a completely avoidable, but often overlooked aspect of the practice of medicine.
In my last post, I noted how cough and cold products for children have largely been withdrawn from the market due to their lack of efficacy, and the risks related to toxicity. Today’s post is going to dive a little more deeply into factors that can contribute to toxicity in the pediatric population. Let’s start with a vignette that may be familiar to parents:
The new father is wakened from a blissful, deep sleep by a crying child. Once Dad realizes when and where he is, and the source of the crying, he silently curses the short duration of action of the acetaminophen liquid he gave his child at bedtime. It has probably worn off already, and the fever is back. Stumbling into his child’s room in the dark, he can feel the heat radiating off his body. He fumbles around for the Tylenol, and something to measure it with. He can’t find the dropper bottle, but finds a bottle of syrup. It’s hard to measure the dose in the dark, and the medicine cup he finds is hard to read. “I think the dose is a teaspoon..that’s 5mL”. He pours the medicine into his child’s throat, tucks him back into bed, and both are back asleep within minutes.
Did this parent measure the acetaminophen dose correctly? What factors could contribute to a dosing error in this situation?
Dosing errors are the among the most common and most preventable causes of adverse drug events in children. Why children? Drugs for children are often in liquid form for ease of measurement and administration. Typically dosed based on milligrams per kilogram, liquid formulations allow us to (in theory) deliver the exact dose that’s appropriate. But measurement isn’t always easy or intuitive. What’s the best way to measure 2.5mL (half a teaspoon)? How easy is it to confuse teaspoons (5mL) and tablespoons (15mL)? And what instructions should health professionals give parents and caregivers to ensure they can measure and administer a dose accurately? Despite the prevalence of dosing errors, there has been little evidence telling us what health professionals, or parents, can do better. Until now.

In a study by Yin et al in Archives of Pediatric and Adolescent Medicine, the authors set out to determine what works, and what doesn’t, when it comes to measuring liquid medications for children. When measuring a liquid, formulation-specific issues such as viscosity (thickness) and surface tension affect the way a liquid behaves. The delivery instrument of choice should compensate for these factors, so the correct dose is administered. In health care settings, the oral syringe is preferred as many of these factors are minimized. But what about in the hands of consumers?
The Study
The study design was simple but effective. Parents were enrolled from a pediatric clinic. All were instructed to measure 1 teaspoon (5mL) of a medication (acetaminophen) using six different measurement methods (links are sample images):
- A dosing cup with printed markings (capacity 15 mL or one tablespoonful)
- A dosing cup with etched markings (capacity 30 mL or two tablespoonfuls)
- A dropper (capacity 5 mL)
- A dosing spoon (capacity 10 mL)
- An oral syringe (capacity 5 mL)
- A oral syringe with a bottle adapter (allows the drug to be easily drawn up directly from the bottle) (capacity 5 mL)
Each participant measured using all devices, but they were presented in random order. The measured dose was compared (by weight) with a reference dose drawn up with an oral syringe. Literacy of participants was also assessed using the Newest Vital Sign test, to evaluate what influence that might have on measurement practices. Sociodemographic and child health status information were also collected.
The investigators defined an appropriate dose as one that contained no more that 120% of the expected dose. A small error was 120% to 140%, and a large error was anything more than 140% of the target 1 tsp (5 mL) dose.
The Results
302 subjects were recruited; they were mainly female (95%), Hispanic (80%), and non-US born (76%). About half were high school graduates (51%) and the majority were predicted to have a high likelihood (41%) or possible likelihood (38%) of limited literacy.
Underdoses with all devices were virtually nonexistent. Excess doses, on the other hand, were common. The worst product was the printed dosing cup, where only 30% of parents could measure a dose accurately. The etched dosing cup was a bit better, at 50%. The dropper had the most accurate dosing, with 94% measuring correctly. The syringe was 91%, and the dosing spoon was 86%.
When literacy was examined, it was negatively correlated with dose measurement accuracy. That is, caregivers with lower literacy were more likely to make “large errors” with the different dosing instruments. These errors were far more common with the dosing cups, however.
So what can we conclude? Devices matter. Oral syringes are the gold standard for accuracy, and in the case of prescription drugs, should probably accompany all liquids dispensed. Other devices are more or less accurate. Consider in the context of our sleep-deprived father measuring acetaminophen. What are the odds that he’ll measure the dose correctly? To answer that, we need to look at how over-the-counter products are labelled, packaged, and used.
Designed for dosing errors?
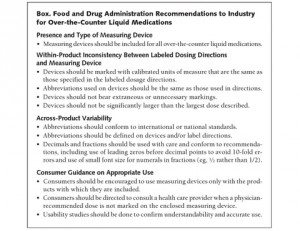
In late 2009, in response to over-the-counter unintentional overdoses, the FDA released voluntary guidance to industry. Recommendations were as follows:
In a second paper by Yin and associates, just published in the Journal of the American Medical Association, the authors set out to evaluate the dosing directions and measuring devices that accompanied currently marketed pediatric cough and cold products.
The Study
This was a descriptive study that looked at 200 top-selling pediatric over-the-counter oral liquid medications. Samples represented 99% of the U.S. market for analgesics, cough/cold, allergy, and gastrointestinal oral liquids. Products were scored on the following:
- inclusion of a measuring device (dropper, cup, syringe, etc.)
- Within-product consistency between labeled directions and markings on the measuring device (e.g., teaspoons, millilitres, on bottle and label)
- Across-product variability (e.g., use of non-standard units and abbreviations (not mL, tsp, etc.))
- Lack of guidance on appropriate use (e.g., caution to only use enclosed measurement device).
This was a baseline study, conducted before the FDA’s guidance could have been implemented. Most of the products (45%) sampled were cough and cold treatments, with the rest being a mixture of analgesic, allergy, gastrointestinal, and combination products.
The Results
Measuring devices were supplied in 74% of products. Of those devices, significant problems were identified: 98.6% had inconsistencies between the dosing directions on the package, and the markings on the device itself. Deficiences included missing markings (24.3%), superfluous markings (81.1%), atypical units of measure (5.5%).
Evaluation
It seems intuitive that unclear directions can be a contributing factor to dosing errors. Deciphering labels and accurately dosing medications can be challenging to anyone, particularly those with limited health literacy. In the case of over-the-counter medications, there may be few opportunities for consultation before these products are used.
With over-the-counter cough and cold medications for pediatric populations, we had a group of products without good evidence of efficacy and the possible but rare risk of toxicity, particularly in overdose situations. It’s possible that packaging and labelling were factors that contributed to its toxicity and to its ultimately unfavourable risk-benefit evaluation. But the finding in these trials trials provide broader guidance to help us reduce the risk of dosing errors:
- Measuring devices should be used with all pediatric liquids, over-the-counter or not. Oral syringes are the most accurate devices. Kitchen utensils should be avoided.
- Consistency between what the label says, and what the measuring device actually measures, is important. Ideally, the device should not be able to measure more than a single dose of the medication.
- Standardized units of measurement should be used. Even “teaspoon” and “tablespoon” can be misinterpreted into 3-fold errors. Millilitres (mL) is preferable, though it admittedly is not an intuitive measuring unit to everyone.
- When expressing fractional amounts, always use leading zeros (i.e., 0.5mL)
Conclusion
Arriving at a science-based, individualized treatment for a child isn’t that useful if parents can’t measure the correct dose. Two recent studies give us data to improve the way we use pediatric liquid medication. In doing so we can improve patient outcomes and reduce the risks associated with medication use.
References
![]()
Yin HS, Mendelsohn AL, Wolf MS, Parker RM, Fierman A, van Schaick L, Bazan IS, Kline MD, & Dreyer BP (2010). Parents’ medication administration errors: role of dosing instruments and health literacy. Archives of pediatrics & adolescent medicine, 164 (2), 181-6 PMID: 20124148
Yin HS, Wolf MS, Dreyer BP, Sanders LM, & Parker RM (2010). Evaluation of Consistency in Dosing Directions and Measuring Devices for Pediatric Nonprescription Liquid Medications. JAMA : the journal of the American Medical Association PMID: 21119074