A Brief Clinical Vignette
In researching this post, I found an article published nearly two years ago in The Hospitalist entitled Growth Spurt: Complementary and alternative medicine use doubles, which began with this anecdote:
Despite intravenous medication, a young boy in status epilepticus had the pediatric ICU team at the University of Wisconsin School of Medicine and Public Health in Madison stumped. The team called for a consult with the Integrative Medicine Program, which works with licensed acupuncturists and has been affiliated with the department of family medicine since 2001. Acupuncture’s efficacy in this setting has not been validated, but it has been shown to ease chemotherapy-induced nausea and vomiting, as well as radiation-induced xerostomia.
Following several treatments by a licensed acupuncturist and continued conventional care, the boy’s seizures subsided and he was transitioned to the medical floor. Did the acupuncture contribute to bringing the seizures under control? “I can’t say that it was the acupuncture — it was probably a function of all the therapies working together,” says David P. Rakel, MD, assistant professor and director of UW’s Integrative Medicine Program.
The UW case illustrates both current trends and the constant conundrum that surrounds hospital-based complementary medicine: Complementary and alternative medicine’s use is increasing in some U.S. hospitals, yet the existing research evidence for the efficacy of its multiple modalities is decidedly mixed.
My jaw dropped in horror when I read this story. Acupuncture for status epilepticus? There’s no evidence that it works and no scientific plausibility suggesting that it might work. And what does the questionable research suggesting that acupuncture might ease chemotherapy-induced nausea and vomiting or radiation-induced xerostomia (which, if you look more closely at the studies, it almost certainly does not, but that’s a post for another time) have to do with this case, anyway? Nothing. Worse, Dr. Rakel fell for the classic post hoc ergo propter hoc fallacy; i.e., despite his disclaimer, he appears to be implying that, because the child recovered, acupuncture must have contributed to his recovery. He also repeats the classic fallacy that I’ve written about time and time again in the context of cancer therapy, namely that if a patient is using quackery as well as science-based medicine, then either it was the quackery that cured him or the quackery somehow made the conventional medical care work better.
I expect better from an academic medical center like the University of Wisconsin. Unfortunately, increasingly I’m not getting it. Quackademic medicine is infiltrating such medical centers like kudzu.
A survey, a survey, my kingdom for a survey!
One of the most frequently used arguments by promoters of “complementary and alternative medicine” (CAM) or, as it’s more frequently called these days, “integrative medicine” (IM) has nothing to do with science at all. Actually, few of the arguments put forth for “complementing” or “integrating” quackery (which, let’s face it, is all the vast majority of IM really is) with science-based medicine actually have anything to do with science, favoring vague and fuzzy appeals to “holistic” medicine and the “whole patient,” as though it’s not possible to be holistic without adding a heapin’ helpin’ of magical thinking to medicine. It’s the classic false dichotomy: Either we inject a generous dose of woo into our medicine, or medicine remains “non-holistic” or, even worse, reductionistic, and we all know how evil “Western” reductionistic science is, right?
No, one of the favorite tactics used to market CAM/IM comes straight out of the Madison Avenue playbook. Indeed, I can imagine Don Draper of Mad Men cooking it up. It’s a classic argumentum ad populum, whereby CAM/IM advocates try to represent their “product” as being very popular and gaining in popularity every day. These sorts of appeals on the part of CAM/IM frequently emphasize the various subcategories of argumentum ad populum, such as the “bandwagon fallacy,” in which it is argued that, because most people believe something (or because large numbers of people; i.e., a sizable majority) you should believe it too, or at least consider it more seriously. Regular readers should be able to see the problem inherent in that approach. After all, many people believe in ghosts or astrology; the fact that such beliefs are popular does not make them true. The second form of argumentum ad populum is known as “snob appeal,” in which CAM proponents try to persuade you of a conclusion by appealing to what an elite or a select few (but not necessarily an authority) in a society thinks or believes. Of course, I view this variety of argumentum ad populum as more an appeal to authority than anything else, and, as I point out from time to time, an appeal to authority is not always a fallacy, which is why legitimate authorities need to be careful and responsible in what they say. What they say matters to non-experts.
We in medicine have apparently been failing in this respect utterly with respect to CAM/IM.
What led me to this conclusion yet again is a recent survey that’s being flogged in the CAM/IM blogosphere that reports to have found that CAM/IM programs are becoming more common in hospitals and medical centers. My first reaction was almost shruggie-like in that I just wanted to shrug my shoulders and agree with Steve Novella that pseudoscience sells. But then I decided to take a closer look.
What I’m referring to is the 2010 Complementary and Alternative Medicine Survey of Hospitals, a survey that was carried out by the Samueli Institute in collaboration with Health Forum, which is listed as an American Hospital Association Company.” Oddly enough, this survey was not funded by the National Center for Complementary and Alternative Medicine (NCCAM), but rather by the US Army Medical Research and Materiel Command under Award No. W81XWH-10-1-0938. With two wars going on, one would think that the Army would have better things to spend taxpayer dollars on. Apparently you’d be wrong.
For those of you who don’t remember the Samueli Institute, it’s one of the major forces, along with the Bravewell Collaborative, promoting the infiltration of quackademic medicine into academic medical centers. It even describes itself thusly on the cover page of its survey report:
Samueli Institute is a non-profit research organization investigating the safety, effectiveness and integration of healing-oriented practices and environments. We convene and support expert teams to conduct research on natural products; nutrition and lifestyle; mind-body practices; complementary and traditional approaches such as acupuncture, manipulation and yoga; and the placebo (meaning) effect. We support a knowledge network that assists in integrating evidence-based information about healing into mainstream health care and community settings and in creating Optimal Healing Environments.
The “meaning” effect“? Holy Dan Moerman, Batman!
Professor Moerman aside, in a couple of talks I’ve given, I’ve used the Samueli Center for Integrative Medicine at UC-Irvine as an example of just how egregious quackademic medicine can get. Indeed, right there on the SCIM website you can see a homeopath, along with acupuncturists and naturopaths. Some of these might well recommend something called FirstLine Therapy, which is basically a program marketed by Metagenics. Not surprisingly, dietary supplements are part of the program, as is “Ultrameal,” which is billed as “medical food” and takes the form of expensive drink mixes and bars. Yum.
But I digress. What about the survey itself? Let’s go to the Samueli Institute’s press release first:
Hospitals across the nation are responding to patient demand and integrating complementary and alternative medicine (CAM) services with the conventional services they normally provide, according to the results of a new survey released today by Health Forum, a subsidiary of the American Hospital Association (AHA) and Samueli Institute, a non-profit research organization that investigates healing oriented practices. The survey shows that more than 42 percent of responding hospitals indicated they offer one or more CAM therapies, up from 37 percent in 2007.
Note how this is a clever combination of the bandwagon appeal and an appeal to authority. After all, there is “patient demand,” and the authorities (i.e., hospitals) are responding. The unspoken subtext is the assumption that hospitals wouldn’t respond to such a demand if there weren’t something to it. They are, after all, health care institutions made up of health care professionals, right? Well, yes, but hospitals are also businesses, and many of these health care professionals have either bought into the myth that “holism” and improving the doctor-patient relationship requires woo, or they are shruggies.
Meanwhile, CAM/IM apologists and supporters are jumping all over this survey as “evidence” that they are winning. John Weeks of the Integrator Blog, for instance, crows:
The most significant data point here is that 74% say that “clinical effectiveness” is a top reason for inclusion. This growth took place in a down economy and despite the lack of good payment models for CAM. These findings will be interesting to view after new incentive structures that might support CAM inclusion kick in with the growth of accountable care organizations (ACOs).
“Clinical effectiveness”? Based on what? Certainly not science in most cases.
In any case, the story has gotten some traction in the mainstream media, such as the L.A. Times, which, tellingly, chose to report on the survey on its Money & Company blog under the title Alternative medical services growing at U.S. hospitals, quoting widely from the joint press release of the AHA and Samueli Institute.
But does the survey actually show what it claims? Let’s go to the report itself. The first thing I noticed when I read the report was that it’s full of the typical “bait and switch” language of CAM designed to inflate the numbers of people who apparently use “CAM modalities.” For instance, diet, exercise, and the like are represented deceptively as being somehow “alternative” when their utility not only can be studied by science but has been studied by science. None of this is surprising, but it is harmful in that it applies a layer of “mystery” and “danger” to modalities that physicians have been prescribing their patients for a long time, such as better nutrition and more exercise. These modalities are, in effect, “woo-ified.” Then, they are lumped together with the real woo, such as acupuncture, homeopathy, and “energy healing,” in order to provide legitimacy by association. For instance, if you look at Figure 2, you’ll see that natural products are the most commonly reported CAM modality, which tells me that the supplement industry’s marketing hype has been effective. More tellingly, other than chiropractic, all of the top nine modalities are nothing that couldn’t be considered SBM. True, homeopathy just barely squeaks into the top ten at number ten, but only 1.8% of adults in the U.S. have reported using it. (I suspect the number would be higher in Europe.) Where’s traditional Chinese medicine? Where’s acupuncture? Where’s “energy healing”? Apparently none of them made the top ten. For instance, if you go to the 2007 National Health Interview Survey Report, you’ll find that only 1.4% reported using acupuncture; 0.4% reported using naturopathy; 0.1% reported using Ayurveda; and 0.5% reported using reiki.
No wonder the bait and switch move is necessary, at least if CAM practitioners want to represent the popularity of their methods as being higher than single digit percents (or in some cases higher than 1%).
Here’s how the survey was done:
The 2010 Complementary and Alternative Medicine Survey of Hospitals, a 42-question instrument, was mailed to 5,858 hospitals from American Hospital Association’s inventory of opened and operating member and nonmember hospitals in March 2010. Respondents had the option to either complete the survey online or mail back a hard copy. A total of 714 responses were received for a response rate of 12%. Of responding hospitals, 299 (42%) stated that they offered one or more CAM therapies in the hospital—which could be either in the form of services provided to patients or employees.
Does anyone see the problem here? It’s fairly obvious, namely the response rate. It’s pretty hard to say much of anything based on a 12% response rate. Basically, all we can say is that 42% of the respondents have a CAM program of some sort or another, but we have no idea whether the respondents are a representative sample. Indeed, they almost certainly are not; there is probably major selection bias going on here, with respondents more likely to be the ones who have some sort of CAM program. Just the geographic distribution of responses makes me wonder, though, with 23% coming from the Midwest and only 11% coming from West Coast states. Later in the report, it is pointed out that “most of the hospitals responding to this survey would be considered ‘early adopters'” who are, apparently, adopting CAM “because they believe it’s the right thing to do or because it’s important to respond to the needs of their communities and patients.” Clearly, this is not a representative sample. Be that as it may, it can still be informative to examine this non-representative sample. For example, the “bait and switch” continues here, with the top six outpatient modalities being:
- Massage therapy
- Acupuncture
- Guided imagery
- Meditation
- Relaxation
- Biofeedback
And the top six inpatient modalities being:
- Pet therapy
- Massage Therapy
- Music/art therapy
- Guided imagery
- Relaxation training
- Reiki and therapeutic touch
The authors of the survey report conclude with amusing understatement:
Looking at the top modalities offered in hospitals it is clear that hospitals are “playing it safe” and starting with fairly conservative and non-invasive therapies to appeal to the broadest range of patients and consumers in the their community. Pet therapy has been growing in popularity. Massage therapy is provided predominantly for pain and stress management and for cancer patients, according to the American Massage Therapy Association’s 2007 Survey of Massage Therapy Utilization in Hospitals.
Other key findings include:
- Majority of respondents offer wellness services for patients and staff, including nutritional counseling, smoking cessation, fitness training and pastoral care;
- Massage therapy is in the top two services provided in both outpatient and inpatient settings;
- The majority of hospitals that offered CAM were urban hospitals (72 percent); and
- Seventy-five percent cited budgetary constraints as the biggest obstacle for implementation of CAM programs.
It is rather instructive, though, to look at the differences between inpatient and outpatient. First of all, who decided that “pet therapy” was in any way alternative? It’s not really “therapy,” either: it’s a great way to raise spirits among hospitalized patients, but lumping it in as a “CAM” therapy seems a major stretch to me. (If pet therapy is an “alternative” or “integrative” therapy, then sending hospitalized patients a card and flowers to lift their spirits must also be alternative or integrative therapy.) Secondly, it is interesting how reiki and therapeutic touch are major offerings in the inpatient realm but not in the outpatient realm. Very likely this is due to the decades-long infiltration of therapeutic touch in the nursing profession, leading too many nurses to come to believe that they can somehow realign a patient’s energy field to healing effect by waving their hands around. Reiki fits right into that, particularly given that reiki practitioners have been making a concerted effort to get into hospitals and offer their “services” to patients.
Money vs. ideology
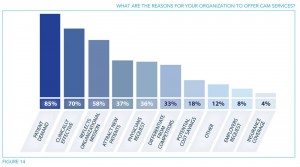
It’s even more instructive to look at the reasons given for starting up a CAM program. Inevitably, financial considerations, plus popularity and a perceived demand among patients, are among the handful of factors that predominate:
Look at what comes in as number one: patient demand at 85%. None of this is surprising, given that in the introduction it is stated:
The American public is also demanding that their hospitals offer more than conventional allopathic health care and begin to integrate CAM therapies into the care they receive in the hospital. In response, hospitals have been looking to meet the needs of their communities. The demand for CAM services is significant, even though insurers may not cover all services or products, with the American public spending approximately $12–19 billion on CAM providers and a total of $36–47 billion on all services and products combined.
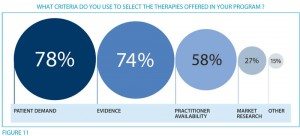
Which at first suggested to me that it’s almost all about the business. There’s a lot of money to be made in CAM, and it’s paid for out of pocket. It’s also instructive to look at the reasons given for choosing the CAM modalities offered:
There are, however, a couple of anomalies here. Most prominent, given that only 27% state that market research drove their decision to offer CAM, one wonders how all the others who didn’t do any market research (78%) knew that there was enough patient demand to justify spending the money to offer specific CAM services. In any case, I consider it also telling that the survey reports that 85% will use patient satisfaction as a metric to evaluate the CAM program while only 42% plan on evaluating health outcomes and 31% will evaluate quality. Don’t get me wrong, patient satisfaction is important, and we measure it for science-based medicine. However, there’s something wrong when twice as many hospitals with CAM programs will be looking at patient satisfaction as will be looking at health outcomes.
Perhaps the most interesting part of this study suggests that it may actually not be all about the money, despite the listing of how lucrative CAM can be. For example, only 57% of facilities will be using volume as a criterion for evaluating their CAM program. Is there a clinical program on earth (or at least in the U.S.) that doesn’t use volume as part of its criteria for evaluating it? It may be one of many, and it might not even be one of the more important criteria, but it’s usually a significant criterion. Adding to this, only 39% will use revenue; 20% will use profit; and 8% will use market share. To me these suggest that perhaps CAM is indeed more ideological than financial, particularly when coupled with the finding that 75% of hospitals reported that budgetary constraints are the biggest obstacle to implementing a CAM program, even though such programs can cost as little as $200,000 to start up. (One notes, in contrast, that only 43% reported that a “lack of evidence-based studies” was a major obstacle.) No wonder quackademic medicine is trying so hard to entice third party payers to reimburse for their services; if that were to happen, no doubt many CAM programs that are currently not financially viable will become viable. Perhaps, for as unrepresentative a sample as was surveyed, this survey serves the inadvertent purpose in providing evidence to suggest that the infiltration of quackademic medicine is not driven primarily by money, as skeptics and supporters of SBM (myself included) have on occasion speculated.
Maybe it really is about the ideology.