If there’s one form of so-called “complementary and alternative medicine” (CAM) that I find more tolerable than most, it’s massage therapy. The reason, of course, is that, whatever else anyone claims about massage, there’s no doubt that it feels good. Indeed, I’ve sort of come around to Kimball Atwood’s way of thinking. Back when he and I were on a panel together at TAM9, Kimball said something somewhat surprising, namely that he’s not sure we even need to test massage in randomized clinical trials because we all know that it feels good and if it feels good it can certainly be helpful at the very least to improve patients’ quality of life. Unfortunately, there’s a lot of woo in massage these days, and massage therapists who buy into the woo aren’t satisfied with simply using the rationale that massage feels good to recommend it to patients. They just can’t resist going beyond that to infuse massage therapy with every bit as much woo as any chiropractor or acupuncturist infuses into his respective specialty. For instance, some of the claims for massage include:
- Decreases muscle pain & tension.
- Rejuvenates the body and mind and lifts the spirit.
- Relieves anxiety, stress and tension.
- Relaxes muscles.
- Alleviates headaches.
- Hastens healing.
- Increases ranges of motion.
- Facilitates removal of waste and inflammation by-products.
- Stimulates the immune system.
- Eases symptoms related to fibromyalgia.
- Promotes relaxation and comfort.
- Reduces nausea in pregnant women.
- Accelerates weight gain in premature infants.
- Helps premature infants become more active and aware.
- Increases energy and alertness.
- Enhances morale and attitude.
Of course, there’s little doubt that a good massage probably can relax muscles, promote relaxation and comfort (which seems like the same thing to me), and enhance morale and attitude. I’d even be willing to concede that massage, properly administered, can probably also alleviate headaches (tension headaches, anyway) and increase range of motion in joints. But facilitate the removal of waste and inflammation byproducts? Stimulate the immune system (the all-purpose meaningless claim)? Hasten healing? Not so much.
All too often massage therapists ruin a perfectly good massage by imposing pseudoscientific and quack claims on it, such as claims that they are stimulating acupressure points or their adoption of the language of “energy healing.” Our own assistant editor, Paul Ingraham, a former massage therapist, has thoroughly covered claims about massage therapy and myofascial pain.
So it was with a bit of trepidation (but also more than a bit of interest) that I took a look at some links that readers sent me about a week ago (too late, alas, for me to write about this last Monday). These links were to news stories with titles like Scientists Uncover Why Massage Heals Sore Muscles and Massage Reduces Inflammation And Promotes Growth Of New Mitochondria Following Strenuous Exercise, Study Finds. My first impression, actually, was that this was somewhat counterintuitive in that one might predict that deep kneading of muscles might actually cause a bit of inflammation and that it’s the counterirritation effect that leads to the perceived reduction in the amount of pain. Yet, according to the press release issued by McMasters University, whose contents were mirrored in many news stories, a study claiming state-of-the-art methods is concluding that massage is reducing inflammation:
Most athletes can testify to the pain-relieving, recovery-promoting effects of massage. Now there’s a scientific basis that supports booking a session with a massage therapist: On the cellular level massage reduces inflammation and promotes the growth of new mitochondria in skeletal muscle. The research, involving scientists from the Buck Institute for Research on Aging and McMaster University in Hamilton Ontario appears in the February 1st online edition of Science Translational Medicine.
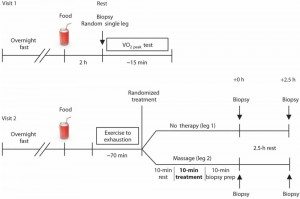
The study involved the genetic analysis of muscle biopsies taken from the quadriceps of eleven young males after they had exercised to exhaustion on a stationary bicycle. One of their legs was randomly chosen to be massaged. Biopsies were taken from both legs prior to the exercise, immediately after 10 minutes of massage treatment and after a 2.5 hour period of recovery.
My first thought upon reading this press release was that this was rather interesting and I wanted to find out more. My second thought, which turned out to be correct, was that the investigators were totally overselling their preliminary results.
Unfortunately, my third thought was: Muscle biopsies? Really? Although it is possible to do a needle biopsy of the muscle, most of the time muscle biopsies are surgical procedures, and, although the description of how the muscle biopsies were done is maddeningly vague in this paper, they do not appear to have been needle biopsies, which could not have provided enough tissue to do all the tests the investigators ran. In any case, I’ve done muscle biopsies before. They involve making an incision, carrying it down to the fascia overlying the muscle, cutting into the fascia, and then taking a piece of muscle. Sure, muscle biopsies can be done under local anaesthesia, and they’re not big procedures, but they are surgical procedures, in this case, being done for no therapeutic intent on healthy volunteers. One wonders how the investigators got this study past the Institutional Review Board (IRB), because I know for sure that the IRBs at the two institutions where I’ve been on the faculty would probably have—shall we say?—challenged the investigators on their experimental design. Yet approved this study was by the McMaster University Research Ethics Board. Leaving aside the problems I have from an ethics standpoint of doing not one, not two, but five (!) unnecessary muscle biopsies on research subjects, the next question I have is whether this study actually shows what the investigators claim it shows. To do that, I went straight to the source, namely the study in Science Translational Research by Crane et al. entitled Massage Therapy Attenuates Inflammatory Signaling After Exercise-Induced Muscle Damage. Here’s one of the investigators discussing the study:
Buck Institute Faculty Simon Melov, PhD, Discusses Recent Study on Molecular Benefits of Massage Therapy Following Exercise from Buck Institute on Vimeo.
When I first heard of this study, I couldn’t make up my mind whether it was good science, a fishing expedition that got lucky, or woo-omics. Then I got around to looking up the study, and I wondered if I was the only one disturbed by its design. Its big problem is that the investigators didn’t strike me as having a strong enough preclinical data base to justify doing a clinical trial in which medically unnecessary invasive procedures were carried out on healthy people and then whole genome mRNA expression profiling carried out. From my perspective, before doing five muscle biopsies on research subjects, there should be evidence from other less invasive (or preferably noninvasive) methods compelling enough to justify such an expensive study using invasive testing methods on humans. Yet, here is the authors’ justification:
Massage therapy is a well-known form of alternative medicine that consists of physical manipulation of muscle and connective tissue at a site of injury, inflexibility, or soreness to reduce pain and promote recovery (1, 2). Massage has been hypothesized to moderate inflammation, improve blood flow, and reduce tissue stiffness, resulting in a diminished sensation of pain. The potential benefits of massage could be useful to a broad spectrum of individuals including the elderly, those suffering from musculoskeletal injuries, and patients with chronic inflammatory conditions. About 18 million individuals undergo massage therapy annually in the United States, making it the fifth most widely used form of CAM (1). The functional benefits of massage remain contentious in humans (2–4), and experiments using massage therapy in animals may not properly mimic the human responses, limiting their usefulness. Despite several reports that long-term massage therapy reduces chronic pain and improves range of motion in clinical trials (5–7), the biological effects of massage on skeletal muscle tissue remain unclear.
After going on about various aspects of inflammation, which is what happens to muscle when it’s overworked because there are small tears in the myofibrillar structure of the muscle. So, basically, the authors’ hypothesis seems to be that massage somehow mediates inflammation and their rationale for choosing the study design they chose was that animal models may not mimic human responses, an assertion that, I note, the authors make without citing references to back it up. Is that enough to justify a clinical trial with this many muscle biopsies? I say no, but obviously the McMaster University Research Ethics Board did not agree. I also did not at all like how the authors bought into the language of “complementary and alternative medicine” (CAM), referring to massage therapy as “alternative medicine.” It is not, or, at least, it should not be considered so. The extent that massage is “alternative” depends directly on the amount of woo overlaid on it. It is, after all, physiologically plausible that manipulating muscles can do something to inhibit or release cytokines or other factors that might either increase or decrease inflammation. Of course, this plausibility should have been explored in an appropriate animal model before moving straight to human studies.
Preliminary results overblown
There is little doubt that this particular study is the most “high tech” study ever done on massage therapy in that some fairly heavy duty genomic techniques were brought to bear on the question of what gene changes occur (1) after heavy exercise and (2) in response to massage therapy. It’s a small study (only 11 subjects), which means that there’s the potential for a lot of noise, which further means that the results had better be striking (i.e., at least a two-fold or better change in gene expression) to be suggestive or convincing, and that replication is needed. The former definitely didn’t apply, and the latter is awaited, although I don’t think that I’d want to repeat a study that involves five muscle biopsies per subject.
Let’s take a look at the trial design itself, as shown in Figure 1 (click for full size):
As you can see, there are two visits and a total of five biopsies performed on each subject, one baseline and then two performed on each leg, before and after massage of one leg and before and after no massage on the opposite leg. Total RNA was isolated from these muscle biopsy samples, which were also subjected to additional testing, which will be discussed later. First, since it was the aspect of this study that caught my attention (and that of other scientists), I’m going to look at the results of the whole genome expression profiling. For those of you not familiar with this technique, it basically involves simultaneously measuring the levels of messenger RNAs (mRNAs) for every known gene in the genome. This is done by hybridizing the total mRNA isolated with probes designed to bind to each mRNA coded by the genome. These probes are housed on a chip, and the binding (or lack of binding) can be read by the machine. It’s all very complicated, with several probes designed for normalization, but when it’s done the results of each chip can be compared to other chips, and the results are usually reported as log2 results (i.e. “1” means a two-fold difference between control and experimental; “2” a four-fold difference, etc., with negative numbers meaning a decrease by the same factor). Ten years ago these cDNA microarrays, as they’re called, were state of the art. They aren’t now. Next generation sequencing (NGS) techniques, such as RNAseq, are, but that doesn’t mean cDNA microarrays aren’t still useful. NGS probably would have been overkill for this study—or at least prohibitively expensive.
One thing that I immediately noticed about this study is that it didn’t exactly use what is state-of-the-art analysis techniques on the data that were generated. Basically, they analyzed their data pretty much the same way I analyzed microarray data back in 2005, which was to look at single genes that had the most profound increase or decrease in expression compared to control. In this case, each subject served as his own control because these were muscle biopsies done before and after massage therapy or control intervention (i.e., no intervention). These days, more sophisticated analyses, known as network analyses, are usually done. These involve looking for groups of genes that are turned on and off in synchrony that indicate broader pathways that are being turned on and off. Single genes don’t actually mean all that much. It’s the groups of genes going up and down together as part of a pathway that truly indicate specific pathways being turned on and off. To get an idea of what these sorts of analyses look like, check out Figure 5 in this paper. Instead, what we get is a circa 2005 gene list not unlike the ones I produced (click for full size):
The first thing I noticed about this list is that it’s a short list, particularly compared to the number of genes that changed in response to exercise:
Independent of the massage treatment, the control leg muscle exhibited a change in 943 probes (representing 592 genes) at 0 hours after massage (30 min after exercise) and 2307 probes (representing 1309 genes) at 2.5 hours after massage (3 hours after exercise), significant changes that were induced by exercise alone (tables S1 and S2).
In other words, these five genes were a tiny subset of the genes altered by exercise to exhaustion. Less impressive is that none of them were particularly strongly turned on or turned off. The gene most turned on only reached a level 1.68 times control at time zero after massage and was not detectably different from control by 2.5 hours. The gene most turned off only decreased to 0.73 times control, a 27% decrease. Not impressive, at least not to me. This was particularly true after I perused the supplemental data list, in which I found a whole bunch of genes whose expression appeared to change more than this, due to exercise. Unfortunately, the authors didn’t include the table I really wanted to see, namely the table doing the head-to-head comparison of massage versus no massage.
Now, let’s see what the authors said about the identity of the genes whose mRNA levels changed:
One of the five genes whose expression was altered by massage immediately after the treatment was functionally related to actin dynamics (filamin B, b) (Table 1). One of the four genes induced by massage after recovery from treatment (2.5 hours) was related to NFκB nuclear trafficking (nucleoporin 88) (Table 1). Overall, this profile suggested that massage altered processes related to the cytoskeleton the former process being activated early after massage and the latter induced later in recovery.
I found this very questionable based on my own experience analyzing a cDNA microarray. The reason is that what I found my gene of interest to do was to decrease nuclear factor-κB (NF-κB) signaling. I’ve also done studies looking at the nuclear localization of NF-κB using confocal microscopy and NF-κB. When NF-κB is activated or turned off in my experience the changes seen in whole-genome expression profiling assays are not subtle and do not involve just a single gene, like nucleoporin, whose messenger RNA was elevated (but, it should be noted, whose protein was never verified to be also elevated after massage). NF-κB changes the activity of dozens of genes in a pattern that’s so obvious that when I showed my initial microarray results to an NF-κB expert several years ago, he immediately recognized that pattern by “eyeballing it” (and now I can recognize that pattern too). The changes were also much more dramatic. Indeed, I was looking at fold-changes that ranged from two-fold to over a hundred-fold. While it is true that I was studying cultured cells, which are an inherently less noisy system than tissue biopsies, I would have still expected to see a lot more genes altered if massage were truly impacting inflammation in general and the NF-κB signaling pathway in particular.
So how did Crane et al. come to the conclusion that NF-κB was being affected? Basically, they observed that nucleoporin 88 was expressed at an increased level on the cDNA microarray. If that were truly related to NF-κB signaling in stressed muscle, we would expect that massage would increase, not decrease, NF-κB signaling because nucleoporin facilitates the entry of the NF-κB into the nucleus. Increased expression of nucleoporin 88 is associated with increased NF-κB activity, and depleting nucleoporin 88 results in decreased NF-κB signaling. Now, to be fair, the authors did follow up by measuring NF-κB level in the nucleus and found that nuclear NF-κB levels did appear to decrease at T=0 after massage but that by 2.5 hours there was no significant difference. This actually doesn’t really correlate with the changes in nucleoporin, which didn’t increase until 2.5 hours. To try to bolster their case, Crane et al. also looked at heat shock proteins and saw a decrease at 2.5 hours. They also looked at another inflammatory cytokine and noted a truly unimpressive decrease that was statistically significant at 2.5 hours. Finally, they saw an even less impressive decrease in tumor necrosis factor (another inflammatory cytokine) at 0 hrs that was statistically significant but was not significant at 2.5 hr. In other words, the data are not entirely consistent, nor is the magnitude of the decrease in inflammatory factors impressive or persistent. The authors might be correct in their interpretation, but what I see more than anything else is probably either noise or a mild effect that is probably not clinically significant.
Interestingly, contrary to many of the other claims made by massage therapists, anabolic signaling and muscle metabolites, such as lactate, macroglycogen, proglycogen, and total glycogen were unaffected by massage. So much for the idea of “washing out toxins” that we sometimes hear.
O Mitochondria, Mitochondria, wherefore art thou, mitochondria?
Finally, the authors looked at another signaling molecule, nuclear peroxisome proliferator–activated receptor γ coactivator 1α (PGC-1α), because they found evidence that upstream signaling pathways that activates PGC-1α were turned on by massage (hmmm, I have to be more careful about how I phrase things). Sure enough PGC-1α levels were slightly increased (by maybe about 20% to my eyeballing the graphs) at 2.5 hours after massage. However, contrary to the way some news outlets reported this story, the number of mitochondria did not increase. Worse, this is a misstatement promoted by Dr. Melov himself:
Buck Institute faculty Simon Melov, PhD, was responsible for the genetic analysis of the tissue samples. “Our research showed that massage dampened the expression of inflammatory cytokines in the muscle cells and promoted biogenesis of mitochondria, which are the energy-producing units in the cells,” said Melov. He added that the pain reduction associated with massage may involve the same mechanism as those targeted by conventional anti-inflammatory drugs. “There’s general agreement that massage feels good, now we have a scientific basis for the experience,” said Melov.
Uh, not quite. This paper doesn’t show that massage promotes biogenesis of mitochondria, only that massage might—I repeat, might—increase the level of one molecule that promotes the development of mitochondria by 20% at most. Paul Ingraham put it very well in his own article about this research:
What the authors actually reported is: “potentiated mitochondrial biogenesis signaling” and “promotes mitchondrial biogenesis.” In other words, they didn’t find more mitochondria … they found a mitochondrial growth signal. It’s the difference between finding bigger plants or just some bags of fertilizer.
Whether or not mitochondrial growth actually happens probably depends on many biological inputs, like everything else that our cells do. Inferring from one signal in a small sample that “massage increases mitochondria” is really just an enormous leap. Fortunately, the authors themselves didn’t make that leap — but lots of other people are making it.
Except that at least one of the investigators certainly is implying it very strongly—so much so that it’s a claim appearing in mainstream news articles about the study as though it were fact. As Paul also points out, the very design of this study indicates a lack of clinical insight into how massage therapy is usually used in the real world. What Crane et al. were studying was acute muscle injury in response to exercise to the point of exhaustion. Massage is not often used for that, and, in fact, as he summarizes, we already know that massage has only at best modest effects on exercise recovery; i.e., there isn’t much of a clinical benefit to explain. Rather, massage tends to be used used for chronic soreness. In fact, it might well be that a vigorous massage after a workout to the point where one’s muscles are so exhausted that one can’t even pedal a bicycle anymore would actually be painful.
When interesting results are oversold
My quibbles about the ethics of this study aside (well, they’re more than quibbles), scientifically this is not a bad study. However, as is so often the case in CAM studies, it is in the interpretation of the results that the authors go astray. They try to make something out of a mere five genes compared to hundreds that are changed by exercise when there doesn’t appear to be much to see. (In fact, my guess is that if they did a network analysis, the effect they observed would probably disappear into statistical insignificance.) They infer the wrong conclusion from the observation that nucleoporin 88 messenger RNA is elevated in muscle after massage. The correct inference would be to predict that NF-κB signaling should be elevated after massage, because nucleoporin 88 is involved in bringing NF-κB protein complex into the nucleus, where it does its stuff and turns on all the genes it turns on, which is why shutting down nucleoporin 88 inhibits NF-κB signaling. Yet they found that NF-κB signaling wasn’t increased but was rather decreased. Moreover, if the alterations in NF-κB signaling were significant, then there should have been a whole lot more than just a rather unremarkable change in the level of nucleoporin 88 messenger RNA. There should have been dozens of NF-κB target genes changing their levels in tandem because of NF-κB activation. There weren’t. Thus, the proper conclusion of this study is that there was little or no significant effect in inflammation-related gene expression from massage. That would have been perfectly fine as a conclusion. After all, negative studies happen and should be published.
Yet that’s not what was concluded. They did not report what was in essence a negative study.
Instead, the authors concluded that they had found that massage was anti-inflammatory, and that that’s how it “works.” They concluded that it “promoted mitochondrial biogenesis” without showing any evidence for anything other than the thinnest of thin evidence, a small increase in one signaling protein that promotes mitochondrial formation. And the news media ate it up.
None of this is to say that massage is useless or that it might not have therapeutic benefit in some circumstances. What this is to say is that this study, contrary to how it’s being portrayed, is not slam-dunk evidence that massage is some sort of “non-drug” treatment for inflammation that can replace non steroidal anti-inflammatory drugs. Unfortunately, whether because the authors were naive or desperate to salvage something from a study that didn’t show very much, that’s not how it was sold. The media might be guilty of overselling this study, but at least one of the authors was either complicit or didn’t realize how his words would be represented. Now this study is out there; look for massage therapists who are into woo to be pointing to this study for years to come as “proof” that massage is anti-inflammatory and “regenerates mitochondria.”