If there’s one thing I’ve become utterly disgusted with in the time since I first became interested in science-based medicine as a concept, its promotion, and the refutation of quackery and medical pseudoscience, it’s empty-brained celebrities with an agenda. Be it from imbibing the atmosphere within the bubble of woo-friendly southern California or taking a crash course at the University of Google and, through the arrogance of ignorance, concluding that they know more than scientists who have devoted their lives to studying a problem, celebrities believing in and credulously promoting pseudoscience present a special problem because of the oversized soapboxes they command. Examples abound. There’s Bill Maher promoting anti-vaccine pseudoscience, germ theory denialism, and cancer quackery on his show Real Time with Bill Maher and getting the Richard Dawkins Award from the Atheist Alliance International in spite of his antiscience stances on vaccines and what he sneeringly calls “Western medicine.” Then there are, of course, the current public faces of the anti-vaccine movement, Jenny McCarthy and her boyfriend Jim Carrey, the former of whom thinks it’s just hunky dory (or at least doesn’t appear to be the least bit troubled) that her efforts are contributing to the return of vaccine-preventable infectious diseases because she apparently thinks that’s what it will take to make the pharmaceutical companies change their “shit” product (her words), and the latter of whom spreads conspiracy theories about vaccines and contempt on people suffering from restless leg syndrome. Finally, there’s the grand macher of celebrity woo promotion, Oprah Winfrey, who routinely promotes all manner of medical pseudoscience, be it “bioidentical” hormones, the myth that vaccines cause autism (even hiring Jenny McCarthy to do a blog and develop a talk show for her company Harpo Productions), or other nonsense, such as Christiane Northrup urging Oprah viewers to focus their qi to their vaginas for better sex.
Unfortunately, last week the latest celebrity know-nothing to promote health misinformation released a brand new book and has been all over the airwaves, including The Today Show, Larry King Live, and elsewhere promoting it. Yes, I’m talking about Suzanne Somers, formerly known for her testimonial of having “rejected chemotherapy and tamoxifen” for her breast cancer, as well as her promotion of “bioidentical hormones,” various exercise devices such as the Thighmaster and all manner of supplements. Her book is entitled Knockout: Interviews with Doctors Who Are Curing Cancer–And How to Prevent Getting It in the First Place. It is described on the Random House website thusly:
In Knockout, Suzanne Somers interviews doctors who are successfully using the most innovative cancer treatments–treatments that build up the body rather than tear it down. Somers herself has stared cancer in the face, and a decade later she has conquered her fear and has emerged confident with the path she’s chosen.
Now she shares her personal choices and outlines an array of options from doctors across the country:
EFFECTIVE ALTERNATIVE TREATMENTS
- without chemotherapy
- without radiation
- sometimes, even without surgery
INTEGRATIVE PROTOCOLS
- combining standard treatments with therapies that build up the immune system
METHODS FOR MANAGING CANCER
- outlining ways to truly live with the diease
Since prevention is the best course, Somers’ experts provide nutrition, lifestyle, and dietary supplementation options to help protect you from getting the disease in the first place. Whichever path you choose, Knockout is a must-have resource to navigate the life-and-death world of cancer and increase your odds of survival. After reading stunning testimonials from inspirational survivors using alternative treatments, you’ll be left with a feeling of empowerment and something every person who is touched by this disease needs…HOPE.
I first found out about Somers’ book about a month and a half ago and was fortunate enough (I think) that one of my readers who had a review copy of the book sent me a chapter list. The reason I wanted a chapter list was because I was really curious just who these doctors were whom Somers had interviewed. In particular, back then I predicted (and hoped) that one of the doctors would be one whom we’ve met before. It was. Can you guess which one? Think about it. What major study did I blog about in the middle of September? What form of cancer quackery has been covered so ably by Kimball Atwood since the very beginning of this blog? No, no, you don’t have to go back to the archives and search. I’ll tell you:
Dr. Nicholas Gonzalez. He’s the second featured doctor who is “curing cancer,” right there in Somers’ book in Chapter 6!
That’s right, one of these doctors who are “curing cancer” is a quack (in my opinion, of course) whose “protocol,” which includes 150 supplement pills a day topped off by a couple of coffee enemas per day, was recently shown to be worse than useless for pancreatic cancer and, indeed, based on a recent study, far worse than conventional treatment.
From my perspective, it was incredibly bad timing and bad luck on Somers’s part to have one of the subjects she lionized in your book to have his protocol shown to be not just worthless, but likely actively harmful, a mere two months before the release of her book. In case there are any journalists who might be interviewing Somers and are interested in more than a puff piece that lets her promote her book, I list all the posts on Science-Based Medicine that have discussed the rank pseudoscience that is the Gonzalez protocol because, as many of you have figured out, I’m never satisfied with a hammer to smack down a form of woo when going nuclear is so much more fun:
- “Gonzalez Regimen” for Cancer of the Pancreas: Even Worse than We Thought (Part I: Results)
- “Gonzalez Regimen” for Cancer of the Pancreas: Even Worse than We Thought (Part II: Loose Ends)
- Tom Harkin, NCCAM, health care reform, and a cancer treatment that is worse than useless
- Cancer Quackery is Dangerous – The Gonzalez Treatment
- The Ethics of “CAM” Trials: Gonzo (Part I)
- The Ethics of “CAM” Trials: Gonzo (Part II)
- The Ethics of “CAM” Trials: Gonzo (Part III)
- The Ethics of “CAM” Trials: Gonzo (Part IV)
- The Ethics of “CAM” Trials: Gonzo (Part V)
- The Ethics of “CAM” Trials: Gonzo (Part VI)
- The “Gonzalez Trial” for Pancreatic Cancer: Outcome Revealed
Sadly, this bad timing appears to have had no effect whatsoever on the publicity blitz of an actress who every day tries to live down to the character she played on Three’s Company back in the 1970s or on the questions asked of her by interviewers. Somers has been all over the media this week, and I’ve seen nary a challenging question stronger than pointing out that some of the doctors featured in Somers’ book have gotten in trouble with their state medical boards, much less a much deserved question about Nicholas Gonzalez. Instead we’ve thus far been treated to cliched, credulous headlines like Suzanne Somers questions chemo in new book, Somers’ New Target: Conventional Cancer Treatment, or Suzanne Somers works to ‘Knockout’ cancer. The article circulating about her book on the AP wire begins:
Less than a year after the former sitcom actress frustrated mainstream doctors (and cheered some fans) by touting bioidentical hormones on “The Oprah Winfrey Show,” she’s back with a new book. This one’s on an even more emotional topic: Cancer treatment. Specifically, she argues against what she sees as the vast and often pointless use of chemotherapy.
Somers, who has rejected chemo herself, seems to relish the fight.
Let’s get one thing straight here. It is most definitely not, as implied by various articles about Somers, in any way amazing that Somers is still alive after having “rejected chemotherapy.” As I explained at the dawn of this blog, Somers had a stage I tumor with a favorable prognosis. If Somers is going to play the gambit of repeating, “I rejected chemotherapy and tamoxifen and I’m still alive” and attributing her survival to the alternative medicine woo she chose instead, perhaps now is the time to go into more detail than I’ve ever gone into before about her case. Well, not quite. I did go into quite a bit of detail in my talk at the Science-Based Medicine Conference at TAM7 in July. After all, I did the research; so I might as well get some more use out of it and spread it beyond the 150 or so people who heard my talk.
Prelude by flashback: Suzanne Somers’ breast cancer
In preparation for my talk at TAM7, I searched for all the information I could find that was publicly available about Suzanne Somers’ diagnosis of breast cancer back in 2000. For your edification, I’ve also uploaded the slides from my presentation relevant to Suzanne Somers’ breast cancer diagnosis as a PDF file. Suffice it to say, there is a great deal of misunderstanding of breast cancer in Somers’ testimonial. In this case, I don’t actually blame Somers all that much for her misunderstanding, because it is a very common misunderstanding that clearly derives from a misunderstanding of the difference between using chemotherapy for primary treatment of cancer versus adjuvant treatment of cancer. In early stage breast cancer, which can be surgically removed for cure, chemotherapy and radiation therapy are in general used as additional therapies that decrease the risk of recurrence of the cancer after surgery. That’s what adjuvant therapy is, extra therapy that improves a patient’s odds of surviving after a primary treatment. In the case of early stage breast cancer, the primary treatment is surgery.
From what I can find from publicly available information on the Internet (I’ve never read one of Suzanne Somers’ books), at age 54 Somers was diagnosed with a breast cancer that was treated by lumpectomy (excision of the “lump” or tumor) and a sentinel lymph node (SLN) biopsy, the latter of which was negative for tumor cells in the SLN, plus radiation therapy. For those not familiar with the SLN procedure, it is a procedure that developed in the 1990s to determine whether a woman’s breast cancer has spread to the axillary lymph nodes (the lymph nodes under the arm) without actually removing all of the axillary lymph nodes. Before the advent of SLN biopsy, the standard of care was to do an axillary dissection (removal of all the lymph nodes under the arm) on the side of the tumor in order to determine if and how many of the lymph nodes are positive for cancer. This is critical information, because the single most powerful prognostic indicator for potentially curable breast cancer (i.e., breast cancer that has not spread beyond the axillary lymph nodes to the rest of the body, such as bone, liver, or lung) is the presence of metastases in the axillary lymph nodes and, if they are present, how many. Unfortunately, as less invasive means of treating breast cancer were developed, such as lumpectomy, the part of the operation that carried the most morbidity was the axillary dissection. Consequently, as science-based physicians are wont to do, during the 1990s surgeons tried to find a way to get the same information (are the lymph nodes positive or negative) with a less morbid procedure and thus reserve axillary dissection only for patients who do have lymph nodes with breast cancer metastases in them.
Thus, the SLN biopsy was developed as a strategy to decrease the possibility of the most feared complication of axillary dissection, lymphedema, and still get the necessary information regarding lymph node positivity or negativity. Basically, an SLN biopsy is preformed by injecting both a radioactive dye and a blue dye (usually Lymphazurin Blue) into the breast. The dyes are then taken up in the lymphatics and head towards the axilla, where they lodge in one or more lymph nodes. This is (these are) the sentinel lymph node(s). The concept behind the procedure is that the sentinel node is the first lymph node a tumor cell that broke off from the tumor and got into the lymphatics will “see” and lodge in. In other words, the dye mimics the pathway that tumor cells take to metastasize to the axillary lymph nodes. If the sentinel node is negative, it’s an accurate indication that the rest of the lymph nodes are negative, and in general no further surgery is needed. Women are identified as node negative without removing all the axillary lymph nodes. Best of all, the risk of lymphedema from the procedure very, very small, far smaller than it is for axillary dissection (removing all the lymph nodes). Since the purpose of axillary dissection was far more diagnostic (to find out if the lymph nodes are contain tumor and, if so, how many), this is a good thing. On the other hand, if the SLN contains tumor, then axillary dissection is needed. In fact, far fewer women now undergo the procedure than in the past, and it is even coming under question whether a woman with a positive SLN truly needs a full axillary dissection.
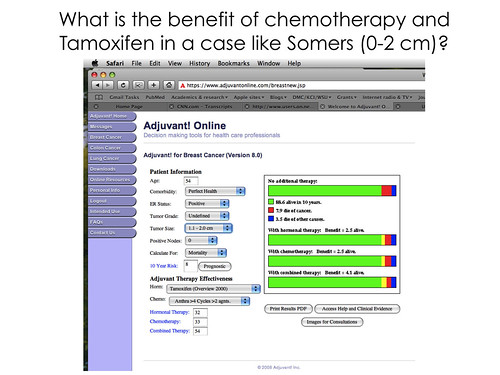
Why do I mention this? Because I want readers to understand that Somers underwent, as far as I can tell, standard surgery for a favorable, estrogen receptor-positive stage I cancer. She also underwent radiation, although she has stated in the past and now states in Knockout that, if she had it all to do over again, she would not have opted for radiation. Be that as it may, she has been trumpeting proudly for a number of years that she rejected chemotherapy and tamoxifen and has done quite well. This claim, although true, says nothing about whether he decision to eschew those adjuvant therapies was a good one and even less about whether the woo she pursued after that had anything to do with her survival. As I described so long ago, however, surgical excision is curative for most small breast cancers. Radiation therapy reduces the risk of local recurrences (recurrences in the breast), and chemotherapy and antiestrogen therapy (like Tamoxifen) reduce the risk of systemic recurrences (recurrences elsewhere in the body). In other words, chemotherapy and radiation are “icing on the cake” after surgery. Indeed, there is a website known as AdjuvantOnline.com that allows physicians to calculate the estimated risk of recurrence and the estimated benefit of chemotherapy and, if appropriate, antiestrogen therapy. Given when Somers had her cancer diagnosed (2000) and because I know that she had a stage I tumor, i entered data for her assuming a tumor between 1-2 cm in size, mainly because most tumors under 1 cm would not warrant adjuvant chemotherapy. Here is a blowup of the key slide from my talk where I showed the results I got when I entered the known information about Suzanne Somers’ tumor into AdjuvantOnline:
(Click for a larger image.)
As you can see, based on what we know from publicly available sources, Somers had an 88.6% chance of living 10 years without any chemotherapy or Tamoxifen. Chemotherapy provides a survival advantage of 2.5%; tamoxifen, 2.5%; and combination therapy, 4.1%. In other words, eschewing chemotherapy and tamoxifen increased Suzanne Somers’ odds of dying of her cancer within 10 years by around 4%, not a huge number. As I’ve explained before, although the benefit of chemotherapy and tamoxifen for early stage breast cancer is around 30% on a relative basis, but it’s only around 4% or 5% on an absolute basis. You may think that’s not very much, but, I assure you, the vast majority of women are willing to undergo chemotherapy and hormonal therapy for that extra insurance. Indeed, I would point out that surveys I have seen have revealed that a majority of women would still opt for chemotherapy even if it provided only a 1% absolute survival benefit. Moreover, for more advanced tumors, that relative benefit generally stays around 30% or so, meaning that, as the risk of dying from cancer goes up, the absolute benefit of adjuvant chemotherapy goes up as well. Be that as it may, I’ve laid out this information to point out that testimonials like Somers’ are not particularly impressive if you know something about breast cancer. I also mention it to point out that, even though it’s a bad idea for Somers to be pumping herself full of “bioidentical hormones,” the favorable nature of her tumor means that she can get away with it. Even if it increased her risk of recurrence by 10 or 20%, the odds of survival would still be overwhelmingly in her favor, adjuvant chemotherapy and tamoxifen or not, thanks to her friendly neighborhood surgeon. So when you see a passage like this about Somers, remember what I’ve just told you:
Diagnosed with breast cancer a decade ago, she had a lumpectomy and radiation, but declined chemotherapy, as she did more recently when briefly misdiagnosed with pervasive cancer.
As I said before, Somers’ misunderstanding of the role of adjuvant therapy in breast cancer is somewhat understandable. It is a concept that can be difficult to communicate this to patients under the best of circumstances, and the absolute benefit of chemotherapy in treating a stage I ER(+) cancer is relatively small. Moreover, treatment paradigms change with new scientific evidence. Most women these days with a stage I ER(+) tumor would undergo Oncotype DX® testing, and the results of that testing would guide the decision of whether chemotherapy is recommended or not. Oncotype DX did not exist in 2000, and adjuvant chemotherapy was recommended for the vast majority of women with a stage I breast cancer with a tumor greater than 1 cm in diameter.
Somers’ second testimonial, however, is not as forgivable as the first, which is actually only somewhat forgivable, given how aggressively Somers has used her own testimonial to promote “alternative” medical treatments such as mistletoe extract (which may have some anti-tumor activity but the evidence is very weak–more on that perhaps in a future installment). It reveals such a profound ignorance of what she herself is recommending to women for their “health” that, as a breast cancer surgeon dedicated to providing only the best science-based surgical and medical care to my patients, I must call her out for it.
Knockout: Suzanne Somers’ “whole body cancer” scare
I do not yet have my promotional copy of Knockout, although, I’m assured, it’s on the way. I had debated whether to wait until I had read it to write about the book, but then last week I saw this interview with Ann Curry:
Visit msnbc.com for Breaking News, World News, and News about the Economy
It was also pointed out to me that Chapter 1 of Knockout is available online at the Random House website. It’s entitled A Cancer Story–Mine. I read it and was appalled at the degree of misinformation being discussed right there in the very first chapter of the book, so much so that I started to doubt whether it was such a good idea of me to get a copy of the whole book and do a review on it. Still, I’m made of fairly stern stuff, and Somers is out there promoting the hell out of this book; so I feel that it’s my duty to look critically at the story she begins her book with. Suffice it to say, after I read Chapter 1, I was left shaking my head that anyone would listen to Suzanne Somers about cancer or any other health issue, so deep is the ignorance and so strong the distrust of “Western medicine.” Somers starts out her book by describing a cancer scare. Specifically, she describes an incident in which she was brought to the hospital with what sounds like an anaphylactic reaction of some sort and was misdiagnosed with what she calls “full body cancer.”
Before I go on, let me say right here that I do not mean to denigrate or otherwise downplay the seriousness of what happened to Somers, nor do I mean to cast doubt on the veracity of her story. At the very least, Somers appears to believe what she is saying, and it is quite possible that she was misdiagnosed with widespread metastasis from her breast cancer. I also don’t want to under estimate how much it probably scared her. Imagine yourself having survived breast cancer and then, eight years later, being admitted to a hospital for something else and being told that you had widespread metastases. It’s a horrible thing, if it really happened the way Somers said it happened, and it’s the sort of experience that would terrify anyone.
Color me somewhat skeptical, however.
Certain elements of Somers’ story sound a bit fishy. First off, Somers declines to identify the hospital. Right at the outset, I wondered why that is and can guess at a couple of likely reasons. First, perhaps she’s worried about being sued. Of course, if you’re a celebrity and the truth is on your side you probably don’t have much worry about being sued. In such a case, it’s far more likely that the entity suing would get the worst of it, at least as far as negative publicity. More likely, Somers knows that, whatever hospital she had been admitted to and whatever doctors had cared for her, patient confidentiality and HIPAA law prevent the hospital and doctors from discussing her case–or even admitting that Somers was ever a patient. Indeed, neither the hospital nor any of the health care professionals involved with Somers care can discuss her case without her explicit permission. Their hands are completely tied, and Somers can write and say whatever she wants without fear that anyone will contradict her. That’s why it disturbs me that no one who has interviewed Somers yet has asked her a handful of very obvious–and inconvenient–questions based on the anecdote in Chapter 1, namely:
- At what hospital were you hospitalized and when?
- Who were your doctors?
- Will you release some of your medical records and allow your doctors to speak about your hospitalization?
- If not, why not?
These are questions that need be asked in addition to questions about Somers’ support for Nicholas Gonzalez, whose pancreatic cancer “protocol” was recently shown to be worse than useless, but I have yet to see anyone ask her these questions.
Now, on to Chapter 1:
I wake up. I can’t breathe. I am choking, being strangled to death; it feels like there are two hands around my neck squeezing tighter and tighter. My body is covered head to toe with welts and a horrible rash: the itching and burning is unbearable.
The rash is in my ears, in my nose, in my vagina, on the bottoms of my feet, everywhere — under my arms, my scalp, the back of my neck. Every single inch of my body is covered with welts except my face. I don’t know why. I struggle to the telephone and call one of the doctors I trust. I start to tell him what is happening, and he stops me: “You are in danger. Go to the hospital right now.” I knew it. I could feel that my breath was running out.
Right off the bat, to me Somers’ symptoms sound like an allergic reaction to something or an anaphylactic reaction. It could be something else (more later), but the first thing that comes to mind is an allergic reaction. Indeed, upon hearing this story, I couldn’t help but wonder if one of the many supplements that Somers takes on a routine basis was the cause. Did she start any new supplements recently? Certainly I’d wonder about that. (Again, more on that later; my speculation may well have been correct, just not in the way I thought at first.) Regardless of the initial cause, it certainly sounded as though the E.R. docs at whatever hospital Somers was brought to thought she was having some sort of allergic reaction. Based on that, they treated her appropriately with Benadryl, Albuterol, and steroids. Even someone as medically ignorant as Somers realized the most likely diagnosis:
I say to the doctor, “It seems to me that I’ve either been poisoned or am having some kind of serious allergic reaction to something. I mean, doesn’t that make sense? The rash, the strangling, the asphyxiation. Sounds classic, doesn’t it?”
“We don’t know. A CAT scan will tell us. I really recommend you do this,” the doctor says. “Next time you might not be so lucky — you might not get here in time. You were almost out.”
As I read this part of the story, I was puzzled, and certainly Somers didn’t initially give enough information for me to hazard a particularly educated guess about why her doctor ordered a CT scan. After all, a CT scan is not generally the test of choice for diagnosing the cause of anaphylaxis or respiratory distress, which is what it sure sounds as though Somers was being treated for. On the other hand, maybe doctors saw a mass on chest X-ray (quite likely, as we will soon see). They may also have suspected a pulmonary embolus (PE), for which chest CT has supplanted the older test previously to detect PE, namely the V-Q scan. There may have been other findings on physical examination that suggested that a CT scan might be indicated. (There almost certainly were.) Again, initially, at least, Somers doesn’t give us enough information to judge. She does, however, engage in typical pseudoscientific thinking. While acknowledging that those evil pharmaceuticals had saved her life, still she can’t help but attack them:
I am now dressed in a blue hospital gown, and so far I’ve been reinforced by three rounds of oxygen and albuterol. I’m starting to feel normal again. Drugs have been my lifesaver this time. This is what they are for. Knowing the toxicity of all chemical drugs, I’ve already started thinking about the supplement regime and detox treatments I’ll have when I get out of here, to get all the residue of pharmaceuticals out of me. I’m hopeful this will be the one and only time I have to resort to Western drugs.
Remember, whenever you hear an alt-med maven say “Western medicine” (shades of Bill Maher!), what that alt-med maven is really referring to is science-based medicine. As for supplements, if they have anything in them that does anything physiological, they contain “chemical drugs.” There is no difference between “chemical drugs” found in pharmaceuticals and “chemical drugs” found in supplements, other than that the drugs found in supplements are adulterated with all sorts of stuff. There is no magical difference between the two. They both contain chemicals, and the body responds to chemicals through its biochemistry. Nothing makes supplements magically immune to the laws of physics and chemistry. Moreover, “detox” treatments are completely unnecessary quackery. Somers apparently doesn’t realize it, but her body is more than capable of “detoxing” away those evil “Western” pharmaceuticals through its own amazing abilities. Somers appears to think that “Western” pharmaceuticals somehow leave their taint behind. Maybe she thinks the cells in her body have a “memory” in the same way that homeopaths claim that water has “memory” and that the taint has to be somehow purged, just as a Catholic believes that confession purges sins or certain Muslim sects think that self-flagellation will purge them of their sins. It really is religious thinking more than anything else for Somers to think that she was somehow “contaminated” by “Western” pharmaceuticals and needed to have that “contamination” purged.
But I digress. So what did the CT scan find? This, apparently:
We have very bad news,” he continued. My heart started pounding, like it was jumping out of my chest. “You have a mass in your lung; it looks like the cancer has metastasized to your liver. We don’t know what is wrong with your liver, but it is so enlarged that it is filling your entire abdomen. You have so many tumors in your chest we can’t count them, and they all have masses in them, and you have a blood clot, and you have pneumonia. So we are going to check you into the hospital and start treating the blood clot because that will kill you first.”
We already know that Somers did not, in fact, have cancer. (Otherwise, it would not have been a misdiagnosis.) So what she did have, I’ll get to shortly. In the meantime, let’s take a look at what Somers says about her oncologist:
The oncologist comes into my room. He has the bedside manner of a moose: no compassion, no tenderness, no cautious approach. He sits in the chair with his arms folded defensively.
“You’ve got cancer. I just looked at your CAT scan and it’s everywhere,” he says matter-of-factly.
“Everywhere?” I ask, stunned. “Everywhere?”
“Everywhere,” he states, like he’s telling me he got tickets to the Lakers game. “Your lungs, your liver, tumors around your heart … I’ve never seen so much cancer.”
So the oncologist who saw Somers first was a world-class jerk. It’s quite possible. Not every doctor has a good bedside manner, and some have a horrendous bedside manner. Sadly, some of them are oncologists, even though, if there’s a specialty that really demands a good bedside manner, it’s that of medical oncologist. On the other hand, as physicians we have to remind ourselves all the time that what we think we have said to the patient is not always how the patient has heard it and how we come across to the patient is not always how we have, in fact, come across to the patient. Maybe the oncologist was that uncaring, maybe not. We have no way of knowing because all we have is Suzanne Somers’ report. Maybe it’s also true that the other oncologist who saw her was somewhat less of a jerk but just as quick to jump to a conclusion prematurely:
Then the lung cancer doctor enters the room. Maybe he has better news. But no—he says, “I just looked at your CAT scan, and you have lung cancer that has metastasized.” He is nicer, more thoughtful. “I mean, I’m going to think about this,” he says. “Maybe it’s something else, but this sure doesn’t look good. I’ll be back tomorrow.” Leslie takes out pen and paper and is making notes. She will continue to do this the entire week, writing down everything everyone is saying. Thank God, because when you are stunned and on medication, things get foggy.
Day one is almost over. The most shocking, devastating day of my life, our life! I know the facts: when you have lung cancer and it has metastasized to your liver, heart, abdomen, and all over your body, you have at most two months—maybe only two weeks or less.
As a possible bit of perspective, I’ll point out that not too long ago I had to relearn the lesson of how my perception of what I say to a patient may not always jibe with the patient’s perception of what I said. A while back, I saw a patient with breast cancer in her hospital room, a woman I had operated on the day before. I thought I had calmly laid out the situation, reassured her that her tumor was treatable, and told her that she might not need chemotherapy. About an hour later I got a frantic page from the floor. The patient was in tears, and the family was in an uproar. I don’t know how I had done it, but I had somehow given this patient the impression that her situation was hopeless and that she was going to die. When her family arrived to take her home she was crying. Apparently she had interpreted my telling her that she might not need chemotherapy (mainly because of her age and tumor characteristics) as telling her that it was pointless to treat her more. I relearned a valuable lesson that day, one I (and, I daresay, most doctors, no matter how experienced) need to relearn periodically, namely that patients don’t always interpret what I tell them the way I think they will and that sometimes how I view a conversation with a patient may be very different than how the patient viewed the conversation. Fortunately, I was able to reassure everyone and correct the misconceptions that had been left, but I did not feel too good about my bedside manner that day. In fact, the rest of that day I felt like the most insensitive, idiotic doctor in the world.
Or maybe Suzanne Somers’ oncologist was indeed a flaming jerk. That would be the worst case for “Western medicine” in this story, and it is not nearly as uncommon as I’d like to admit for a physician to have the personality of a paper cup or the bedside manner of bully. Besides, it’s easier to assume that that is how the oncologist in question treated Somers. Even so, in that case, I’d say, “So what?” I’m sorry that Somers’ oncologist treated her badly. There’s no excuse for that. I’d also tell her simply to go and get another oncologist or go back to her regular oncologist, which she ultimately did. One nasty doctor does not invalidate “Western medicine,” nor does the occurrence of a misdiagnosis, even one apparently this spectacular. In any case, it’s quite possible that there was a bit of Somers hearing things one way when her doctors weren’t telling it the way she interpreted them as telling her. The reason I say that is because Somers goes on and on, mainly in interviews but also in the book, about how, over six days, doctors told her she needed chemotherapy. As someone who has dealt with medical oncologists every day for over 10 years, that part of her story just didn’t seem very likely to me. The reason is that, in general, oncologists are very reluctant to administer chemotherapy to a patient in the absence of a definite tissue diagnosis proving that they have cancer, be it metastatic cancer or any cancer.
This would be doubly true in a case like what Somers describes in her book, particularly given that she had one oncologist thinking that she had lung cancer, not a recurrence of her breast cancer. In any case, widespread cancer could be a recurrence of her breast cancer (especially given Somers’ proclivity to pump herself full of “bioidentical hormones” after having been treated for an estrogen receptor-positive cancer), but in a 63-year-old woman, there are lots of other possible malignancies. Chemotherapy would be used for breast cancer might not work very well against, say, colon cancer or ovarian cancer, both of which are other likely possibilities in a woman of Somers’ age. Another reason I seriously question whether doctors were pushing hard for chemotherapy in a mere six days is because, if they truly thought she had such a massively widespread recurrence of her breast cancer, particularly an estrogen receptor-positive breast cancer, all treatment would be palliative. We can’t cure most metastatic solid tumors, and the first rule in treating stage IV disease is usually the classic “First, do no harm.” Thus, oncologists usually tend to do the minimum possible that it takes to relieve symptoms and (hopefully) slow the progression of the tumor. Most likely, if this was indeed metastatic breast cancer, an oncologist would have chosen to treat Somers first with an anti-estrogen drug, probably an aromatase inhibitor (no tamoxifen if she had blood clots causing that much trouble!) and then seen how she did. In the case of a woman who has ER(+) cancer recur as stage IV disease, that is almost always the first option. In such cases, chemotherapy is usually reserved for the case when antiestrogen therapy fails. Indeed, if the cancer was truly as widespread as Somers reports, chemotherapy might not even be used at all if the likelihood of success is tiny; in such cases, hospice would be recommended.
Be that as it may, the very first thing that any competent oncologist would demand before initiating chemotherapy is a tissue diagnosis, either from a needle biopsy or other tissue, to prove that there was cancer and to identify the type of cancer, so that the correct chemotherapy could chosen. Cancer chemotherapy is not like antibiotic therapy. In the case of infectious diseases, it is not uncommon to begin an antibiotic empirically based on the most likely organisms to be causing the infection and then to tailor the therapy to whatever organism(s) can be identified by cultures. Oncologists, on the other hand, are incredibly reluctant to treat metastatic cancer empirically, particularly cancer that appears to have recurred eight years after the original diagnosis of a stage I tumor. Such cancer might very well be a different cancer from a different organ, and the chance of doing harm with chemotherapy for no benefit is too great.
That’s why I thought right away that there’s something very fishy about Somers’ story. It just doesn’t add up very well. What I suspect to have happened is that perhaps the oncologist did have a conversation about a probable need for chemotherapy, and, like my conversation with my postoperative patient, Somers saw the conversation differently from how her doctors did. She probably viewed various “what if” scenarios or “if this is recurrent breast cancer, then you will need this” conversations as “pressuring” her to take chemotherapy. If her oncologist wasn’t particularly warm and fuzzy or patient, she might have been even more likely to interpret his recommendations that way. Or perhaps her oncologists were incompetent enough to pressure her to take chemotherapy without a diagnosis of biopsy-proven cancer. Who knows? Even if the latter is true, it still doesn’t excuse Somers’ horrible ignorance that becomes manifest later in the chapter.
Ultimately, Somers did get a biopsy. She describes it in her interview above, “They cut into my neck and went in and took a piece of my lung, a piece of one of the so-called tumors around my heart turned out it was not cancer at all.”
So what was it?
I’ll admit that my first guess, sarcoidosis, was dead wrong. Given the symptoms of skin lesions, shortness of breath, and, apparently, “tumors around the heart” (which could indicate either pericardial involvement, or, more likely enlargement of the paratracheal nodes), I didn’t think it too unreasonable a first guess. (Besides, in the cases in House, MD, sarcoidosis almost always appears on the differential diagnosis list.) However, never having lived in the southwest, having forgotten my medical school learning about common fungal infections, and being what I self-deprecatingly like to call a dumb surgeon, I didn’t consider what turned out to be the real diagnosis right away, namely valley fever, or, as it’s known by its official name, coccidioidomycosis. Indeed, the description of the most severe disseminated form of coccidioidomycosis matches Somers’ presentation quite well:
The most serious form of the disease, disseminated coccidioidomycosis occurs when the infection spreads (disseminates) beyond the lungs to other parts of the body. Most often these parts include the skin, bones, liver, brain, heart, and the membranes that protect the brain and spinal cord (meninges).
The signs and symptoms of disseminated disease depend on which parts of your body are affected and may include:
- Nodules, ulcers and skin lesions that are more serious than the rash that sometimes occurs with other forms of the disease
- Painful lesions in the skull, spine or other bones
- Painful, swollen joints, especially in the knees or ankles
- Meningitis — an infection of the membranes and fluid surrounding the brain and spinal cord and the most deadly complication of valley fever
Now here’s the kicker. Take a look at these two (out of several) risk factors for the most severe form of coccidioidomycosis:
- Weakened immune system. Anyone with a weakened immune system is at increased risk of serious complications, including disseminated disease. This includes people living with AIDS or those being treated with steroids, chemotherapy or anti-rejection drugs after transplant surgery. People with cancer and Hodgkin’s disease also have an increased risk.
- Age. Older adults are more likely to develop valley fever than younger people are. This may be because their immune systems are less robust or because they have other medical conditions that affect their overall health.
These are risk factors for the serious disseminated coccidioidomycosis. Most people who contract coccidioidomycosis are either asymptomatic or exhibit relatively mild symptoms. Indeed, valley fever often presents as a flu-like illness from which people recover rapidly. Many people, in fact, are unaware that they’ve ever had coccidioidomycosis until there’s either an abnormality on chest X-ray done for another reason or they have a positive skin or blood test. It’s very much like histoplasmosis right here in the Midwest. So why did Somers get such a serious case? It’s a legitimate question, given how she represents her regimen of supplements, bioidentical hormones, and various other woo as a highly effective path to rejuvenation and health that she recommends to her readers. Let’s see. Somers is 63, but apparently in good health. She also takes all sorts of supplements which, or so she claims, “strengthen the immune system.” But her immune system was obviously not strong enough to prevent her from getting disseminated coccidioidomycosis. Why didn’t all those supplements ward off the fungus? For someone who takes handfuls of supplement pills every day and makes millions of dollars selling woo to “boost the immune system,” Somers sure doesn’t appear to have a particularly strong immune system, as it failed miserably to protect her from a severe infection due to an endemic fungus that usually causes only mild disease or any symptoms at all but almost killed her.
Another possibility presents itself. As we know from her previous books and appearances on The Oprah Winfrey Show, Somers takes boatloads of “bioidentical” hormones. She promotes them as a fountain of youth for women. One wonders if any of her various supplements or bioidentical hormones were somehow adulterated with corticosteroids, which suppressed her immune system, one does. Or at least I do.
One need wonder no more. Right there, in Chapter 1 of her book, is a highly plausible, highly likely explanation for why Somers became as ill as she did from coccidioidomycosis:
Day 5. Dr. Oncologist comes into my room. Now, you would think he’d say, “Well, sometimes it’s good to be wrong.” Or “Isn’t it great that you don’t have cancer?” But no. He walks in, doesn’t sit down, just looks at me and says angrily, “Well, you should have told me you were on steroids.”
I am flabbergasted. I don’t know what to say to him; I am so stunned by his lack of compassion that I just stare at him. I am not on steroids. I would never take steroids. But because he is stuck in old thinking and so out of touch with new medicine, he has no clue and doesn’t understand cortisol replacement as part of the menopausal experience.
I don’t know where to begin with him. He’s too arrogant to listen to a “stupid actress,” anyway. So much of his attitude with me has been the unsaid but definite “So you think all your ‘alternatives’ are going to help you now, missy?”
Why steroids would have anything to do with being misdiagnosed with full-body cancer, I can’t guess. But we still don’t know what has gone wrong in my body. We still have to find out what caused me to end up in the ER.
(Emphasis mine.)
It’s incredibly hard at this point not to go even beyond Mark Crislip-grade acid sarcasm at the arrogance of ignorance on display. Here we have a woman who is apparently taking cortisol as part of her “bioidentical hormone” cocktail, and this woman does not know that each and every one of those estrogens she is taking is a steroid hormone. More importantly, Somers apparently does not know that cortisol is a corticosteroid (“cortico,” get it?), the very same kind of steroid that is routinely used by us evil reductionist practitioners of “Western medicine” as an anti-inflammatory and immunsuppressant. When used that way by us evil pharma shills, cortisol is known as hydrocortisone, which is–gasp!–a pharmaceutical concoction! It’s also “bioidentical,” too, proving once more that “bioidentical” does not mean “risk-free.” Indeed, hydrocortisone is often included as one of the drugs in immunusuppressive protocols used to prevent the rejection of organ transplants. Given that Somers has said that she takes enough “bioidentical” estrogens to recreate the hormonal milieu of a woman in her 20s (in other words, far more estrogens than a 63 year old woman would ever have or need), it’s not beyond the pale to wonder whether she similarly takes a significant dose of hydrocortisone (sorry, cortisol) as part of her brew of “bioidenticals,” particularly in light of her having fallen seriously ill due to an organism that usually causes mild disease in immunocompetent hosts. Yes, valley fever can sometimes be a bad disease in immunocompetent hosts, but being immunocompromised for whatever reason is still a significant risk factor for disseminated disease or the reactivation of quiescent disease.
After reading Somers’ story in Chapter 1, I shook my head in disbelief that Random House apparently didn’t have better editors who could have told Somers that she had just written something incredibly contradictory and just plain dumb when she wrote that didn’t take steroids in the context of writing how she castigated her oncologist for “not understanding” the role of cortisol in her menopause treatments. Also, based on Somers’ (or her ghostwriters’) own words in Chapter 1 of her book, I think I have discovered the most likely explanation for Somers’ contracting disseminated coccidioidomycosis. True, it could be that she was just unlucky and getting old, given that age is indeed a risk factor for disseminated disease, but one can’t ignore all the supplements she was taking. One can’t ignore that Somers was apparently taking cortisol as part of the cocktail of “bioidentical hormones” to recapture her youth. It is thus very reasonable to wonder whether the reason that Somers became so ill last year was because she had been chronically dosing herself with cortisol and suppressing her very own immune system. Worse, Somers doesn’t even understand that cortisol is a steroid and an immunosuppressant and therefore can’t accept or admit that this is a possibility. Indeed, that misunderstanding is leading her to view her misdiagnosis as clear evidence supporting her worldview that “Western medicine” is hopelessly flawed, chemotherapy rarely works, and the “alternative” medicine doctors whom she interviews can actually cure cancers that “Western” medicine cannot. Even worse still, Somers is successful enough to be able to parlay her suspicion into a highly lucrative career, and her promotion of dubious, unproven, and even ineffective medical treatments for cancer may well result in cancer patients who might be saved eschewing science-based medicine and endangering their lives. At least, that is what I fear.
A panoply of unproven treatments and what’s to come
As I said before, I plan on looking at Knockout and writing a more formal review once I get my copy to read. That’s why this post is labeled “Part 1.” However, so incensed was I at the rank pseudoscience and dangerous misinformation being promoted relentlessly over the past week by a woman who is apparently utterly ignorant of what a steroid hormone is or that steroids are immunusuppressive that I decided to do this post now, while Somers’ media blitz is still at its height. I concluded that an antidote to Somers’ promotion of nonsense such as the Gonzalez protocol needed to be provided in clear, concrete, unequivocal terms was needed now, that someone needed to express his opinion now that pseudoscience such as the Gonzalez protocol is quackery, particularly given the limp, woo-friendly response of Dr. Otis Brawley, chief medical officer for the American Cancer Society. His article, Somers’ cancer advice is risky, appeared on CNN.com. In it Dr. Brawley practically bent over backwards to be conciliatory, calling Somers a “wonderful actress” (she’s not and never has been), writing that he is “not critical of the concept of alternative and complementary medicine” (I am) and that “open-mindedness to other ideas is how we advance conventional medicine” (apparently his mind is so open that his brains threaten to fall out), even going so far as to invoke the hoary old alt-med examples of aspirin being derived from tree bark or vincristine being derived from a plant as though pharmacognosy were the same thing as herbalism. It’s not. Moreover, I wanted to provide a handy-dandy resource for journalists who may be interviewing Somers or people who may be seeing her at book signings or promotional events, hoping against hope that skeptics will ask her why she doesn’t think a steroid like cortisol wouldn’t predisopose her to disseminated coccidioidomycosis or why she thinks that Dr. Gonzalez is “curing cancer” when a clinical trial was published a mere two months before her book was released that showing clearly that his protocol is worse than useless and that pancreatic cancer patients undergoing conventional therapy live three times longer than those undergoing the Gonzalez protocol.
A guy can hope, can’t he?
In the meantime, here’s a chapter list, which will give you an idea of what you have to look forward to when I get around to reading the book:
The Doctors Who Are Curing Cancer
Chapter 5: Stanislaw Burzynski, M.D.
Chapter 6: Nicholas Gonzalez, M.D.
Chapter 7: Burton Goldberg
Chapter 8: Julie Taguchi, M.D.
Chapter 9: James Forsythe, M.D.Preventing Cancer Before it Starts
Chapter 10: Russell Blaylock, MD
Chapter 11: Steve Haltiwanger, MD
Chapter 12: David Schmidt
Chapter 13: Jonathan Wright, M.D.
Chapter 14: Steven Sinatra, M.D., F.A.C.C., F.A.C.N.
Chapter 15: Michael Galitzer
Chapter 16: Cristiana Paul, M.S.
Most names I actually don’t know, but some names stand out, such as Dr. Burzynski, whom we haven’t yet discussed much on this blog but should (reviewing this book will give me just that opportunity), and Dr. Blaylock, who is best known for videos like this about H1N1:
I’ll spare you parts 2 and 3 of Dr Blaylock’s video. You get the idea, and if you are masochistic enough top want to view them, you can easily find them on YouTube. Suffice it to say, showing up on Alex Jones’ Prison Planet TV is not exactly a way to burnish one’s scientific credentials. Jones’ websites, Infowars and Prison Planet, are repositories of conspiracy craziness on par with David Icke’s lizard people, including 9/11 Truthers, “New World Order” conspiracy theorists (including, of course, the Illuminati and the Rothschilds), and a heaping helping of anti-vaccine and alt-med conspiracy mongering. In fact, Dr. Blaylock isn’t too far from David Icke’s rant about how the swine flu vaccine is a plot by the Illuminati.
Such are Suzanne Somers’ “doctors who are curing cancer.”
The bottom line is that, whatever her intentions, whether they be to help people or make money or both, Somers is unwittingly promoting dangerous cancer “cures” that are anything but cures. They are treatments that are anything but science-based, as well. Just as Jenny McCarthy, Jim Carrey, and Bill Maher are promoting anti-vaccine pseudoscience to the nation and Oprah Winfrey is providing an unmatchable soapbox for all manner of promoters of woo, Somers is taking advantage of her position to bash conventional medicine and promote non-science-based medicine, most likely raking in the cash hand over fist.
People may well die as a result.