I see that the kerfuffle over screening for cancer has erupted again to the point where it’s found its way out of the rarified air of specialty journals to general medical journals and hence into the mainstream press.
Over the last couple of weeks, articles have appeared in newspapers such as the New York Times and Chicago Tribune, radio networks like NPR, and magazines such as TIME Magazine pointing out that a “rethinking” of routine screening for breast and prostate cancer is under way. The articles bear titles such as A Rethink On Prostate and Breast Cancer Screening, Cancer Society, in Shift, Has Concerns on Screenings, Cancers Can Vanish Without Treatment, but How?, Seniors face conflicting advice on cancer tests: Benefit-risk questions lead some to call for age cutoffs, and Rethinking the benefits of breast and prostate cancer screening. These articles were inspired by an editorial published in JAMA last month by Laura Esserman, Yiwey Shieh, and Ian Thompson entitled, appropriately enough, Rethinking Screening for Breast Cancer and Prostate Cancer. The article was a review and analysis of recent studies about the benefits of screening for breast and prostate cancer in asymptomatic populations and concluded that the benefits of large scale screening programs for breast cancer and prostate cancer tend to be oversold and that they come at a higher price than is usually acknowledged.
For regular readers of SBM, none of this should come as a major surprise, as I have been writing about just such issues for quite some time. Indeed, nearly a year and a half ago, I first wrote The early detection of cancer and improved survival: More complicated than most people think. and then followed it up with Early detection of cancer, part 2: Breast cancer and MRI. In these posts, I pointed out concepts such as lead time bias, length bias, and stage migration (a.k.a. the Will Rogers effect) that confound estimates of benefit due to screening. (Indeed, before you continue reading, I strongly suggest that you go back and read at least the first of the aforementioned two posts to review the concepts of lead time bias and length bias.) Several months later, I wrote an analysis of a fascinating study, entitling my post Do over one in five breast cancers detected by mammography alone really spontaneously regress? At the time, I was somewhat skeptical that the number of breast cancers detected by mammography that spontaneously regress was as high as 20%, but of late I’m becoming less skeptical that the number may be somewhere in that range. Even so, at the time I did not doubt that there likely is a proportion of breast cancers that do spontaneously regress and that that number is likely larger than I would have guessed before the study. Of course, the problem is that we do not currently have any way of figuring out which tumors detected by mammography will fall into the minority that do ultimately regress; so we are morally obligated to treat them all. My most recent foray into this topic was in July, when I analyzed another study that concluded that one in three breast cancers detected by screening are overdiagnosed and overtreated. That last post caused me the most angst, because women commented and wrote me asking me what to do, and I had to answer what I always answer: Follow the standard of care, which is yearly mammography over age 40. This data and these concerns have not yet altered that standard of care, and I am not going to change my practice or my general recommendations to women until a new consensus develops.
Before I discuss the JAMA analysis, let me just sample a bit of how this issue is being portrayed in the popular press:
- This week the conversation garnered national attention when physicians at the University of California, San Francisco, and University of Texas, San Antonio, published an analysis in the Journal of the American Medical Association expounding on their concerns about the ongoing harm inflicted on patients who undergo prostate and breast cancer screening. One problem is that screening often picks up harmless or non-life-threatening tumors that could have gone unnoticed for a lifetime, leading to unnecessary and aggressive treatment for patients. In the days before widespread mammography, for instance, physicians rarely encountered ductal carcinoma in situ (or DCIS), a type of low- to intermediate-grade breast cancer that grows slowly and may even regress, meaning that the body may rid itself of the tumor. But today DCIS accounts for nearly 30 % of all breast cancer diagnoses (more than 60,000 cases a year), leading to an untold amount of treatment and patient distress. (TIME Magazine)
- The purpose of screenings is to detect cancer early, when treatments are most likely to be effective, and to save lives. That the tests do so for colon, breast and cervical cancer has been well-established for middle-age adults but is not indisputable for those who are older, as most studies have been done in people younger than 65. Research on routine PSA screening has yet to prove a definitive benefit at any age. On the other side are the potential costs, which can include unnecessary treatments for cancers that never would have become life-threatening, the anxiety and distress associated with cancer diagnosis, the complications associated with screening procedures or therapies, and medical expenses. (Chicago Tribune)
- Call it the arrow of cancer. Like the arrow of time, it was supposed to point in one direction. Cancers grew and worsened. But as a paper in The Journal of the American Medical Association noted last week, data from more than two decades of screening for breast and prostate cancer call that view into question. Besides finding tumors that would be lethal if left untreated, screening appears to be finding many small tumors that would not be a problem if they were left alone, undiscovered by screening. They were destined to stop growing on their own or shrink, or even, at least in the case of some breast cancers, disappear. (New York Times)
- The American Cancer Society, which has long been a staunch defender of most cancer screening, is now saying that the benefits of detecting many cancers, especially breast and prostate, have been overstated. It is quietly working on a message, to put on its Web site early next year, to emphasize that screening for breast and prostate cancer and certain other cancers can come with a real risk of overtreating many small cancers while missing cancers that are deadly. (New York Times)
The latest kerfuffle is simply the latest bubbling up of a controversy that has been going on for years. It’s also a classic example of the difficulty of applying messy science to public health issues. Science is messy, but public health initiatives, to be successful, arguably need a simple message that resonates with the public, a message like
- Screening for cancer catches cancers at an earlier stage when they are more easily treated.
- Screening for cancer saves lives.
- You should get screened if you’re older than N years old.
Thus, when evidence that calls into question any of these messages appears, it causes consternation among the lay public. Worse, cranks leap to take advantage of such controversies and make claims, such as “mammography is useless” and publish cartoons like this. Even people who should know better say similar things. As I’ve said before, science-based medicine is hard and not always clear-cut. Moreover, I would argue that debates such as this demonstrate that the claims of cranks that physicians all march in lockstep or that there is a “conspiracy” to keep shortcomings of SBM from patients are nothing but the rankest nonsense. Finally, cranks often conflate, either through ignorance, willful ignorance, or often outright hostility to “Western medicine,” screening mammography with diagnostic mammography. Screening mammography is designed to detect disease in asymptomatic women. If a woman feels a suspicious lump, nothing–I repeat, nothing–in any of this data says that she should not have a physical exam and appropriate imaging, including mammography and ultrasound at the minimum, posthaste. That’s diagnostic mammography, and that is not what this kerfuffle is over. Suspicious lumps, especially in women over 40, need to be worked up, period. I can’t emphasize that strongly enough.
So what did Esserman et al say? They lay out the problem thusly:
A large fraction of the US population participates in screening for prostate cancer and for breast cancer. About 50% of at-risk men have a routine prostatespecific antigen (PSA) test and 75% have previously had a PSA test.3,4 About 70% of women older than 40 years reported having a recent mammogram.5 Two decades of screening have resulted in a significant increase in detection of early cancers. Prostate-specific antigen testing has nearly doubled the chance that amanwill be diagnosed with prostate cancer in his lifetime: In 1980, a white man’s lifetime risk of prostate cancer was 1 in 116; today it is 1 in 6.1 A woman’s lifetime risk of breast cancer was 1 in 12 in 1980; today it is 1 in 8.1 If ductal carcinoma in situ (DCIS) is included, the risk of being diagnosed with breast cancer, like prostate cancer, has almost doubled as well.
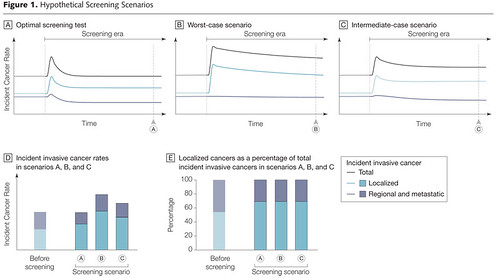
The increase in early cancers as a fraction of total cancers detected is not necessarily beneficial. The introduction of an optimal screening test should be followed by an increase in the rate of early disease followed by a decrease in regional disease while the overall detection rate remains constant.7 FIGURE 1 illustrates hypothetical optimal, worst case, and intermediate-case scenarios, using 1980 breast cancer incidence rates as a starting point. In the worst case, screening leads to an increase in local disease detection without a corresponding decrease in regional disease, thereby increasing costs and morbidity due to overdetection and overtreatment of non–life-threatening cancers.
They conclude that current screening protocols for breast and prostate cancer result in a case that is intermediate between the worst case and optimal case scenarios. Because their graph illustrates this problem better than words can, I present it here:
Esserman et al then point out that the incidence of early stage breast and prostate cancers has increased dramatically as a fraction of total cancers detected, while regional and metastatic cancers have decreased dramatically as a fraction of those cancers detected. One example is the form of breast cancer known as ductal carcinoma in situ, abbreviated DCIS. DCIS is considered to be breast cancer, but “pre-invasive” cancer, given that the sine qua non for its diagnosis is seeing cancerous-appearing breast epithelial cells confined within the ducts with no evidence of their having invaded through the basement membrane that separates the ducts from the surrounding tissue. Thus, DCIS has been labeled “stage zero” cancer, and its 5 year survival is close to 100%, although a small proportion of patients does recur and ultimately die of breast cancer. There is even a debate over whether DCIS truly represents a precursor to cancer, as it is unclear what percentage of DCIS lesions progress to frank cancer, making the treatment of DCIS very confusing to patients. Before the mammographic screening era, which began in earnest after 1980, diagnoses of DCIS were uncommon. Now DCIS makes up nearly a third of new breast cancer diagnoses. Again, because we don’t know which of these lesions will progress and which won’t (or even which ones might regress), we treat them all, and this treatment involves nearly all the treatments used for breast cancer, with the only treatment not used on DCIS being chemotherapy.
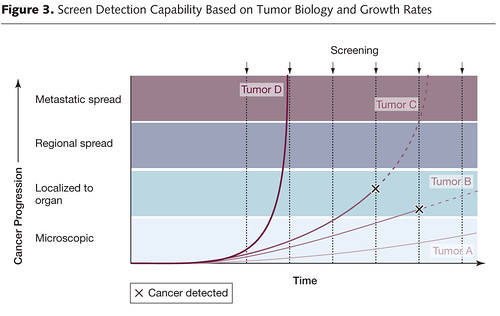
As for more advanced regional tumors (tumors with lymph node metastases or involvement of local structures) and metastatic tumors, the absolute numbers have also decreased, but not very much. If screening were having a huge effect on breast cancer, the expectation would be that removing tumors at a smaller stage would, nearly three decades later, ultimately result in fewer advanced cancers being detected, their having been preempted by screening and appropriate treatment by surgical excision and adjuvant therapy. (This is one reason why screening for colorectal cancer has been more effective; removal of polyps is effective at preventing the subsequent development of colorectal cancer.) The conclusion, which again should be nothing surprising for anyone who saw my post from last year, is that screening by nature preferentially detects slower growing, more indolent cancers, which by their very nature tend to be less lethal and some of which may not even ever progress enough to endanger the life of the patient. The fastest-growing, most lethal cancers grow so fast that they seem to “pop up” between screenings. As a breast cancer surgeon, I see such tumors occasionally. A woman will come in with a palpable mass and an very ugly mammogram after having had a mammogram less than a year before that shows no trace of abnormality or, sometimes, an abnormality that is only appreciated in retrospect because it was so subtle. Naturally, such women are distraught because they have “done everything right” and obtained their yearly mammography just as their primary care doctors told them too. However, no practical screening program could catch tumors such as these because it would require too frequent screenings, which would also, unfortunately, increase the chances of finding abnormalities that lead to overdiagnosis. The dilemma, again, was discussed in my post, and, indeed, Figure 3 in the JAMA article is in essence the same figure that I reproduced to help me discuss length bias, only with much better design sensibilities and a dash of color:
The most distressing conclusion of Esserman’s analysis is just how many patients need to be screened to save one life. It is well-accepted that screening women over age 50 for breast cancer does decrease mortality due to breast cancer by approximately 30%, but what does this reduction really mean? This:
Essentially, mammography reduces the odds of a 60-year-old woman dying of breast cancer in the next decade by 30%. Sounds impressive, until you look at her absolute risk: by getting her annual mammogram, her chances of dying from breast cancer are whittled from 0.9% to 0.6%. Overall, for every 1,000 women in their 60s screened for breast cancer in the next 10 years, mammograms will save the lives of 3 people but 6 others will still die. (The numbers edge up or down in lockstep with a woman’s age.)
Esserman et al conclude that, to avert one death from breast cancer with mammographic screening for women between the ages of 50-70, an age range intentionally chosen because it is the age range for which mammographic screening is the least controversial, 838 women need to be screened over 6 years for a total of 5,866 screening visits, to detect 18 invasive cancers and 6 instances of DCIS. The additional price of this was estimated to be 90 biopsies and 535 recalls for additional imaging, as well as “many cancers treated as if they were life threatening when they are not.” For prostate, to prevent one death from cancer, 1,410 men need to be screened over 9 years, for a total of 2,397 screening visits and 48 cancers detected. In other words, screening takes a lot of effort for, on an absolute basis, not as many lives saved as we had hoped. The authors also point out that technology exacerbates this problem. We push for ever greater sensitivity at the cost of lower specificity, which means that we detect more and more lesions that turn out not to be cancer or to be indolent, non-lifethreatening cancer. Yet all of these cancers end up being treated the same, again because we cannot distinguish between them. The addition of hypersensitive modalities such as MRI only exacerbate this problem even further. As Esserman et al state:
After 2-1/2 decades of screening for breast and prostate cancer,conclusions are troubling: Overall cancer rates are higher, many more patients are being treated, and the absolute incidence of aggressive or later-stage disease has not been significantly decreased. Screening has had some effect, but it comes at significant cost, including overdiagnosis, overtreatment, and complications of therapy, problems likely to be exacerbated as the US population ages. Additional gains are unlikely with the current approach and may inadvertently add to the burden of treatment and diagnosis for relatively indolent disease.
So what’s the solution? Should we give up on screening?
I’ll answer the second question with an emphatic absolutely not. There is no doubt that screening can save lives; the problem is that we’re doing it “bigger” not and not necessarily better or smarter, using more or less a one-size-fits-all approach when a more tailored approach is necessary. In essence, we’re using 20th century technology, when 21st century technology can find a way out of these conundrums. Here’s where I (mostly) agree with Esserman et al. We need to change how we screen for common cancers using the latest advances in biochemistry, molecular biology, and technology to differentiate which lesions are most likely to be cancer and which are not, which cancers are likely to progress to the point of threatening a patient’s life in their remaining lifespan and which ones are not. To this end we need the following tools:
- Develop biological and genetic markers of risk for various cancers. It’s long been known that screening is more effective in populations where a disease is common. The more common the disease (to a point) the more likely screening is to save lives. Thus, if we could develop better tools to identify women most at risk for breast cancer, for example, we could start screening such women at a younger age and perhaps screen them more frequently. We already do this to some extent, but our current tools (family history to identify higher risk populations, a handful of genetic markers, and ethnicity) are crude measures at best. Equally important would be to find similar markers to identify women at lower risk, who might start screening at an older age and undergo screening less frequently. Most important of all, identifying high risk patients more effectively would open up the possibility of prevention to a far greater extent than is possible now.
- Identify biological markers to differentiate minimal risk cancers from cancers with significant risk. Again, we have begun to do this to some extent. For example, tests such as the Oncotype DX multigene test are now clinically used to determine which women with early stage, estrogen receptor-positive breast cancers would and would not benefit from chemotherapy. It’s relatively crude as a tool goes, but we will do better. Indeed, we are beginning to develop the tools that would allow us to go much further. It would not surprise me if, in a decade or so, we routinely do a battery of such tests on newly diagnosed tumors and then use the results to decide which ones can undergo “watchful waiting,” which ones need aggressive therapy, and which ones can undergo less aggressive therapy. Eventually, we will be using therapy targeted to the individual genetic alterations in an individuals tumor. Yes, I know I’ve expressed skepticism over such “targeted” therapy before, but that’s not because I don’t believe the concept will work; it’s because the boosters of targeted therapy often seem not to realize just how difficult and complex it is and will be to identify targets and how hard it will be to turn the targeting of proteins and genetic alterations into therapies that result in decreased mortality from cancer. In other words, I believe that genetic and biomarker analysis will ultimately allow us to tailor therapy to an individual’s tumor; I just think that getting there will take a lot longer and be a lot messier than the current generation of biotech cheerleaders either understand or will let themselves admit.
- Develop better markers of response to therapy. Right now our primary assessment of whether a therapy is working or not boils down to one of two things: survival rates (the ultimate endpoint) or whether a tumor shrinks or not in response to therapy. Both are very crude. The former is the ultimate measure, but it is not helpful in the case of an individual patient, who wants to know if her treatment worked or not before she dies. The latter is notoriously inaccurate, with tumor shrinkage only showing a weak correlation to overall survival. This is one area where tests similar to the ones being developed to determine the aggressiveness of a tumor could potentially help.
- Develop better imaging tools to assess risk. This is the one area that Esserman et al neglected almost completely in their review. This is an area that I have only recently become very interested in for our research program. Technology is progressing to the point where it soon may well be possible to identify a lesion as cancerous or not with greater than 90% using a “virtual biopsy” and then further to determine its risk of causing the death of the patient, when combined with biochemical and genetic analyses. Such tools would allow us to choose patients who might be appropriate for “watchful waiting” with far less anxiety over whether we’re doing the right thing than there is now and, even better, potentially to identify tumors that are likely to regress spontaneously.
None of this will be easy, and the process of getting from where we are now to this futuristic vision will be be full of fits and starts. At times it will be controversial. Advances in science-based medicine always are. Moreover, there will be significant barriers to its implementation, not the least of which is the relatively simplistic thinking that has come to predominate how we view cancer screening, not in the rarified air of the research institutions that actually study the pros and cons of screening, but “in the field” at the level of individual practitioners trying to put these screening recommendations into practice. It is not the fault of these practitioners that these fine points are not more widely known. Rather, the reason derives from the conflict between the need for simple messages to tell patients and the difficulty of applying epidemiological science to individual patients.
So what do we do in the meantime? One thing I am not going to say is to stop undergoing screening. Women should continue to undergo mammographic screening as recommended according to the standard of care. Whether men should continue to undergo routine prostate screening as previously recommended is now controversial, with less evidence to support it than mammography except in high risk populations. Until a consensus develops for changing the current regimen, it is the best we have, and, for all its shortcomings, mammography remains the best and most cost-effective tool we have to detect cancer. (The case for routine mass PSA screening, in contrast, now strikes me as considerably weaker.) Even in the worst case scenario that breast cancer screening results in the appearance of a benefit all due to lead time bias (which it isn’t; I present this as a worst case scenario), treatment of cancers caught at an earlier stage is still less invasive and less morbid. True, this has to be weighed against overtreatment of lesions that would never progress, but even so the benefit of using less invasive therapy is one that is routinely discounted by the new generation of what I am sometimes tempted to call “screening nihilists,” a group that seems to think that nearly all screening is worthless.
The problem is not that screening is worthless. For example, even mammography under the most pessimistic estimates routinely touted as evidence that it’s pointless to screen clearly does save lives. A relative reduction in risk is not meaningless or of insignificant worth, either, as some nihilists will suggest. Also, don’t forget that even small absolute percentages when applied to millions upon millions of people, can result in large numbers of lives saved. That being said, I also think that these recent trials suggest that we are not doing an adequate job of informing patients of the down side of screening, such as excessive biopsies, a down side many might well be willing to accept if they were informed of it and understood it. After all, as I’ve mentioned before with regards to breast cancer, I’ve seen polls where most women say they would agree to undergo cytotoxic chemotherapy to improve their odds of surviving breast cancer by 1%. To save more lives relative to the number of women overtreated and overdiagnosed, we need to learn how to screen smarter. Our current screening regimens are not good enough. Improving them will require science-based medicine, and, unfortunately, will be controversial. Watching the jolting, jarring journey to a new scientific consensus about something as important as screening for breast and prostate cancer is much watching the proverbial sausage being made. I also can’t help but point out the contrast to “alternative” medicine, which rarely questions and almost never changes practice in the face of new data. It may well be that our hopes for screening for breast cancer and prostate cancer were too high, but in science-based medicine evidence eventually wins out. Screening practices will likely change in the face of new evidence, and that is a good thing. Certainly it’s better than the alternative, namely not changing and not improving.