It’s that time of year when every day I can expect to see at least one patient with a concern about Lyme disease. In Lyme-endemic regions such as Western Massachusetts, where I practice pediatrics, summer brings a steady stream of children to my office with either the classic Lyme rash (erythema chronicum migrans, or ECM), an embedded tick, a history of a tick bite, or non-specific signs or symptoms that may or may not be due to Lyme disease. Sometimes the diagnosis is relatively straightforward. A child is brought in after a parent has pulled off an engorged deer tick, and there is a classic, enlarging ECM rash at the site of the bite. More often the presentation is less clear, requiring detective work and science-based reasoning to make an informed decision and a diagnostic and therapeutic plan based on the best available evidence. Depending on the story, the plan may include immediate treatment without any testing (as in the straightforward case described above), immediate testing without treatment pending test results, or waiting as we watch and see how a rash progresses before doing anything. An example of this latter course of action would be when a patient comes in with a pink swelling at the site of a new tick bite. In this case, it may not be clear if the swelling is a Lyme rash or simply a local reaction to the bite, a much more common occurrence. The classic ECM rash (an enlarging, red, circular, bull’s-eye rash at or near a tick bite) typically develops 1-2 weeks after a tick bite, but can occur anywhere from 3-30 days later. It then expands and darkens over another 1-3 weeks before fading. This classic rash is not the most common rash of Lyme disease, however, as it occurs in only about 30% of cases. Instead, the rash may be uniformly pink or red (or even darker in the center) without the target-like appearance, or may be a linear rash, expanding outward from the tick bite site. In the case of a patient who comes in with a vague, pink swelling within a day few days of a tick bite, we will typically wait and see what happens to the rash. If it is a local reaction, it will likely resolve within another few days. With Lyme disease, the rash will continue to enlarge and declare itself as an ECM rash. Another unclear and not uncommon situation is when a patient comes in with non-specific symptoms such as fatigue, musculoskeletal pains, and headache. If warranted by the history and the physical exam, we may in this case order Lyme testing. This may not give us an answer even if the patient has Lyme disease, because results are often negative in the first few weeks of the disease. In this case, if symptoms persist or evolve, we will repeat the testing in another few weeks at which point true Lyme disease will test positive and can then be treated. The good news is that the treatment of Lyme disease, particularly in the early, localized phase of the disease, is extremely safe and effective with a 14-day course of antibiotics. The testing is also relatively straightforward, with very good sensitivity and specificity when performed correctly. And this is where the bad news comes…
Lyme-literate doctors
Though providers who choose to practice a science-based approach to caring for their patients stick to the CDC-recommended testing protocol, created using the best evidence, there are many so-called “Lyme literate” providers who stray from the evidence-based path to offer up a potpourri of unapproved, non-recommended, and expensive tests to their patients. The purpose of these tests is without a doubt to detect cases of Lyme disease that other, presumably Lyme-illiterate providers missed due to their “close-mindedness” to these superior tests. Before we discuss these maverick, enlightened providers further, let’s review the tests that are currently recommended by the CDC and the best available evidence.
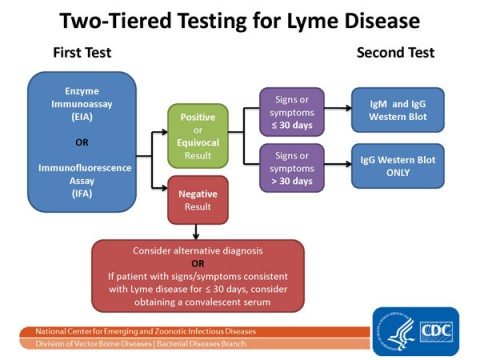
The CDC has set forth a relatively simple protocol for the use of laboratory testing to confirm a suspected case of Lyme disease. The current, science-based consensus on laboratory diagnostic testing for Lyme disease comes from the Second National Conference on Serologic Diagnosis of Lyme Disease, which convened in 1994. Based on the best available evidence, the Conference recommended a two-step testing protocol using a single blood sample.
Step I: ELISA
In step I, an enzyme-linked immunosorbent assay (ELISA) is used to detect antibodies to a wide assortment of antigens from B. burgdorfori, the Lyme organism. If this test is negative, it is likely that either the patient does not have Lyme disease, or that the test was performed too early in the course of the illness (the first 3-4 weeks). In this case, the test should be repeated in a few weeks, assuming the diagnosis is still being considered due to persistent signs or symptoms. If, on the other hand, the result of step I is positive or equivocal, a more definitive and specific test is performed.
Step II: Western Blot
If Step I is positive or equivocal, we move to step II, the Western blot (WB) test. This looks for antibodies to specific Lyme proteins that have been separated based on their molecular weights. These separated proteins are then exposed to the patient’s blood sample. If the patient has antibodies to these proteins, they bind to them and are visible as bands on the WB. A specific pattern of positive bands of sufficient intensity are required to be present for the WB to be interpreted as positive.
When performed correctly, this test is considered highly specific for Lyme disease. When well-trained individuals at certified labs perform the correct FDA-approved tests in appropriate circumstances, and when providers interpret the results correctly, Lyme disease testing can be a reliable way to confirm or rule out the disease with a high degree of validity. Unfortunately, this does not always occur.
Confirmation bias and the Lyme-literati
Individuals who believe they have Lyme disease that was missed by their own providers will sometimes seek out so-called “Lyme-literate” providers; I’ll call them Lymlits. Often these individuals believe they are suffering from chronic Lyme disease (a non-entity discussed elsewhere), and are hoping to confirm this diagnosis. Lymlits provide the confirmation bias these patients are looking for. They quickly empathize with these patients and offer what they claim to be a more informed approach to their diagnosis and treatment. Like all alternative medicine providers (and make no mistake, that is exactly what we are talking about here), they are quick to cast the patient’s more conventional provider as shackled by convention, or to Big Government or Big Pharma. Often they claim a more holistic approach as well, infusing other sCAM modalities or spiritualism into the mix. Again, like many sCAM providers, they claim special knowledge and insights not available to or ignored by conventional providers. To the sCAM-credulous, the Lymlits represent an open, understanding ear and long-sought answers to their problems.
The websites of Lymlit providers clearly pander to the fears, anxieties, and preconceptions of their clients. Often they contain entire sections devoted to the “problem” of undiagnosed (but not over-diagnosed) Lyme disease, and how the Lymlits can help uncover the diagnosis and provide the correct (often dangerously incorrect) treatment. The patients I see at my practice who have bought into a wide variety of woo diagnoses and treatments have often been seen by providers of the Northampton Wellness Center, and the over-diagnosis and treatment of Lyme disease is no exception. Their services are so typical of this this kind of practice that I will use them as an example. A quick perusal of their website’s Lyme disease section should be of concern to anyone who cares about the practice of EBM and SBM. Like many sCAM practitioners, this group does not serve as primary care providers but rather as “consultants”. This is a misnomer, however, as they are rarely consulted by science-based providers. Rather, patients typically self-refer. Using a “holistic” approach, they claim the ability to help patients with chronic illness who have not been helped by their conventional providers. What they offer is reassurance that they have come to the right place, that they will get the answers they are looking for, and receive treatments not available through most providers. Ironically, their diagnostic tests and treatment modalities are usually described with terms borrowed from true science, and are often claimed to be evidence-based as well. The Northampton Wellness Center’s website seems to do everything possible to reaffirm people’s fears about their chronic or undiagnosed Lyme disease. It explains why the organism is so tricky to diagnose and treat (it really isn’t), and how they can do so safely, effectively, and often “naturally” and “holistically”. They hype the existence and importance of biofilms, co-infections, weakened immune systems, and heavy metals in the pathogenesis of Lyme disease, and explain how they can help diagnose and fix these problems. And unsurprisingly, the Northampton Wellness Center website has the clear red-flag seen on many other sCAM practice websites – the ubiquitous web store. These stores typically hawk all manner of supplements, potions, and snake oils to treat your every ailment. I couldn’t access the Northampton Wellness Center’s web store without being a patient, so I don’t know exactly what they offer the chronic Lyme sufferer. Perhaps most alarmingly, Lymlits like those at the Northampton Wellness Center hype unapproved and non-recommended laboratory tests for diagnosing Lyme disease in their patients. One example is an extended, purportedly-superior Western blot assay. According to their website:
Unfortunately, most laboratories leave out the most specific bands, 31 and 34, on their Western Blot assays. If we use a special laboratory and get a positive band 31 result, we can confirm that this is truly related to the Lyme organism by doing a “31 kDa epitope” test, to make sure it is not positive from a cross-reaction, which could occur from having a chronic viral infection.
Without getting too deep into the weeds here, the Internet is rife with conspiracy theories about why the CDC would fail to include the 31 kDa band in the group of bands required to be present for a positive Western blot interpretation. At the heart of the conspiracy is the belief that this band, which represents OspA, the outer surface protein of B. burgdorferi, was left out because OspA was the main component of a Lyme vaccine (Lymrix) which is no longer available but was given to nearly 2 million people before it was taken off the market. The allegation is that the band was not included because people who had received Lymerix would likely test falsely positive. Given the limited number of individuals vaccinated with Lymerix, this seems an unlikely explanation. Another allegation is that the CDC and FDA do not want people to be diagnosed with Lyme disease as a result of a conspiracy involving the insurance industry. However, as explained by Halperin et al. in the book Lyme disease: an evidence-based approach, the explanation is much more mundane (and rational) than this:
the bands selected for use in the Western blot were chosen not because they are unique to B. burgdorferi but rather on the basis of statistical considerations that included an analysis of those combinations of bands that provided the best predictive values for well-characterized specimens known to have been obtained from individuals with and without Lyme disease
In other words, though OspA is a relatively specific marker for infection with B. burgdorfori, in the assessment of actual patients it was not found to be among the group of bands which best distinguished Lyme disease patients from controls.
They go on to add that that:
laboratories using criteria other than these must establish the validity of their own criteria based on equally rigorous scientific assessments.
Scientists are actively working on better, more sensitive and specific diagnostic tests for Lyme disease. But it will take reproducible and validated results to move these tests forward. Not the direct marketing of unsupported tests to Lymlits by specialty labs. Other examples of unapproved and non-recommended tests discussed on the Northampton Wellness Center website and recommended by many Lymlits include dot-blot testing, PCR, and T-lymphocyte response assays. The CDC clearly states that none of these tests are sufficiently reliable for diagnosing Lyme disease. In 2005, the CDC became so concerned about the proliferation of non-validated and potentially dangerous tests for Lyme disease, that it issued an alert in its Morbidity and Mortality Weekly Report (MMWR). In April of this year, the CDC issued yet another warning about a new laboratory-developed culture method that has been made available commercially. Again, the CDC has warned that the results of these types of “home-brewed” tests should not be relied upon. According to the warning:
Published methods and results for this laboratory-developed test have been reviewed by CDC. The review raised serious concerns about false-positive results caused by laboratory contamination and the potential for misdiagnosis.
The CDC’s warnings are justified. While Lymlits claim these specialized tests are better able to detect Lyme disease than those used by conventional practices, what they do, in fact, is produce a predictable increase in false-positive results. Thus, by pretending to have superior testing options than those provided by the patient’s primary care provider, Lymlits provide patients with the elusive Lyme disease diagnosis they are searching for, and then offer unnecessary treatments for a non-existent infection. Ignoring the science-based treatment recommendations of the Infectious Disease Society of America (IDSA), Lymlits often recommend dangerously long, sometimes intravenous courses of antibiotics, in addition to myriad other potentially dangerous sCAM modalities for the treatment of these questionable infections. Additionally, the misdiagnosis of Lyme disease in these individuals potentially delays the diagnosis of other, real conditions, which then go untreated.
Ironically, Lyme advocates and Lyme-conspiracy proponents were at the forefront of the manufactroversy surrounding the demise of Lymerix, the first FDA-approved Lyme vaccine. Although Lymerix, whose main component was the OspA protein, was not the most effective vaccine (with an efficacy rate <80%), it was still a cost-effective preventative strategy for people at risk in endemic areas. Unfortunately a slew of adverse events reported soon after the vaccine was licensed, combined with an irresponsible (but predictable) media storm, put a chill on the use of the vaccine, eventually leading to its economic failure and being pulled from the market. Pre- and post-marketing studies involving large numbers of patients failed to link any significant adverse events to Lymerix beyond the usual injection site redness and swelling and occasionally fever seen with other vaccines. There was some evidence that a small subset of people with the HLA-DRB1*0401 genotype might be at risk for developing an autoimmune reactive arthritis in response to the vaccine, though the data was inconclusive and did not prove causality. Still these concerns, combined with the spreading fear of unsupported adverse events and the ensuing media frenzy was enough to put an end to the vaccine, a vaccine that could have led to the prevention of many cases of Lyme disease.
Conclusion: Lymlit tests are not supported by good evidence
Lymlit doctors claim they are providing their patients with a service that most others are either unwilling or lacking the knowledge to provide. They balk at the argument that these tests are not supported by sufficient evidence of validity, citing junk science, data from the proprietary labs themselves, or anecdote to support their position. These arguments are often shrouded in conspiracy theory, invoking closed-door sessions in which physicians and scientists do the bidding of Big Pharma or the insurance industry. So-called Lyme advocacy organizations have evolved to support individuals who believe they have chronic Lyme disease or Lyme disease undiagnosed by their doctors. While research is underway to develop even more sensitive and specific tests for diagnosing Lyme disease, the current strategy recommended by the CDC is the best we have to date. Unfortunately, as long as there are providers willing to pander to conspiracy theorists and to patients looking to confirm their fears, people will continue to be needlessly treated, and our societal approach to science will move further back in time.