About a month ago, I finally wrote the post I had been promising to write for months before about medical marijuana. At the time, I also promised that there would be follow-up posts. Like Dug the Dog seeing a squirrel, I kept running into other topics that kept me from revisiting the topic. However, over the past couple of weeks, the New York Times gave me just the little nudge I needed to come back and revisit the topic, first by openly advocating the legalization of marijuana, then by vastly overstating the potential medical benefits of pot (compare the NYT coverage with my post from a month ago), and finally this weekend by running a story lamenting the federal law that makes research into medical marijuana difficult in this country.
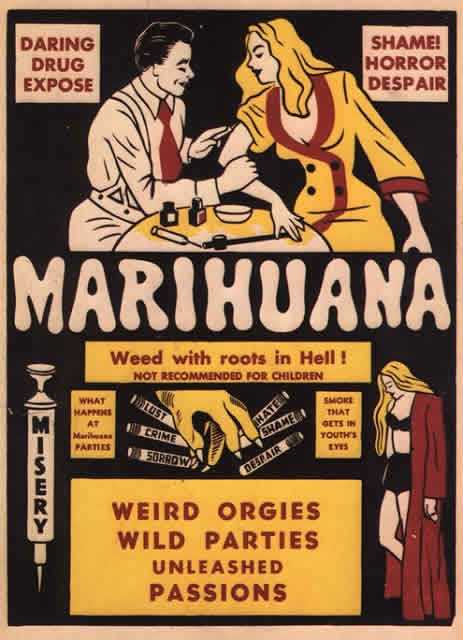
I stated my position on marijuana last time, which is that marijuana should be at least decriminalized or, preferably, legalized, taxed, and regulated, just like tobacco and alcohol. I also likened the cult of medical marijuana to the “new herbalism,” because it (1) vastly inflates the potential of medicinal uses of marijuana and (2) ascribes near-mystical powers to smoking or making extracts out of marijuana, rather than identifying and isolating constituents of the plant that might have medicinal value. All of this is very much like herbalism in alternative medicine. Indeed, promoting laws legalizing medicinal marijuana is such an obvious ploy to open the door to full legalization that some advocates don’t even bother to disingenuously deny it any more. Given that I tend to support legalization, as a physician this sort of deception irritates me. It also has consequences, particularly when overblown claims are made for what cannabis can do. Perhaps the best example of this is the claim that cannabis cures cancer, which pops up all over the Internet in memes such as the one in the image above.
Don’t believe me? Just Google “cannabis cures cancer” or “marijuana cures cancer.” To my relief, you’ll find the National Cancer Institute’s page on cannabis and cannabinoids, which, as I discussed last time, dwells more on whether cannabinoids are useful for pain relief, nausea, and cancer cachexia than on whether they can be used to treat cancer directly. However, you’ll also find pages like 20 Medical Studies That Prove Cannabis Can Cure Cancer, a Facebook page Cannabis Cures Cancers!, and articles like Rick Simpson’s Hemp Oil Medicine, which resembles a lot of articles for various alternative medicine and quackery in terms of providing lots of testimonials of cures for skin cancer, diabetic ulcers, and other skin diseases and conspiracy mongering but no hard evidence. Indeed, a commenter by the ‘nym of “Danman” showed up at another blog many of you are familiar with and proceeded to make hilariously bad arguments for the healing power of cannabis and how a post at that blog was a “prohibitionist hit piece,” even though it expressed the opinion that marijuana should be legalized over the course of over 150 comments. Meanwhile, others are recommending hash oil for gliomas with a near-religious fervor, touting the same sort of evidence that Stanislaw Burzynski uses to claim he can cure gliomas with antineoplastons.
So what is the story, really?
Cannabinoids versus cancer: Hype versus science
The first problem one encounters when examining the evidence concerning the effect of cannabinoids on cancer is that the vast majority of studies touted by advocates claiming that “cannabis cures cancer” are either in vitro or animal studies. In vitro and animal studies are what we in the biz call “preclinical data,” meaning data obtained before trying a treatment in the clinic. As the American Cancer Society put it:
More recently, scientists reported that THC and other cannabinoids such as CBD (cannabidiol) slow growth and/or cause death in certain types of cancer cells growing in laboratory dishes. Some animal studies also suggest certain cannabinoids may slow growth and reduce spread of some forms of cancer. However, these substances have not been tested in humans to find out if they can lower cancer risk. There is no available scientific evidence from controlled studies in humans that cannabinoids can cure or treat cancer.
This basically says it all, and it’s tempting to wind up this post right there, but, as Han Solo said after being urged to be quiet while taking out some storm troopers, “Hey, it’s me.” Besides, you, our SBM readers, expect science in addition to my self-absorbed blather, as amusing as it might sometimes be. So you shall have it. As good a place as any to start is, as you might imagine, 20 Medical Studies That Prove Cannabis Can Cure Cancer. After all, I assume that Arjun Walia, the person who put this list together, wanted to provide the very best evidence that could be found, particularly given the emphasis that “this is a short list.” I perused the papers in the list and was—shall we say?—underwhelmed. I’ll divide my discussion into tumor types, the way the list does. First, you have to understand that CBD, one of the cannabinoids found in marijuana, is viewed as particularly promising because it does not produce the same psychotropic effects as Δ9-tetrahydrocannabinol (THC), making it a particularly attractive for developing treatments whose side effects don’t involve being stoned all the time.
Glioma. The first thing that jumped out at me is that one of these papers has nothing to do with cancer, specifically this study that suggested that cannabinoids could protect the brain against neurodegeneration in neonatal rats caused by the toxin ouabain (an Na+/K+-ATPase inhibitor). The vast majority of the other studies were in human cell lines, such as this one studying the effect of cannabidiol, a nonpsychoactive cannabinoid, on glioma cell lines. As a cancer researcher, I noted that the IC50 (the concentration that produces 50% of maximal inhibition of the parameter being measured), was 25 μM, which is a bit higher than we like for an anticancer compound. I was thus not particularly impressed, although in fairness subcutaneous injection of CBD was able to inhibit the growth of glioma xenografts implanted subcutaneously in athymic nude mice, although no dose-response was demonstrated, and a dose of 0.5 mg per mouse is a pretty generous dose (25 mg/kg for a typical 20 g mouse). So while there does appear to be antitumor effect against the glioma cell lines tested, it was, at best, modest. Certainly it wasn’t the sort that would knock my socks off as a cancer researcher. A different study, which combined THC and temozolomide, produced more impressive results, not for the THC, which produced at best modest antitumor effect, but for the combination, which looked a bit more promising. Of course, one also must note that this is not hash oil or smoked pot, but the purified THC component. That THC might be useful against glioma does not tell us that hemp oil or smoking the weed will be useful against glioma any more than the fact that digoxin works in congestive heart failure tells us that it would be a good idea to ingest foxglove leaves.
Skeptical Raptor puts it in perspective:
In one study, the researchers determined that it would take a concentration of cannabinoids of approximately 10 µmol/L to cause the death breast cancer cells in cell culture. This converts to around 3.14mg/L of THC. So, you’d have to assume that to kill any breast cancer cells, you’d need at least a blood level of 3.14 mg/L to achieve breast cancer cell death. So how close to that 3.14 mg/L can we get by just smoking a joint or two? According to research, smoking one joint will give you a blood level of THC of around 1.3-6.4 ng/mL serum, or about .00013-.00064 mg/L. In other words, to get an anti-cancer effect, you need to light up around 1000 joints per day.
The IC50 values in these studies were higher than 10 μM.
Finally, there was one human study in the list of glioma papers. Basically, this was a phase I trial testing a method of administering THC. This was also some strange science in that nine patients with recurrent glioma had their tumors resected, but a catheter was left in the cavity left behind after surgery, and then:
Each day an aliquot of the THC solution (100 mg ml−1 in ethanol) was dissolved in 30 ml of physiological saline solution supplemented with 0.5% (w v−1) human serum albumin, and the resulting solution was filtered and transferred to an opaque syringe. This process was performed at the Department of Pharmacy of the Hospital Universitario de Canarias. Owing to the high hydrophobicity of THC, we controlled by gas chromatography/mass spectrometry (see below) the actual concentration of THC in the final solution. The THC solution was administered to the patients for different times starting at days 3–6 after surgery at a rate of 0.3 ml min−1 with a syringe pump connected to the subcutaneous reservoir. In the case of Patients 1 and 2, who received THC for 30 and 26 days, respectively, biopsies were also taken after the THC-treatment period and various tumour-cell parameters were evaluated.
As you can see, this is very different from smoking marijuana or ingesting hash oil. It involves directly infusing THC solution at a high concentration directly into the brain cavity where the tumor had been, in the hope of killing off any remaining tumor cells surrounding the cavity. Let’s just put it this way. There’s a reason why direct intratumoral injection of any drug is generally frowned upon, and that’s because it’s invasive and rarely works. Moreover, no one generally bothers with intratumoral infusion of a drug unless it requires a very high concentration to work. Mean survival was 24 weeks, and two patients survived approximately a year. The authors try (rather like Stanislaw Burzynski, actually) to argue that this is better than would be expected based on other studies and controls, and to claim that some patients responded. I find no convincing evidence of this in the paper, and in a cohort of nine patients though, it’s pretty darned hard to conclude this. I agree with Harriet. There is nothing “earth shattering” about these results. They could be consistent with an antitumor effect, but they could just as easily be consistent with no effect. Worse, this was not simply ingesting, smoking, or being injected with cannabinoids. The study involved having catheters sticking out of the subjects’s heads and having THC infused directly into the brain.
Breast cancer. I’m a breast cancer surgeon; so I’m going to go out of order here. There are four breast cancer studies listed. The first study examines CBD activity against a mouse breast cancer cell line 4T1 (another cell line I’m quite familiar with, having used it in my lab and because it was a cell line developed by a now retired investigator whom I know), and the breast cancer cell line MDA-MB-231 (which I’m more familiar with than I’d like to be). Basically, the study showed a modest effect against these two cell lines in vitro and in mouse models using 1 mg/kg and 5 mg/kg CBD. The second study looked at five different cannabinoids and found that CBD was the most potent inhibitor of breast cancer cell growth in vitro (IC50 between 6.0 and 10.5 μM) and that CBD and “CBD-rich oil” could inhibit the growth of MDA-MB-231 tumor xenografts. In this study, the effects of THC on cancer cell growth were weak (IC50 between 14.2 and over 25 μM, depending on the cell line). The third study showed similar results for HER2/neu(+) tumor cell lines using THC and specific synthetic agonists (activators) of cannabinoid receptors CB1 and CB2 (Win55,212-2 and JWH-015, which activate CB1 and CB, respectively) except that THC was not as weak. The fourth study didn’t look at marijuana cannabinoids at all, but rather the endogenous cannabinoid anandamine, with similar results.
Lung cancer. The next set of three studies look at lung cancer. The first study used a cell line with which I’m quite familiar, A549 lung cancer cells, using both cell culture and mouse xenograft models. I must say that I was singularly unimpressed with the effect sizes, at least in the in vitro studies, which also required fairly high concentrations (15 μM) of THC. In a mouse tail vein injection model of lung metastases, 5 mg/kg of THC decreased metastases by 50%, which is not bad, and in a straightforward xenograft model resulted in a 50% growth delay of the tumors, which is also not bad. The next study found similar results testing CBD against lung cancer cell lines and tumor cells from a patient in cell culture and mouse models. The third study showed that stimulation of cannabinoid receptors (CB1 and CB2) with synthetic agonists, Win55,212-2 and JWH-015, which activate CB1 and CB2, respectively, inhibited the growth and invasion of A549 lung cancer cells in vitro and their growth and metastases in mouse models.
And so it goes. Nearly all of these studies look at purified cannabinoids, usually either THC or CBD, but sometimes the endogenous cannabinoid anandamine (which isn’t even in marijuana), as with the breast cancer study above and this prostate cancer study. Some use synthetic agonists, such as the breast cancer and lung cancer studies above, or this study of mantle cell lymphoma that tested R(+)-methanandamide in addition to Win55,212-2, or this study of non-Hodgkin’s lymphoma, which also used R(+)-methanandamide. With the exception of the glioma study, all were preclinical studies looking at cell culture models and mouse models. One was a review article. One, as I pointed out above, had nothing to do with cancer, and I suspect the author included it to round up his list of studies to 20.
Unfortunately, it’s a highly intellectually dishonest list of studies if your goal is to provide evidence that “cannabis” (as in the plant or extracts from the plant) can cure cancer. Unfortunately, this is not the first time Arjun Walia has constructed such a list. Last year, Liz Ditz nailed him for constructing a similarly intellectually dishonest list of studies that “show vaccines cause autism.” Let’s just put it this way. In 2013, Walia was still citing some highly discredited studies, such as studies by Mark and David Geier.
The intellectual dishonest of representing this list of studies as evidence that cannabis cures cancer aside, it is a group of moderately interesting papers that suggest that purified cannabinoid receptor agonists can produce reasonable, albeit by no means spectacular, antitumor effects in preclinical models. As a whole, they suggest that some of these purified cannabinoid agonists, whether naturally occurring, such as THC, CBD, or synthetic, such as R(+)-methanandamide, or specific to CB1 or CB2, such as Win55,212-2 and JWH-015, might be worth investigating further. Again, we’re talking about pharmacology, isolating active substances and purifying or chemically modifying them to improve their activity and safety profile, not smoking weed or using hash oil. Cancer Research UK concludes:
But claims that this body of preclinical research is solid “proof” that cannabis or cannabinoids can cure cancer is highly misleading to patients and their families, and builds a false picture of the state of progress in this area.
It’s also noted that the best results in the lab have come from using a combination of highly purified THC and CBD, but that there have also been positive results with synthetic cannabinoids, such as a molecule called JWH-133, just as I’ve described, through mechanisms that include:
- Triggering cell death, through a mechanism called apoptosis
- Stopping cells from dividing
- Preventing new blood vessels from growing into tumors
- Reducing the chances of cancer cells spreading through the body, by stopping cells from moving or invading neighbouring tissue
- Speeding up the cell’s internal ‘waste disposal machine’ – a process known as autophagy – which can lead to cell death
Unfortunately, as good as that sounds, it’s not all good. There is also evidence that cannabinoids, under some circumstances, can stimulate cancer cell growth and possibly contribute to tumor progression. They can also have different effects depending on dose and the level of cannabinoid receptors on the tumor cells being treated. For instance, this study suggests that cannabinoids only induce apoptosis in cells that express low levels of receptors that couple to a signaling pathway called ERK1/2 but don’t induce apoptosis in cells that have high levels of receptors because they then couple through a survival pathway known as AKT. Interestingly, cannabinoids also seem able to induce cell death through pathways that don’t involve cannabinoid receptors. In other words, it’s complicated, because cancer is complicated, and cancer drugs tend to work only against certain cancers. If cannabinoids do have anticancer effects in humans, it will likely only be against certain cancers, most likely combined with existing chemotherapy and targeted drugs. We also know from the preclinical work that has been done that it will take purified THC and/or CBD and/or synthetic cannabinoid receptor agonists to produce even the modest effects observed thus far, effects that are too modest to expect cannabinoids to be any sort of cure for cancer on their own. Smoking weed or using hash oil just isn’t going to cut it.
But what about the anecdotes?
On that other blog that you all hopefully know and love, one of the commenters, Justin Kander, cited a case report that’s been going around social media as “proof” that cannabis cures cancer. This case report describes a 14-year-old girl, PK, who presented with symptoms of “weakness, shortness of breath and bruising when she was taken to the Hospital for Sick Children, Toronto, Canada, on the 10th March 2006.” She was diagnosed with acute lymphoblastic leukemia (ALL) and underwent standard chemotherapy for ALL for six months. Upon analysis, she was found to be positive for a mutation in the Philadelphia chromosome, which is found in 2-10% of pediatric ALL cases. Philadelphia chromosome-positive ALL tends to have a poorer prognosis than other ALL. PK underwent a bone marrow transplant but was noted to have blast cells six months after treatment and therefore underwent aggressive chemotherapy along with a tyrosine kinase inhibitor. After more recurrences and more treatment (such as radiation therapy to the brain for a presumed, but never completely documented, infiltration of the brain by leukemia, it was stated in the case report:
On the 4th February 2009, blood was noted in the patient’s stools and a blood cell count revealed the presence of blast cells. As a result, all treatment including the disatinib was suspended and the patient’s medical staff acknowledged failure in treating her cancer. It was charted by the patient’s hematologist/oncologist that the patient ‘suffers from terminal malignant disease. She has been treated to the limits of available therapy… no further active intervention will be undertaken’. She was placed in palliative home care and told to prepare for her disease to overwhelm her body and from which she would suffer a stroke within the next 2 months.
The family found articles on how cannabis supposedly cures cancer, and found their way to Rick Simpson, who has been featured in utterly credulous articles in High Times and SF Weekly (the latter of whose editors really should have known better) as the man who can cure cancer with hemp oil, who provided her with hemp oil mixed with honey (because of the bitter taste and viscous nature of hemp oil). This was administered in daily doses. It is claimed in this case report that there was a strong correlation between increasing dose of the hemp oil and decreases in PK’s blast count (a measure of leukemia cells in the blood), but looking at Figures 1, 2, 3, and 4, I have a hard time seeing it. Figure 1 shows increasing doses of hemp oil from what was called the “chronic” strain. That’s the closest we see to decreasing blast counts correlating with hemp oil dose. By day 15, the chronic strain was gone, and PK started taking Hemp Oil #2 from an outside source. In actuality in Figure 2, we see the blast count increasing with increasing dose until day 27, when it starts falling. Figure #3 shows Hemp Oil #3 (Afghan/Thai strain) from days 44 to 49. Given that the blast count stayed the same one can’t say much about this. Then Hemp Oil #4 was tried from day 50 to day 67, and her blast counts started rising. Finally, Hemp Oil #5 was tried and PK’s blast count fell between days 69 and 78. During that time, PK suffered the psychotropic effects of the hemp oil, including euphoria, disoriented memory, and the like.
Unfortunately, PK developed gastrointestinal bleeding and bowel perforation with peritonitis on day 78 and passed away. So, basically, she lived two and a half months after being placed on hospice. The authors assert that a dose-response curve was achieved, but to my eye I really don’t see it, except perhaps at the beginning, nor do I really buy the claim that the bumps in blast counts correlate with using “lower potency” strains. They also assert because PK was treated for tumor lysis syndrome (a syndrome in which the waste products of tumor breakdown, often seen after intense chemotherapy in hematopoietic malignancies, injure organs such as the kidneys), it must mean that the hemp oil was effective.
Unfortunately, even if a mild dose-response effect was observed that would not rule out spontaneous remission. Spontaneous remission is known to occur in ALL, although it is usually temporary, and spontaneous tumor lysis syndrome has been reported, although it is rare. In any case, one has to wonder whether the patient’s bone marrow was petering out near the end, something that is hard to determine because almost no laboratory values other than blast counts are presented, except at the end, when she had a very low platelet count (8K; normal 150K to 450K), a low white blood cell count (1.4, normal 4.5-13.0), and severe anemia (hemoglobin 8.2; normal: 13 to 16). It wasn’t established how the diagnosis of tumor lysis syndrome was made other than that the patient had elevated urate levels. Indeed, the entire case report seemed to have been written with the belief that it was the hemp oil that accounted for the decrease in blasts. A lot of information has been left out about the patient’s clinical course. All we know is that, after being placed in hospice, she was fortunate to have her blast count fall, developed a central line infection, and was treated for tumor lysis syndrome. We can also infer that she was still having considerable issues with her gut because she was on total parenteral nutrition (being fed by vein) and had trouble when they started to try to feed her orally again.
It should also be remembered that, whether or not hemp oil was responsible for the decline in blasts (which is possible but not convincingly demonstrated by this case study) or whether it was “burnout” of the bone marrow in the terminal phase of the disease or even spontaneous remission, the patient still died. She still developed GI bleeding and a GI perforation with peritonitis and died of it only 78 days after going on hospice. There’s no way of knowing whether hemp oil prolonged her life. Probably it did not, as a two to three month survival after going into hospice after being declared terminal for leukemia is well within what is expected. In other words, this case report is mighty thin gruel indeed.
Of course, the sad story of PK and the treatment of her terminal relapsed ALL with hemp oil is probably the highest quality cancer cure testimonial out there, and unfortunately its quality is not that high at all. The rest of the anecdotes I ran into tended to be about as convincing to someone familiar with cancer as nearly all the other alternative cancer cure testimonials I’ve found; i.e., not very. If you don’t believe me, take a look at this article, in which Rick Simpson claims his success rate for patients with terminal cancer is around 70% and says:
“The ones that can’t be saved are usually the ones who’ve had the most chemotherapy and radiation, or wait too long to start the treatment,” he says. “They have to be able to stay alive long enough for the oil to start to work.” In fact, most patients who undergo chemotherapy die from the treatment, not the disease.
No, it is not a “fact” that most patients who undergo chemotherapy die from the treatment, not the disease. It’s a lie. In any case, Rick Simpson is just like cancer quacks the world over, who have no firm evidence to back up their miraculous-sounding cure rates and excuse their failures by claiming that the treatment patients had before prevented the quackery from working. Quacks like Rick Simpson do those who think that cannabinoids have promise in treating cancer no favors.
Conclusions
There’s a lot of interesting research about the role of cannabinoid receptors in cancer and whether targeting them with cannabinoid agonists from marijuana or other natural sources, synthetic agonists, or endocannibinoids will be a useful tool to add to the armamentarium of anticancer therapies. From what we know now, it is quite clear that cannabis does not cure cancer, at least not by itself and certainly not ingested or smoked as marijuana or ingested or applied topically as hemp oil. Even in purified form, naturally-derived or synthetic cannabinoid agonists show relatively modest antitumor activity in preclinical models, which means that they will have to be combined with existing chemotherapeutic regimens. If they do find their way into the routine clinical treatment of cancer, it will be through rigorous pharmacological studies and rigorous clinical trials, the latter of which, in particular, are painfully lacking. Indeed, if you search ClinicalTrials.gov, you’ll quickly find lots of trials of cannabinoids to treat cancer-related symptoms and side effects, but precious few to treat cancer itself. There’s this phase I trial of Dexanabinol in Patients With Advanced Solid Tumors, which has been open two years and is still accruing patients, as well as this one of Dexanabinol against brain cancers. It’s not a lot, and suggests that there is not much interest in even synthetic cannabinoids as a treatment for cancer. After all, there are so many other promising avenues that a class of drugs that show the modest effects that the cannabinoids I’ve discussed do just don’t excite researchers that much.
In any event, the claims of advocates that “cannabis cures cancer” are nothing more than herbalism infused with the magical thinking of the naturalistic fallacy. Just because it’s “natural” does not make it better. In the case of cannabis for cancer, the only potentially promising way forward is to isolate the active components and figure out which of the hundreds of different cancers in which these components have activity against.
Finally, I have no objection to lobbying for the legalization of marijuana for recreational use. I would support such measures myself. However, trying to use hugely exaggerated claims of medicinal benefit as a back door path to legalization gets my skeptical antennae all a’twitchin’ about all the other claims made by advocates and provides ammunition for critics whose real goal is prohibition.
Next installment: More testimonials analyzed.

