If scientific evidence guides our health decisions, we will look back at the vitamin craze of the last few decades with disbelief. Indiscriminate use is, in most cases, probably useless and potentially harmful. We are collectively throwing away billions of dollars into supplements, chasing the idea of benefits that have never materialized. Multivitamins are marketed with a veneer of science but that image is a mirage – rigorous testing doesn’t support the health claims. But I don’t think the routine use of vitamins will disappear anytime soon. It’s a skillfully-marketed panacea that about half of us buy into.
Not all vitamin and mineral supplementation is useless. They can be used appropriately, when our decisions are informed by scientific evidence: Folic acid prevents neural tube defects in the developing fetus. Vitamin B12 can reverse anemia. Vitamin D is recommended for breastfeeding babies to prevent deficiency. Vitamin K injections in newborns prevent potentially catastrophic bleeding events. But the most common reason for taking vitamins isn’t a clear need, but rather our desire to “improve overall health”. It’s deemed “primary prevention” – the belief that we’re just filling in the gaps in our diet. Others may believe that if vitamins are good, then more vitamins must be better. And there is no debate that we need dietary vitamins to live. The case for indiscriminate supplementation, however, has never been established. We’ve been led to believe, through very effective marketing, that taking vitamins is beneficial to our overall health – even if our health status is reasonably good. So if supplements truly provide real benefits, then we should be able to verify this claim by studying health effects in populations of people that consume vitamins for years at a time. Those studies have been done. Different endpoints, different study populations, and different combinations of vitamins. The evidence is clear. Routine multivitamin supplementation doesn’t offer any meaningful health benefits. The parrot is dead.
This week’s Annals of Internal Medicine published three papers on multivitamins, with a frankly written editorial that should not surprise regular readers of this blog: Enough Is Enough: Stop Wasting Money on Vitamin and Mineral Supplements:
The large body of accumulated evidence has important public health and clinical implications. Evidence is sufficient to advise against routine supplementation, and we should translate null and negative findings into action. The message is simple: Most supplements do not prevent chronic disease or death, their use is not justified, and they should be avoided. This message is especially true for the general population with no clear evidence of micronutrient deficiencies, who represent most supplement users in the United States and in other countries.
While these papers have generated a lot of press, the findings are not surprising. They are consistent with what the accumulated scientific evidence already tells us: there is no compelling reason for most people to take regular vitamin supplements. At best there are an expensive placebo. At worst, they may be harmful.
The U.S. Preventive Services Task Force (USPSTF) Systematic Review
One of the three papers isn’t actually new, as I reviewed it last month. Briefly, it’s the U.S. Preventive Services Task Force Report update to its 2003 guidance on the use of multivitamins, entitled “Vitamin and Mineral Supplements in the Primary Prevention of Cardiovascular Disease and Cancer: An Updated Systematic Evidence Review for the U.S. Preventive Services Task Force“. The intent of this review was to examine the evidence for vitamin and mineral supplementation in community-dwelling, nutrient-sufficient adults. They studied the effect of supplementation on two major killers: cardiovascular disease (CVD) and cancer. Thousands of papers were searched and those of the highest quality were compiled:
- Multivitamin supplements: 4 trials and 1 cohort study
- For individual or paired supplements: 18 trials and 5 cohort studies
Overall, multivitamins were found to have no effect on cardiovascular disease or cancer risk. If there is an actual effect, it’s too small to measure in these trials, and too small to be meaningful. From a risk perspective – there was no clear signal of harms from multivitamin supplementation.
Individual supplements also lacked a sound evidence base. There was no evidence of harm or benefit from vitamins A, C, or D, folic acid, calcium (with or without Vitamin D), or selenium. There was more data with beta-carotene, enough to demonstrate that it clearly has no meaningful effects, except in high-risk groups, where it is associated with an increase (yes, an increase) in cancer risk. The evidence for vitamin E was also clear – there were no beneficial effects. The takeaways from this review were stark. Multivitamins have no established role to play in the prevention of cardiovascular disease and cancer. There is currently no persuasive evidence to suggest that routine supplementation offers any meaningful benefits. The USPSTF review joins a long list of studies (1,2,3,4,5,6,7,8,9,10) that have come to similar conclusions.
The Physicians’ Health Study II (PHS II)
The PHS II was a massive study designed to study the effects of vitamins on a number of chronic diseases. This paper reported on the effects of a daily multivitamin on cognition, a secondary outcome in the study. This is another area where the evidence for vitamins has been unimpressive – mainly negative findings albeit with some positive results. The PHS II recruited 5947 male physicians, aged 65 or older. Patients were randomized to beta-carotene or placebo; synthetic vitamin E (400IU) on alternate days, or placebo; vitamin C 500mg daily, or placebo; or a multivitamin (Centrum Silver) or placebo. Patients were assessed through telephone interviews that measured cognition ever 3 years, and followed for a total of 12 years. The reports for beta carotene and vitamins C and E (for cardiovascular disease and for cancer) have been previously reported, with no meaningful benefits shown. This study looked at the multivitamin treatment with Centrum Silver – about 2 900 were randomized to each group.
There was good follow-up with participants and the adherence rate was high, with about 84% of each group taking at least 2/3 of their doses. The findings were also clear – there were no differences between the groups for any outcome at any evaluation, starting with the first cognitive assessment right through to the final assessment about a decade later. The same was observed for verbal memory: no differences between the groups at any assessment. With a very large study of such high quality, we can draw clear conclusions: supplementation with a multivitamin in a generally healthy group of older males appears to have no benefit. If multivitamins have any effect on cognition, then it was too small to be detectable.
The Trial to Assess Chelation Therapy (TACT)
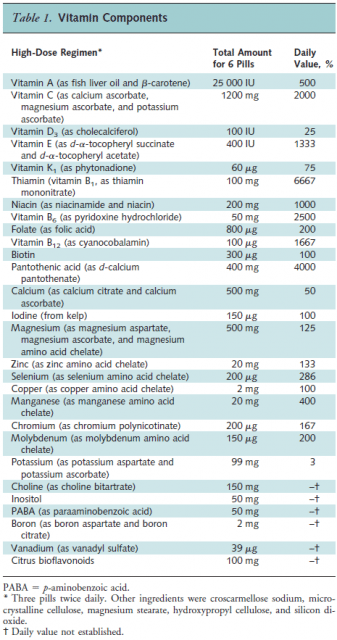
The last trial is the most infamous of all, one that SBM editor Kimball Atwood argued was “unethical, dangerous, pointless, and wasteful.” TACT was a $30 million NCCAM-funded phase 3 trial that assessed chelation therapy versus placebo and high-dose vitamins versus placebo, for the treatment of patients that recently had a heart attack. Both chelation and high-dose vitamins are the darlings of alternative medicine providers who believe these therapies can treat coronary artery disease: not just modestly, but dramatically. The scientific evidence says otherwise: outside of treating heavy metal toxicity, chelation is quackery. There are several posts at Science-Based Medicine on the myriad of problems with the TACT trial, including its ethical issues, its misleading consent process, and the fact that some of the investigators were convicted felons. Few academic research centers participated in this trial. Instead, investigators (who appeared to be advocates of chelation) relied on recruiting from a network of over 130 small centers, some of which already administered chelation treatments and other pseudoscientific treatments. Sites included the “Institute of Integrative Medicine” in New Jersey, an “Integrated Wellness” center in Maine and the “Center for Complementary Medicine” in New York. While designed to be double-blind, there were questions as to whether this blinding could have been maintained effectively. Overall, 1 708 patients aged 50 or over were recruited, all of whom had a heart attack at least six months previously. The vitamin intervention was a massive 28 ingredient supplement – 3 caplets, twice daily, which according to the trial authors, was “designed to reflect the vitamin regimen commonly used by chelation practitioners” giving doses that were in some cases significantly higher than the recommended daily value:
There were significant problems during the study period. Recruitment was difficult and consequently the target number was reduced. What was expected to take three years to enroll, took seven. In total, 853 patients were randomized to vitamins, 855 to placebo. The endpoint studied was the time to the next major cardiac event (e.g., heart attack) or death. Subjects were followed for a median of about 5 years. The problems didn’t end with recruitment. The lead investigators had to plead with site investigators to spend more time actually tracking and following patients, as they noted as recently as 2007 [PDF]:
Over the last year, the number of patients that have stopped their infusions and vitamins has increased dangerously. If our patients do not receive their treatments, then there is no chance that we could show a difference between groups.
And in what looks like some sort of grade school homework assignment, the investigators even published a list of “Helpful Websites for Finding Patients” to encourage investigators to track patients down that had dropped out of the study. Despite their efforts, the discontinuation rates were indeed dismal: 46% of participants stopped therapy, with no difference between the placebo and the vitamin arms (Perhaps it was the burden of taking six caplets per day.) In the final analysis, no significant difference was found between the high-dose vitamins and placebo for any of the endpoints, including death, or any cardiovascular event. On the positive side, however, the high-dose vitamins were well tolerated and no obvious harms were found. This time, the design and implementation was defined by alternative medicine proponents – and vitamins still failed to deliver any meaningful benefits.
The response from vitamin advocates
As expected, vitamin purveyors don’t take criticism of their product lightly:
The editorial demonstrates a close-minded, one-sided approach that attempts to dismiss even the proven benefits of vitamins and minerals. It’s a shame for consumers that the authors refuse to recognize the real-life need for vitamin and mineral supplementation, living in a fairy-tale world that makes the inaccurate assumption that we’re all eating healthy diets and getting everything we need from food alone. We would not suggest that vitamin supplements are a panacea for preventing chronic disease, but we hope the authors would agree that there is an appropriate place for supplements. Given that government research repeatedly demonstrates that the typical consumer diet is falling short on critical nutrients, vitamin supplements are an appropriate option to meet those needs.
– Steve Mister, President and CEO of the Council for Responsible Nutrition (CRN)
The intention of supplements is to supplement the diet. Don’t expect supplements to cure the common cold or prevent cancer, but they are part of the puzzle of a healthy lifestyle.
– Cara Welch, Sr VP of Scientific & Regulatory Affairs for Natural Products Association (NPA)
It’s telling that advocates won’t directly address the elephant in the room: these products, when studied, demonstrably offer no meaningful health benefits. What the evidence does say is that there is no established role for indiscriminate supplementation, and that they appear to contribute nothing to a healthy lifestyle.
But when it comes to making excuses for supplements, no-one can bring the hysterics like Mike Adams of Natural News:
To make sure these multivitamin studies fail to produce positive results, these studies are universally structured so that they are based on cheap, low-grade, synthetic vitamins and inorganic minerals. Not coincidentally, these brands of low-grade multivitamins are actually manufactured by companies owned by pharmaceutical interests. They really do have a financial incentive to make multivitamins look bad, and so their multivitamin formulations are intentionally designed to fail.
It’s clear Adams didn’t really read the studies at all. If he did, he’d see that Pfizer actually does sell the supplement used in the PHS II study – it’s called Centrum Silver, and a negative trial is probably not what Pfizer is looking for. And guess who designed the supplement used in the TACT study? The TACT authors note:
…complementary and alternative medicine practitioners rather than clinical researchers or supplement companies designed the specific components of the oral treatment regimen, leading to a unique high dose mixture.
TACT was a close as we will probably ever get to seeing a vitamin trial designed by alternative medicine proponents. Furthermore, none of the studies were driven by, or sponsored by, the pharmaceutical industry. The TACT study was sponsored by NCCAM, a regulator with a long history of boosting and supporting supplement use. And why does Adams think these trials repeatedly show that routine supplementation has no meaningful effects? He doesn’t actually refute with actual data. Cue the conspiracy music:
Let’s get down to the real motivation in all this, however. The Annals of Internal Medicine and the scientists behind this extremely deceptive junk science all share the same intention: they want you to trust in drugs, not multivitamins.
Which is an odd statement to make, as I don’t see the Annals or any “scientist” suggesting we should substitute vitamins with drugs for any of the conditions studied. The science is in fact very clear on this point: The healthiest approach, and the science-based approach, is to obtain your vitamins from your food – not from supplements.
Conclusion
Three new papers published in the Annals of Internal Medicine add to an accumulated body of research that has studied the health effects of routine vitamin and mineral supplements in healthy populations. The best available evidence gives us good, reliable information to conclude that multivitamins offer no meaningful health benefits to the generally healthy consumer. It’s time to bring an end to the era of indiscriminate multivitamin use.
References
Guallar E., Stranges S., Mulrow C., Appel L.J. & Miller E.R. (2013). Enough Is Enough: Stop Wasting Money on Vitamin and Mineral Supplements, Annals of Internal Medicine, 159 (12) 850-851. DOI: 10.7326/0003-4819-159-12-201312170-00011
Grodstein F., O’Brien J., Kang J.H., Dushkes R., Cook N.R., Okereke O., Manson J.E., Glynn R.J., Buring J.E. & Gaziano J.M. & (2013). Long-Term Multivitamin Supplementation and Cognitive Function in Men, Annals of Internal Medicine, 159 (12) 806-814. DOI: 10.7326/0003-4819-159-12-201312170-00006
(2013). High-Dose Multivitamins and Minerals After a Heart Attack, Annals of Internal Medicine, 159 (12) I-20. DOI: 10.7326/0003-4819-159-12-201312170-00001
Fortmann S.P., Burda B.U., Senger C.A., Lin J.S. & Whitlock E.P. (2013). Vitamin and Mineral Supplements in the Primary Prevention of Cardiovascular Disease and Cancer: An Updated Systematic Evidence Review for the U.S. Preventive Services Task Force, Annals of Internal Medicine, 159 (12) 824-834. DOI: 10.7326/0003-4819-159-12-201312170-00729