Editor’s Note: Dr. Gorski was on a rare vacation last week, recharging his batteries. As a result, there is no new material by him this week. Fortunately, Ben Kavoussi was ready with another in his series of posts on traditional Chinese medicine. Dr. Gorski will return next week; that is, if he doesn’t return even sooner because he can’t stand to be away from SBM for two whole weeks.
The established laws of nature do not support Oriental Medicine’s claim of Yin and Yang and Five-Phases Theory. Oriental Medicine’s main theory was constructed when our civilization had limited methods to understand our surroundings, and as such, it is only an ancient illusion.1
— Yong-Sang Yoo, MD, PhD, Chairman of the Committee for Medical Unification, Korean Medical Association, 2010
Yong-Sang Yoo is one of the strong and growing voices in Korea that is calling for an end to the national insurance coverage for Oriental Medicine.
Similarly, Professor Zhang Gongyao of the Central South China University petitioned the central government of China in 2006 to abolish support for Oriental Medicine because it has “no clear understanding of the human body, of the functions of medicines and their links to disease. It is more like a boat without a compass: it may reach the shore finally but it’s all up to luck.”2 Zhang Gongyao and fellow critics have consequently blasted China’s traditional medicine as an often ineffective, even dangerous derivative of witchcraft that relies on untested concoctions and obscure ingredients to trick patients, and employs a host of excuses if the treatments do not work.3
Bloodletting is used in Oriental Medicine to relieve excess “heat,” meaning fever, sore throat, joint pain, muscle sprain, as well as inflammation. It is often practiced in unsanitary conditions.
A Product of Archaic Thinking
The arguments of Yong-Sang Yoo and Zhang Gongyao are reminiscent of those of William R. Morse, Dean of Medical School at West China Union University, who wrote in 1934 that China’s traditional medicine was a “weird medley of philosophy, religion, superstition, magic, alchemy, astrology, feng shui, divination, sorcery, demonology and quackery.” Morse added that Chinese diagnostic methods “border on the ridiculous and possibly cross the line into absurdity.” Harvey J. Howard — a Dean at the Peking Union Medical College — also wrote in 1934 that “the great majority of these Chinese medicines reminds one of the list of remedies suggested by the third witch in Shakespeare’s Hamlet.”4
Despite its antiquated underpinnings, Oriental Medicine has survived in East Asia due to an unfortunate interplay of socioeconomic and political forces. For instance, after being outlawed during the Japanese occupation (1910-1945), the profession was resurrected in South Korea and was able to join the National Medical Insurance program in 1987. This revival is due to the Korean government’s laissez-faire policy, combined with the unified efforts and the activism of the advocates.5 In China, Oriental Medicine has a protected status that — at least in theory — guarantees it equal footing with scientific medicine.
But since the 1970s, Oriental Medicine has almost experienced some popularity in the West, although for different reasons. Once considered archaic and obsolete, Oriental Medicine has greatly benefited from the postmodern attitudes towards science and knowledge. This is because postmodernists consider the “truth” as being relative to one’s viewpoint or stance. They do not see science as a superior process of acquiring knowledge, but as a “belief system,” a “language game,” which does not give more access to truth than other conceptual constructs.6
This attitude towards science has even achieved the status of academic orthodoxy in Liberal Arts and Humanities in the last decades.7 Many proponents of “alternative” medicine use this academic attitude to reject science as a method of determining the truth about health and treatments.8 Anti-science advocates believe that these notions offer a viewpoint that is “placed in stark contrast to the naive materialism that informs some scientific points of view.”9
The proponents of unscientific medicines, however, do not realize that prior to the scientific revolution, medicine was some kind of “mass professional delusion,” as David Wootton has pointed out. Prescientific remedies, in general, did more harm than good. Wootton argues that patients sought help from physicians, not because of the efficacy of the ancient remedies, but out of desperation; because doing something was perceived as better than doing nothing.10
They also tend to forget that, as Paul Unschuld has argued, a sharp contrast between “Western” (meaning scientific) medicine and Oriental Medicine is entirely fictitious. The concepts and practices of scientific medicine have their roots not only in traditional European medicine but also in Chinese medicine, writes Unschuld. This is because modern medicine has emerged from a set of conceptual roots that once existed in Europe and continue to exist today in the Far-East. Unschuld therefore argues that by looking at Eastern medicine, modern medicine is actually looking at its own past.11
Prevalent Along the Silk Road
The conceptual similarities mentioned by Unschuld are not coincidental. Historical evidence clearly indicates that the medicine of medieval China and Europe were once intimately linked through the contribution of Middle-Easterners. Due to the importance of this rich cross-pollination along the Silk Road, the historian Paul Buell also disputes the validity of “any claims of isolation between east and west, west and east, with the individual worlds turned in on themselves.” Rather, he recognizes an ongoing “medical and other globalization of the cultures of Eurasia in the 13th and 14th centuries.”12
Indeed, the spice trade by Middle-Easterners along the Silk Road brought many herbal, animal and mineral products to Europe from the Far-East. These products were used for seasoning food, dying fabrics, making perfumes, love potions and tonics, and also for treating diseases. Often spice traders would create a sense of mystery by withholding the origins of their wares, and would ensure high prices by spinning fantastic tales about how they obtained them.13 This trade was so vital to Europeans that when it was curtailed by wars in the Near East and the conquest of Constantinople by Ottoman Turks in 1453, they decided to explore a maritime route to the spice sources westwards. In 1492, Christopher Columbus set out sail to find this route.14
As a result of the commerce between Europe and the Far-East during the Middle-Ages, it would be accurate to state that although the medieval medicine of Europe owes its origin to Greeks and Romans, a significant portion of it actually came from concepts that were commonly shared along the Silk Road. These concepts are commonly known as humorism or humoralism. It is a belief that the body is made up of several fluids (humors), and an excess or deficiency of any of them directly influences health and disposition. Diseases were not seen as forces or entities separate from the body, but as states of humoral imbalances.15
In humorism, each body fluid (humor) was associated with an organ, a quality, a temperament, etc. (Table 1). The prevalent belief was that if humors became imbalanced (dyscrasia) or unhealthy (cacochymia) illness resulted. Deficiencies and excesses or humors were diagnosed by examining the pulse, body discharges and complexion. Bloodletting, purging, enemas, nutrition, and herbal remedies were routinely used as ways to bring the humors back into balance.16
Blood was thought to be made in the liver and distributed throughout the body in the veins. Air and “vital spirits” went from lungs to the heart, where they were distributed to the tissue via arteries. The fact that a cut artery squirted blood rather than air was explained by unseen links between arteries and veins that opened upon injury. The belief was that the tissues consumed all blood delivered to them, and the liver had to make new blood continuously.17
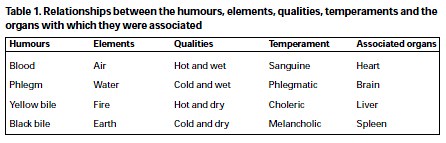
The four humors in Greco-Arabic medicine. The Chinese have a five humor system, with different but comparable relationships. Source: Jackson WA, 2001
It is important to realize that humorism was a first step towards scientific thinking and materialism. Prior to that, disease was believed to be caused by malignant supernatural forces, such as angry divinities, demons, spirits, or by witchcraft and malediction. It was the punishment for impiety and sin, or for the failure to observe religious rites and precepts. Paul Unschuld also views the advent of humorism as a shift from the “ontological” (single-factorial) view to a “functional-individualistic” (multi-factorial) view of disease.
A late medieval publication, the Fasciculus Medicinae (first printed in 1491) illustrates the most important figures of the humoral theory in medieval times.18. If you look at the books on the top shelf in this woodcut from the Fasciculus, next to Aristotle, Hippocrates, and Galen, stand Avicenna, Haly Abbas, Rhazes, Mesue, and Averroes. Pliny the Elder’s Historia Naturalis, and the books of Isaac Judaeus and Avenzoar are either open on the stand or on the table.
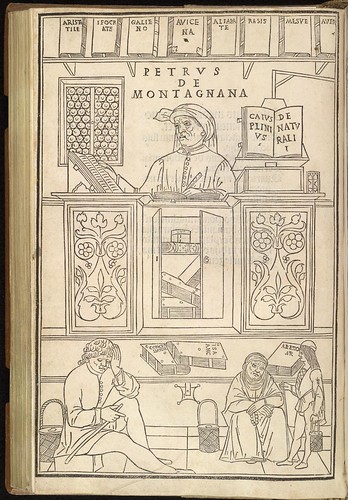
In this first printed medical text to contain illustrations, the author outlines the breadth of medical lore in 15th century Italy. This woodcut represents a scholar at the University of Padua surrounded by medical classics. Image Source: Title page from Johannes de Ketham’s Fasciculus Medicinae. Venice: J. and G. de Gregoriis, de Forlivio (Venice, 1495). Library of Congress, US.
The birthplace of the majority of these authors traces the Silk Road. Avicenna was a Central Asian, born near Bukhara in present-day Uzbekistan. Haly Abbas was from Ahvaz, in contemporary Iran. Rhazes was born in Ray, and Mesue in Gundeshapur — both in Iran. Isaac Judaeus Israeli was born in Egypt, and Averroes and Avenzoar were from Andalusia, in present-day Spain. The period of this remarkable Judeo-Islamic contribution to European medicine is from 8th to 12th century.
The most important figure during this period was Avicenna (ابن سينا, Ibn Sīnā, 980–1037), the author of the Canon of Medicine (القانون في الطب, Al-Qanun fi al-Tibb). Originally written in Arabic, the Canon was a summary of all the medical knowledge of its time. The complete compendium, or portions of it, were eventually translated into Persian, Latin, Chinese, Hebrew, German, French, and English.19
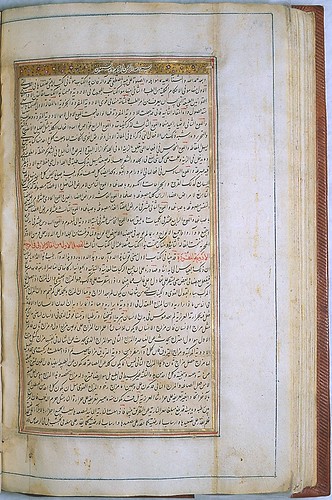
The illustrated opening page of the second book of the Canon of Medicine. Undated; probably from Iran at the beginning of 15th century. Source: The National Library of Medicine, US.
The earliest and most enduring translation of the Canon into Latin is attributed to Gerard of Cremona (c.1114–1187), who completed it in Toledo, Spain.20 Soon afterward, the influence of the Canon was permeating the writings of 13th century physicians in Europe.21 In the 14th century, medical universities made extensive use of it for teaching.22 It remained a standard reference for every medical practitioner throughout the rest of the Middle Ages.23 An improved translation was published in Venice in 1527 and was reprinted several times. In total, some sixty partial or complete editions of the Canon were published in Europe between 1500 and 1674.
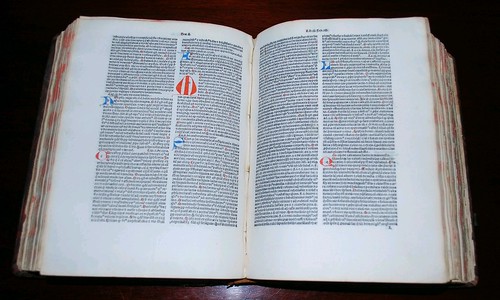
A Latin copy of the Canon of Medicine, dated 1484, at the P.I. Nixon Medical Historical Library. Image source: The University of Texas Health Science Center at San Antonio, TX, US.
Zhu Ming of Beijing University of Chinese Medicine, and Felix Klein-Franke of the Hebrew University of Jerusalem have argued that on reading the Canon, they were struck by the similarity of some of Avicenna’s writings to Chinese medical theories. Among them, is Avicenna’s theory of humors, his pathology, his remarks about how to distinguish the primary disease from the secondary, and his pulse diagnosis (sphygmology). Avicenna distinguishes 19 types of pulse, each with a quality that indicate a specific functional disorder. According to Klein-Franke and Ming, Avicenna’s sphygmology does not have much in common with Galen’s; instead, it significantly resembles Chinese pulse theory.24
In addition, the Canon makes several references to medicines of Chinese origin. Klein-Franke and Ming name 17 plants on which Avicenna wrote “imported from China” or “the Chinese type is preferable,” etc. It is therefore indisputable that Avicenna had access to, and made great use of, the medical lore of China.
Other scholars have looked at the ways in which Greco-Arabic medicine has influenced Chinese medicine. The Canon was translated into Chinese during the Yuan dynasty (1271–1368), and published along with other Persian and Arabic texts in the hui hui yao fang (回回藥方), with much of the text in Arabic.25
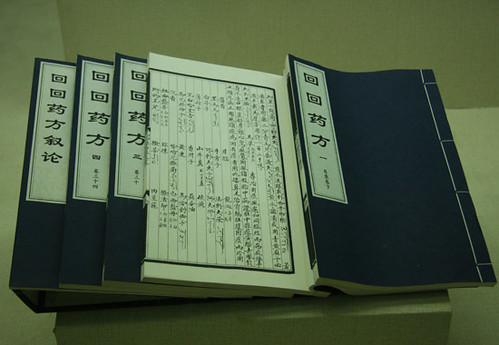
A late 15th century version of hui hui yao fang exhibited in the Chinese Hui Cultural Relics Museum. Image source: SINA Corporation, China.
The hui hui yao fang was probably the official formulary of the Mongolian administration during the Yuan dynasty. Paul Buell sees this document as a “smoking gun” of cultural influences, most of which are now untraceable, because nearly all the other relevant works have been lost. This is why the impact of Chinese medicine on Greco-Arabic medicine, and vice-versa, is widely unknown.
Avicenna is not the only medieval figure whose work shows the exchange of medical ideas and manuscripts between Middle-Easterners and the Chinese. The bibliographer Ibn al-Nadim (ابن النديم, dec. 995 or 998) writes that while a Chinese scholar was visiting Rhazes (رازی, Rāzī) in Baghdad, he translated the so-called “Sixteen Books of Galen,” i.e. the Arabic summary of the most influential books written by Galen. The fate of this translation remains unknown.26
Cultural exchanges along the Silk Road are the reason why Y. C. Kong and D. S. Chen of the Chinese University of Hong Kong write that there is an “inherent affinity between Islamic and Chinese medicines.”27 Paul Buell adds that the medical syncretism that came out of this exchange became in the Middle Ages the base of most European and Middle-Eastern practices, with influences felt as far afield as India and Africa. As seen earlier, this syncretism is apparent in the illustrations of the Fasciculus Medicinae.
Discarded After the Renaissance
Beginning in the 16th century, humorism became increasingly criticized by Renaissance scholars. Andreas Vesalius (1514–1564) was the first to publish a treatise that challenged the anatomy of Galen and Avicenna (the same year that Copernicus published, 1543 — a remarkable year). Others followed suit, including William Harvey (1578–1657), who refuted many humoral assumptions about blood in his treatise on cardiovascular circulation. Harvey measured the amount of blood pumped by the heart in one hour, and showed that it exceeds the weight of the entire body. He also showed that the valves in the heart and the veins allowed the blood to flow in one-way only, and that veins carried blood towards the heart, not towards the limbs.
In the 17th century, humorism was already synonymous with obscurantism and ignorance. The French playwright Molière (1622–1673) made great use of humoral language in writing comedies:
Now, when the vapors of which I speak pass from the left side, where the liver is located, to the right side where the heart is, it happens that the lung… having communication with the brain… by means of the vena cava… meets on its way the vapors which fill the ventricles of the scapula… and because the aforementioned vapors have a certain malignity… which is caused by the acridity of the humors engendered in the concavity of the diaphragm…28
Now compare this laughable anatomy and physiology with a paragraph on “Internal Diseases” in a prevalent textbook of acupuncture and Oriental Medicine, published in 1999.
Wind stirred up by upsurge of liver yang sends qi and blood upwards , which together with the accumulated phlegm Fire disturb the mind , leading to sudden loss of consciousness…29
The inventions and discoveries of the 18th century allowed medicine to undergo a paradigm shift. Disease became subject to new rules of classification and medical knowledge took on an unprecedented precision. Physicians began to describe phenomena that for centuries had remained below the threshold of the visible and expressible.30
Medieval notions such as Humoral pathology, vitalism and spontaneous generation were entirely discredited in the 19th century, when Louis Pasteur, Robert Koch, and others bacteriologists were able to establish indisputable links between germs and disease trough observation and experimentation. The discovery of the cellular basis of disease, and the role of microorganisms in pathogenesis made modern and scientific medicine possible.
Interestingly, as Paul Unschuld points out, when in 19th century Ferdinand von Hebra identified the mite as causing scabies, or when Agostino Bassi identified a fungus as causing silkworm disease, their ideas were initially rejected, not because they were new and revolutionary, but because they were based on a single-factorial view of disease, which then was considered to be old and outdated!
The 20th century witnessed the advent of the molecular basis of disease which addresses the chemistry of disease and recovery processes. Science has identified specific molecules that are involved in disease susceptibility, progression and prognosis, and has allowed the development diagnostic and therapeutic methods based on biochemistry. This has led to an exponential success in disease prevention and treatment, increasing the life expectancy and the quality of life of modern humans.
However, the postmodern fallacy that the science behind these spectacular achievements is merely a “language game” and a “belief system” has allowed the return of mass professional delusions under the label of Chinese, Oriental or Asian Medicine. As an unfortunate byproduct, dangerous and outdated therapies have been legitimized, and quacks and charlatans can overtly defraud those who cannot distinguish scientific medicine from lore and fantasy.
Modern purveyors of obscurantism and ignorance have also created alternative training programs, have funded biased research and publications, have accused the scientific community of corruption and conspiracy, and have spurred legislative efforts to subvert evidence-based medicine and peer-reviewed science.31
This is why responsible physicians, scientists, and public health officials in the West should follow the momentum created by Yong Sang Yoo and Zhang Gongyao in Asia, and call for an end to the licensing of Oriental Medicine practitioners. The modalities and the rationale used by these practitioners are almost identical to the ones we abandoned centuries ago. As George Ulett, MD, PhD, wrote in 2003, it is a “travesty that in this time of scientific evidence-based medicine,” treatments based on archaic thinking are given to unsuspecting patients.32
With many thanks to Daniel Bederian-Gardner, Ui-Won Hwang, Paul Ingraham, Hyunwoo Kim, Chul Koo and Robert Slack for their valuable comments or contributions. The opinions expressed here are those of the author.
References
- Yoo YS. Traditional Oriental Medicine and Integrative Medicine. Hanyang Medical Reviews 2010, Vol. 30, No. 2. Return to text
- Zhou SF. The Future of Traditional Chinese Medicine. Aust J Acupunct Chin Med 2009;4(1):23–24. Return to text
- Magnier M. Scalpel vs. Herb in China. Los Angeles Times. January 08, 2007. Return to text
- Morse WR. Clio Medica—Chinese Medicine. Paul B. Hoeber, Inc. 1934. Return to text
- Lee HJ, Jun W; Hong SP. Alternative Modernity: The Revival of Korean Oriental Medicine in Modern South Korea. American Acupuncturist; Winter2008, Vol. 46, p18. Return to text
- Lyotard JF. The Postmodern Condition: A Report On Knowledge. University of Minnesota Press. 1984. Return to text
- Boghossian P. Fear of Knowledge: Against Relativism and Constructivism. Oxford University Press. 2006. Return to text
- Stenger VJ. “Postmodern” Attacks on Science and Reality. Quackwatch. Posted 30 May 98. [Accessed 15 April 2012] Return to text
- Morris W. Medical Epistemology: A Bias of Culture?. Acupuncture Today. March, 2011, Vol. 12, Issue 03 Return to text
- Wootton D. Bad Medicine: Doctors Doing Harm since Hippocrates. Oxford University Press, USA; 1st edition. 2006. Return to text
- Unschuld PU. Traditional Chinese medicine: Some historical and epistemological reflections. Social Science & Medicine, 1987, vol. 24, issue 12, pages 1023-1029. Return to text
- Buell PD. Medical Globalization in the Mongol Era’, in T.S. Ishdorj (ed.), Mongol Sudlalyn Ogulluud, Essays on Mongol Studies, Ulaanbaatar: ‘Bembi San’ Khevleliyn Gazar (Mongolian Academy of Sciences, International Congress of Mongolists), 138–47. 2007. Return to text
- Dalby A. Dangerous Tastes: The Story of Spices. University of California Press; 1st edition. 2002. Return to text
- Turn J. Spice: The History of a Temptation. Alfred A. Knopf. New York. 2004 Return to text
- Siraisi NG. Medieval and Early Renaissance Medicine: An Introduction to Knowledge and Practice. Chicago: University of Chicago Press, 1990. Return to text
- Jackson WA. A Short Guide to Humoral Medicine. TRENDS in Pharmacological Sciences. Vol.22 No.9 September 2001 Return to text
- Unglaub Silverthorn D. Human Physiology: An Integrated Approach. Benjamin Cummings; 4 edition. 2006. Return to text
- de Ketham, J. The Fasciculus Medicinae of Johannes de Ketham, Alemanus : facsimile of the first (Venetian) edition of 1491. With English translation by Luke Demaitre ; commentary by Karl Sudhoff ; trans. and adapted by Charles Singer. (Birmingham, Ala.: The Classics of Medicine Library, 1988). Return to text
- Elgood C. A Medical History of Persia and the Eastern Caliphate. Cambridge. Cambridge University Press, 1951. Return to text
- Savage-Smith E. Europe and Islam. In: Western Medicine: An Illustrated History. London I (ed). Oxford University Press: New York. 1997. Return to text
- Siraisi NG. The Canon in the Medieval Universities. In: Avicenna in Renaissance Italy: The Canon and Medical Teaching in Italian Universities after 1500. Princeton University Press: Princeton. 1987; 44-46. Return to text
- Khan KJ. The Canon: Essential Artillery of the Medieval Medical Student. University of Toronto Medical Journal, Volume 89, Number 1, December 2011. Return to text
- McVaugh MR. Europe and Islam. In: Medicine in the Latin Middle Ages. In: Western Medicine: An Illustrated History. London I. (ed). Oxford University Press: New York. 1997; 58-59. Return to text
- Klein-Franke F, Ming Z. Avicenna’s Links with Chinese Medicine. A Chapter of the History of Sino-Arabic Relation During the Middle Ages. Asian Medicine. December 1998. Return to text
- Alpher JV, Aris A. Oriental Medicine: An Illustrated Guide to the Asian Arts of Healing. Serindia. United Kingdom, 1st Edition 1995. Return to text
- Klein-Franke F, Ming Z, Qi D. The passage of Chinese medicine to the west. Am J Chin Med. 2001;29(3-4):559-65. Return to text
- Kong YC, Chen DS. Elucidation of Islamic drugs in Hui Hui Yao Fang: a linguistic and pharmaceutical approach. J Ethnopharmacol. 1996 Nov;54(2-3):85-102. Return to text
- Poquelin JP (dit Molière). Le Médecin Malgré Lui. Editions Larousse (FR). 2007. Return to text
- Xinnong C (Editor). Chinese Acupuncture and Moxibustion. Foreign Languages Press; Revised edition. 1999. Return to text
- Foucault M.The Birth of the Clinic: An Archaeology of Medical Perception. Vintage. 1994. Return to text
- Auwaerter PG, Bakken JS, Dattwyler RJ, Dumler JS, Halperin JJ, McSweegan E, Nadelman RB, O’Connell S, Shapiro ED, Sood SK, Steere AC, Weinstein A, Wormser GP. Antiscience and ethical concerns associated with advocacy of Lyme disease. Lancet Infect Dis. 2011 Sep;11(9):713-9. Return to text
- Ulett GA. Acupuncture: archaic or biologic? Am J Public Health. 2003;93:1037. author reply 1037-8. Return to text
