
Today’s post is a reluctant challenge. I’m nominating my own alma mater, the University of Toronto, as the new pseudoscience leader among large universities – not just in Canada, but all of North America. If you can identify a large university promoting or embracing more scientifically questionable activities, I’ll happily buy you a coffee. Yes, it’s personal to me, as I have two degrees from U of T. But I’m more concerned about the precedent. If Canada’s largest university is making decisions that appear to lack a careful consideration of the scientific evidence, then what does that suggest about the scientific standards for universities in Canada?
Documenting the spread of pseudoscience within academic institutions, particularly in health and medicine, is a recurring topic at this blog. In recent years, these tactics have usually been branded as a move towards what has been called “integrative” medicine, where the apparent objective is to “integrate” unproven or disproven treatments into health programs and disciplines. It has been pointed out many times that there simply no basis or need to redefine medicine, “alternative”, “integrative” or otherwise. Integrative medicine is simply a marketing term, nothing more. This statement on alternative medicine, from Fontanarosa & Lundberg, back in 1998, still rings true:
There is no alternative medicine. There is only scientifically proven, evidence-based medicine supported by solid data or unproven medicine, for which scientific evidence is lacking. Whether a therapeutic practice is “Eastern” or “Western,” unconventional or mainstream, or involves mind-body techniques or molecular genetics is largely irrelevant except for historical purposes and cultural interest. We recognize that there are vastly different types of practitioners and proponents of the various forms of alternative medicine and conventional medicine, and that there are vast differences in the skills, capabilities, and beliefs of individuals within them and the nature of their actual practices. Moreover, the economic and political forces in these fields are large and increasingly complex and have the capability for being highly contentious. Nonetheless, as believers in science and evidence, we must focus on fundamental issues—namely, the patient, the target disease or condition, the proposed or practiced treatment, and the need for convincing data on safety and therapeutic efficacy.
– Phil B. Fontanarosa & George D. Lundberg
Academic institutions that grant legitimacy to pseudoscience create problems beyond their own walls. They do so by either lending their good name to questionable practices, or they facilitate education on pseudoscience under the rubric of “alternative” or “integrative” practices. Not only do educational standards suffer, but the affiliation gives alternative medicine practices the imprimatur of scientific legitimacy in the wider community.
What’s painful about documenting the problems with the University of Toronto is that it ought to know better. It’s the biggest university in Canada and one of the largest universities in the world, and U of T is consistently ranked among the best schools in the world. Its medical faculty and research output are highly regarded worldwide. Insulin and stem cells were discovered at U of T. Despite this stellar reputation, a recent series of decisions and announcements has made me question where U of T is headed. Is this a series of missteps, or a deliberate trend? Here are the four reasons for my nomination:
1. The University has endorsed the study of homeopathy for treating ADHD
Last week Joe Schwarcz documented that the Dean of the Leslie Dan Faculty of Pharmacy is the principal investigator in a clinical trial examining the use of homeopathy for ADHD. In an open letter to the Dean, Heather Boon, Schwarcz and 90 other individuals (including several SBM editors and contributors) asked Boon to explain the rationale for this research. In a related column, Schwarcz noted that there has been no response yet, which is disappointing given the circumstances of this clinical trial, as Schwarcz notes:
ADHD is a serious condition that merits serious research. Apparently, the University of Toronto researchers carried out a pilot study involving homoeopathy that seemed to indicate benefit. That study, however, was unblinded, devoid of randomization, had no control group and relied on a subjective outcome, making any data derived from it essentially meaningless. Even if we were to attach some importance to the claimed reduction of symptoms, the effect was about half of that seen with conventional medication, making the homeopathic treatment clearly inferior. Furthermore the proposed study would use individualized treatments for each subject as determined by a homeopathic consultation, so at best the results would be ambiguous in terms of making any recommendation.
The study is actually to be carried out at the Riverdale Homeopathic Clinic, a private institution that also offers ear candling, cranial sacral therapy and “nosodes,” which are homeopathic versions of vaccines. No public funding is involved; support comes from a foundation dedicated to alternative medicine. Nevertheless, one wonders why with various nutritional and biofeedback treatments with significant potential for helping with ADHD needing exploration, a scientifically insolvent notion is being pursued.
Why the Faculty of Pharmacy is sponsoring a trial of homeopathy raises a number of troubling questions. And when that trial is being conducted by the head of the school, it’s even more important for Boon to explain her research. What is also troubling, and remains unexplained, is how this trial came to be approved by the University of Toronto’s Research Ethics Board (REB) (what Canadians call an IRB). Presumably the REB felt this is ethically acceptable research. This is puzzling, because homeopathy is rank quackery. If homeopathy actually works, then almost everything the Faculty of Pharmacy currently teaches its pharmacy students is wrong, as are the foundational facts of biology and chemistry. Yet despite the overwhelming implausibility of sugar pills having any medicinal effect on children with ADHD, the REB gave this trial a green light. Why?
How this trial was approved is problematic for the University and it needs to be addressed. To be clear, Boon’s research hasn’t always been favourable to CAM, and she has gone on record criticizing a popular herbal remedy. She has also given statements that are not supportive of homeopathy (see video around 2:07), making it all the more important for there to be a clear explanation for this homeopathy trial, and an detailed disclosure on how this trial was considered by the university to be ethically acceptable for children.
2. The University has established a new Centre for Integrative Medicine
In a past post I noted that the University of Toronto was establishing a new “Centre for Integrative Medicine”, which I described as the perfect Trojan rabbit to embed pseudoscience in both the pharmacy and medical schools. Here’s how it was described:
The mission of this new Centre is to facilitate, conduct, and obtain support for collaborative basic, clinical, and health services research in complementary and alternative medicine; to serve as an educational and to develop integrative curricula and educational programs on complementary and alternative medicine; to work collaboratively with other departments within both Faculties and their hospital partners to support the integration of evidence-based complementary and integrative medicine into existing clinical settings and clinical research programs.
As this is a partnership between the Faculties of Medicine and Pharmacy, I noted this was a clever strategy to truly embed alternative medicine into practice. To change the standard of medical practice, you have to target both pharmacists and physicians – otherwise one group will call out the other for quackery. Normalize CAM as part of the curriculum, and students might not even notice. The program even has an explicit intent to embed practices into teaching centres – where it’s more likely to be accepted as standard medical practice.
Since my last post there has been an update: a new head of the Centre and an explicit objective to integrate CAM and Traditional Chinese Medicine into medical practice:
Today, the University of Toronto (U of T) and The Scarborough Hospital (TSH) announced a partnership that will provide new answers for the 74% of Canadians who are using some form of complementary and alternative medicine, including traditional Chinese medicine. Called the Centre for Integrative Medicine (CIM), it will bring together researchers from U of T’s Leslie Dan Faculty of Pharmacy and Faculty of Medicine alongside health care professionals at TSH to provide evidence-driven practices. Together, U of T and TSH will create a living laboratory that will allow us to study ways to safely and effectively integrate evidence-informed complementary therapies and traditional Chinese medicine with conventional medical care.
With an appeal to popularity seemingly the rationale for this work, the University of Toronto is well on its way to starting the integration of CAM into medicine. Let’s be clear. Studying if “alternative” medicine practices actually work is important. What’s not necessary is a different evidentiary framework for evaluating them. For example, pharmacognosy is the study of natural products. It’s an appropriate (and productive) research stream, given so many therapeutic drugs have their origins in natural substances. There’s no need to study natural remedies in an “alternative” or “integrative” manner. The same scientific standards should be applied. And as has been pointed out before, the history of Traditional Chinese Medicine is an invented history – not a factual one. Studying TCM needs to start with evaluating the underlying science – which has already been found to be pseudoscience.
3. The University has announced a collaboration with the Canadian Memorial Chiropractic College
The University of Toronto has announced it will collaborate with a chiropractic school to do the following:
The Canadian Memorial Chiropractic College (CMCC) has signed an official Memorandum of Understanding to explore education and research collaborations with the University of Toronto, through the Faculty of Medicine, Leslie Dan Faculty of Pharmacy and the Faculty of Kinesiology and Physical Education.
“This collaboration shows our commitment to expanding research and educational opportunities across the health care spectrum,” said Professor Catharine Whiteside, U of T’s dean of medicine and vice-provost, relations with healthcare institutions. “We’re delighted to partner with an organization committed to improving health with an evidence-based approach.”
This is quite the coup for CMCC, which reportedly has been seeking a collaboration or affiliation with a university for decades. What’s concerning is that chiropractic lacks a sound scientific basis. Chiropractic research has produced no evidence to support the underlying chiropractic theory. While there is evidence that spinal manipulation therapy can be effective for low back pain, that treatment is not exclusive to chiropractors. Beyond low back pain, there’s no evidence that chiropractic treatments offer any meaningful benefit for other conditions. It’s possible to be an evidence-based chiropractor, as SBM contributor and chiropractor Sam Homola has taught us. Unfortunately the profession of chiropractic is not made up of Sam Homolas. This collaboration between U of T and CMCC is reminiscent of an attempt by CMCC to affiliate with York University almost 15 years ago. At that time it was noted that there were serious scientific concerns about chiropractic that made the incorporation of the school into York University inappropriate. It’s not clear what’s changed with chiropractic since that time.
4. The University gives a platform for the promotion of pseudoscientific ideas about health and medicine
It’s been noted by many that there is no such thing as “alternative” medicine, as medicine doesn’t fail to work in a conventional sense yet work in an “alternative” manner. Medicine either works or it doesn’t. What works we call medicine. The rest is either proven not to work, or is not proven to work. Despite this the University of Toronto Scarborough (a satellite campus) is hosting a conference that’s filled with pseudoscience. Coming this Saturday is Alternative Cares of Medicine, a Population Health and Policy Conference:
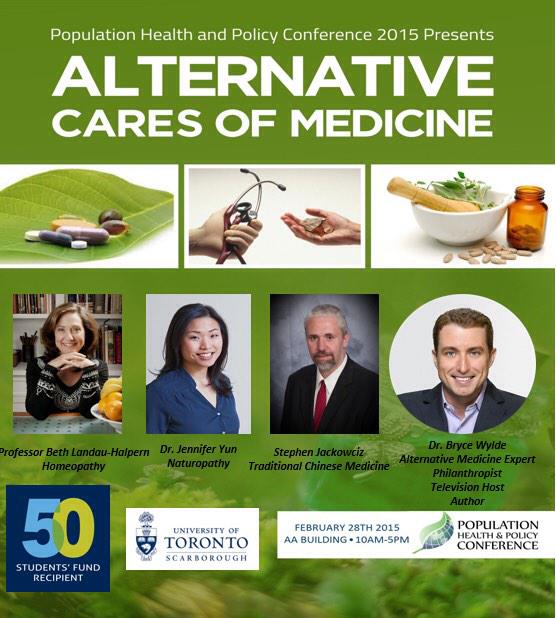
Among the speakers is Beth Landau-Halpern, a Toronto homeopath recently caught on camera by the CBC television show Marketplace selling homepathic “nosodes” to a mother as a substitute for a real vaccine. Homeopathic “nosodes” are a dangerous consequence of the pseudoscience of homeopathy. “Nosodes” are just sugar pills, like all homeopathy, but may be sold by homeopaths as substitutes for vaccination. They are not. After the Marketplace episode aired, Landau-Halpern went on record noting that while Health Canada requires nosodes to be labelled “not a vaccine”, that she is not required to do so. She knows they are not to be sold as a substitute for a vaccine, yet she did so anyway. This conference is labelled as being about population health, and given the resurgence of measles in Ontario and across North America, there is no better case study for the threat that homeopaths make to public health than examining homeopathic “nosodes” and the behaviour of homeopaths. What’s even more concerning is that Landau-Halpern actually seems to have a teaching appointment at the university. How a homeopath has obtained a teaching appointment in the Department of Anthropology at the University of Toronto is another question that the university should answer. Given the recent public outcry over a professor at Queen’s University teaching anti-vaccine pseudoscience, why the University of Toronto is sponsoring a talk by an anti-vaccine homeopath deserves an explanation.
Another speaker is Bryce Wylde, another homeopath and self-described “alternative medicine expert, philanthropist, television host” who certainly gets significant television exposure, whether it’s his own show or guest appearances on The Dr. Oz Show. He’s been criticized for repeatedly promoting ideas and treatments that lack good evidence. There’s also Jennifer Yun, a naturopath who is the co-founder and “clinical director” of Adara Integrative Clinic which offers quackery like intravenous vitamin infusions and a pseudoscience I’d never heard of, esoteric acupuncture, described by her clinic as:
Drawing upon the disciplines of Traditional Chinese acupuncture, sacred geometry, the qabbalastic tree of life, the ayurvedic nadi system, and high Qi nutrition, esoteric acupuncture brings the subtle and finer aspects of Qi (vital energy) into balance.
The entire program is a cornucopia of pseudoscience, and I see little on the agenda that is going to contribute meaningfully to supporting population health. It’s not surprising to see this program is also sponsored by the Toronto School of Chinese Medicine and the Canadian College of Naturopathic Medicine. It’s a clever way to leverage the credibility of the university while promoting your particular form of pseudoscience.
Conclusion
Like many universities, the University of Toronto appears to be taking a new and discouraging turn towards supporting pseudoscientific ideas about health and medicine. The line between science and pseudoscience is increasingly becoming difficult to see, especially when alternative medicine and quackery is rebranded as “integrative” medicine. Yet as can be seen with the resurgence of infectious disease driven by dropping vaccination rates, there are very real consequences to promoting incorrect ideas about health and wellness. We need academic centres like the U of T to be strong societal proponents of the scientific method and the best scientific evidence, rather than using appeals to popularity to determine academic programs and collaborations. Moreover, when the university or its staff make decisions that raise questions about their judgement, the university owes the community an explanation.
