![]() Science-based medicine consists of a balancing of risks and benefits for various interventions. This is sometimes a difficult topic for the lay public to understand, and sometimes physicians even forget it. My anecdotal experience suggests that probably surgeons are usually more aware of this basic fact because our interventions generally involve taking sharp objects to people’s bodies and using steel to remove or rearrange parts of people’s anatomy for (hopefully) therapeutic effect. Ditto oncologists, who prescribe highly toxic substances to treat cancer, the idea being that these substances are more toxic to the cancer than they are to the patient. Often they are only marginally more toxic to the cancer than to the patient. However, if there’s one area where even physicians tend to forget that there is potential risk involved, it’s the area of diagnostic tests, in particular radiological diagnostic tests, such as X-rays, fluoroscopy, computed tomography (CT) scans, and the variety of ever more powerful diagnostic studies that have proliferated over since CT scans first entered medical practice in the 1970s. Since then, the crude images that the first CT scans produced have evolved, thanks to technology and ever greater computing power, to breathtaking three dimensional-views of the internal organs. Indeed, just since I finished medical school back in the late 1980s, I’m continually amazed at what these new imaging modalities can accomplish.
Science-based medicine consists of a balancing of risks and benefits for various interventions. This is sometimes a difficult topic for the lay public to understand, and sometimes physicians even forget it. My anecdotal experience suggests that probably surgeons are usually more aware of this basic fact because our interventions generally involve taking sharp objects to people’s bodies and using steel to remove or rearrange parts of people’s anatomy for (hopefully) therapeutic effect. Ditto oncologists, who prescribe highly toxic substances to treat cancer, the idea being that these substances are more toxic to the cancer than they are to the patient. Often they are only marginally more toxic to the cancer than to the patient. However, if there’s one area where even physicians tend to forget that there is potential risk involved, it’s the area of diagnostic tests, in particular radiological diagnostic tests, such as X-rays, fluoroscopy, computed tomography (CT) scans, and the variety of ever more powerful diagnostic studies that have proliferated over since CT scans first entered medical practice in the 1970s. Since then, the crude images that the first CT scans produced have evolved, thanks to technology and ever greater computing power, to breathtaking three dimensional-views of the internal organs. Indeed, just since I finished medical school back in the late 1980s, I’m continually amazed at what these new imaging modalities can accomplish.
The downside of these imaging modalities is that most of them require the use of X-rays to produce their images. True, over the last 15 years or so MRI, which uses very strong magnetic fields and radiofrequency radiation rather than ionizing radiation to produce its images, has become increasingly prevalent. MRI is great because it produces more contrast between different kinds of soft tissue than CT scans do. However, CT tends to be superior for examining calcified organs, such as bone. (The breast surgeon in me notes that breast MRI is pretty much useless for detecting microcalcifications, an important possible indicator for cancer.) Also, MRI scans require a prolonged period of laying still in a very tight tube, which is a problem for patients with any degree of claustrophobia, although “open” MRIs are becoming increasingly available. More importantly for the quality of images, because they require a patient to lie more still than a CT, MRIs tend to be prone to more motion artifacts, which is perhaps why CT is more frequently used to image the abdomen other than large solid organs such as the liver. The point is that, although MRI is becoming more prevalent, CT scans aren’t going away any time soon. They have different strengths and weaknesses as imaging modalities and are therefore best suited for different, albeit overlapping, sets of indications.
Even so, it’s pretty amazing to consider how much these imaging modalities have changed medical practice in the last three decades. Before CT, surgeons often did exploratory surgery to diagnose a problem, often not knowing what they would find. They had to be ready for almost anything, and there were frequent surprises. (Some older surgeons lament that this has taken some of the excitement out of surgery, but there’s little doubt it’s better for the patients.) Another area where surgery used to be done routinely was in the staging of Hodgkin’s lymphoma. Patients underwent staging laparotomy, where the surgeon in essence carefully explored the abdomen, removed the spleen, and took biopsies of multiple areas in order to define precisely the extent of intraabdominal disease. Based on the results, the stage would be determined and therapy chosen. However, over the last 25 years or so, fewer and fewer of these have been done, thanks to better CT imaging and evolving practice in which more and more Hodgkin’s lymphoma patients receive chemotherapy. Indeed, during my residency I can only recall doing one or two staging laparotomies.
While CT imaging has revolutionized surgery and medicine, it is not entirely benign. Often, it requires the injection of intravenous contrast agents that can damage the kidneys and cause allergic reactions, occasionally life-threatening. Pretty much every physician is aware of these risks. Less acknowledged is the risk from the ionizing radiation from such tests, and physicians tend to downplay the risks from radiation. One exception is pediatrics, because it’s long been known that children are more sensitive to the effects of radiation than adults are, and they have much more time left in their lives for potential radiation-induced cancers to make themselves known. That is why pediatricians tend to be more judicious about the use of CT scans. In any case, by and large, CT scans require far more radiation than other imaging modalities. This concern was again brought to the fore last week by two studies recently published in the Archives of Internal Medicine, along with an accompanying editorial1,2,3. Together, these studies suggest that far more radiation is used in some CTs than is necessary and that there may be far more radiation-induced cancers due to medical tests than we would like to acknowledge. Taken together with another review article in the New England Journal of Medicine from a couple of years ago, they should make us as physicians think more carefully about how we use diagnostic imaging studies.
The NEJM review4 is useful because it gives the background in terms of typical doses of radiation for various imaging studies:
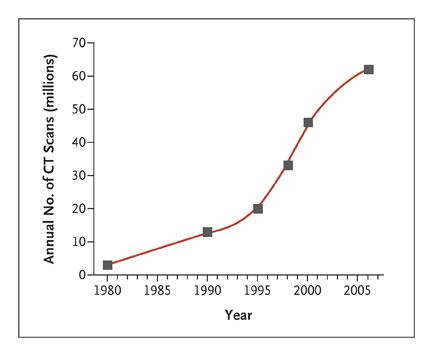
And for the huge increase in the number of CT scans being done in the U.S. every year:
That’s over 60 million CT scans performed in the U.S. in 2006. More recent data shows that 70 million scans were performed in 20072. and, for example, a typical CT scan of the chest results in an absorbed radiation dose 100-fold higher than a typical two-view PA and lateral chest X-ray. Moreover, as Smith-Bindman et al2 point out:
Exposure to ionizing radiation is of concern because evidence has linked exposure to low-level ionizing radiation at doses used in medical imaging to the development of cancer. The National Academy of Sciences’ National Research Council comprehensively reviewed biological and epidemiological data related to health risks from exposure to ionizing radiation, recently published as the Biological Effects of Ionizing Radiation (BEIR) VII Phase 2 report.7 The epidemiologic data described atomic bomb survivors, populations who lived near nuclear facilities during accidental releases of radioactive materials such as Chernobyl, workers with occupational exposures, and populations who received exposures from diagnostic and therapeutic medical studies. Radiation doses associated with commonly used CT examinations resemble doses received by individuals in whom an increased risk of cancer was documented. For example, an increased risk of cancer has been identified among long-term survivors of the Hiroshima and Nagasaki atomic bombs, who received exposures of 10 to 100 milli-sieverts (mSv).8-11 A single CT scan can deliver an equivalent radiation exposure,12 and patients may receive multiple CT scans over time.13
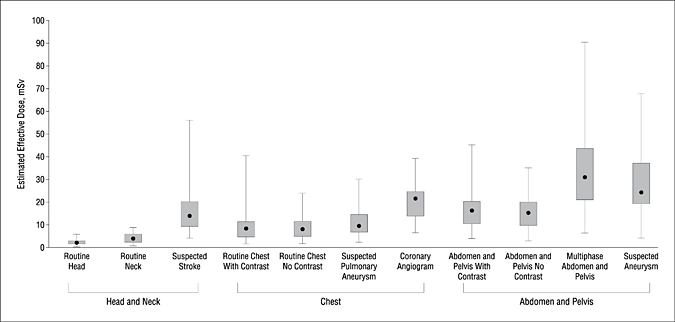
They then observe that few studies have tried to quantify rigorously the typical real-world doses of radiation received in hospitals due to CT scanning. Most studies, other than for CT coronary angiography, have used phantoms rather than patients. So Smith-Bindman et al2 looked at imaging studies in four San Francisco-area hospitals, one of which was at UCSF, and used a method called the “effective dose” to quantify radiation exposure in consecutive studies. What was most shocking is what they found regarding the variability in radiation exposures both within and between institutions even for the same test. Indeed, they noted a mean 13-fold variation between the highest and lowest radiation dose for each study type:
This particular plot type, known as box-and-whiskers, shows the 25th to 75th percentile range in the boxes, while the bars show the range between the highest and lowest values, with the median value being represented by the dots. The investigators then estimated the increased excess risk of cancer for these radiation doses and concluded:
Among 40-year-old women, 1 cancer would occur among 8105 patients who underwent a routine head CT scan (IQR, 1 in 6110 to 1 in 9500). For a 60-year-old woman, the risks were substantially lower and varied from approximately 1 in 420 examinations for CT coronary angiography (IQR, 1 in 370 to 1 in 640) to 1 in 12 250 examinations for a routine head CT scan (IQR, 1 in 9230 to 1 in 14 360). For a 20-year-old woman, the risks were substantially higher and varied from approximately 1 in 150 examinations for CT coronary angiography (IQR, 1 in 130 to 1 in 230) to 1 in 4360 examinations for a routine head CT scan (IQR, 1 in 3290 to 1 in 5110).
These are not insignificant risks. It should be noted, however, that this study has several weaknesses. The biggest weakness is that the cohort studied (1,119 patients) was not large enough to identify possible reasons why the dose of radiation varied so much for even the same tests, including experience of the technologist, physician availability to check the studies and determine the need for additional imaging, geographic variation, imaging algorithms available or used, and patient factors (such as weight). The authors point out that far more standardization is required and that studies are needed to figure out why there may be such variation in radiation dose.
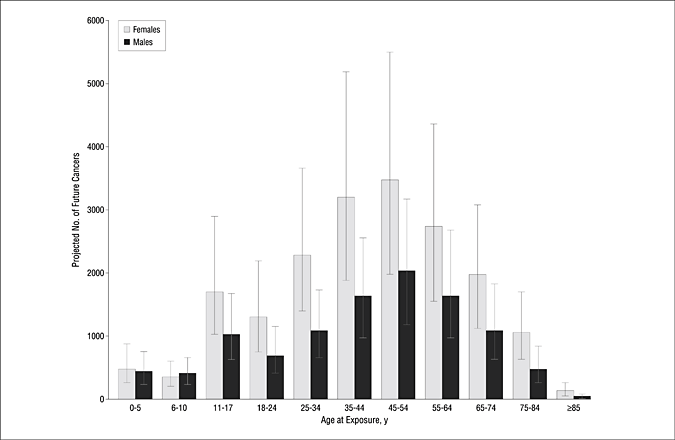
The second study drives home the point that radiation from CT scans can increase cancer risk by using different methodology. Berrington et al1 started with risk models based on National Research Council’s “Biological Effects of Ionizing Radiation” report and organ-specific radiation doses derived from a national survey were used to estimate age-specific cancer risks for each scan type and then combined these models with age- and sex-specific scan frequencies obtained from insurance claims data and surveys. Using a Monte Carlo simulation, they then estimated the number of excess cancers due to radiation from CT scanning. Their conclusions:
Overall, we estimated that approximately 29,000 (95% UL, 15 000-45 000) future cancers could be related to CT scans performed in the US in 2007. The largest contributions were from scans of the abdomen and pelvis (n = 14,000) (95% UL, 6,900-25,000), chest (n = 4100) (95% UL, 1,900-8,100), and head (n = 4000) (95% UL, 1,100-8,700), as well as from chest CT angiography (n = 2,700) (95% UL, 1,300-5,000). One-third of the projected cancers were due to scans performed at the ages of 35 to 54 years compared with 15% due to scans performed at ages younger than 18 years, and 66% were in females.
This graph tells the tale:
The black bars are for men; the white for women. Women tend to have a higher sensitivity to the effects of radiation in cancer production.
One thing that is very important is to put these figures in perspective. 29,000 is a huge number, but compared to the number of new cancer cases every year (estimated to be 1.5 million in 2009, down from earlier years). Indeed, Berrington et al1 estimate that their study suggests that approximately 1% to 3% of cancers in any given year can be attributed to past CT use. Another thing that is very important is that these results are due to a simulation, which is very dependent on the values inputted and the assumptions made in constructing the simulation. The estimates of the number of CT scans. For example, for solid tumors the assumption was a five-year lag period and a linear dose-response model. I’m not sure how valid that assumption for lag time is, given that there are quite a few tumors with longer lag periods after radiation exposure. Still, overall, this study likely represents a fairly good estimate of how many additional cancers there are due to CT scanning, but it is just that, an estimate. It also does not provide any information to tell us which cancers were actually caused by radiation from a CT scan. Neither of these studies do; they’re both population-based and look at aggregate statistics. Even so, the possibility that as many as 3% of adult cancers might be due to radiation from medical imaging studies is a problem that should sober even the most gung ho advocate of using such studies, particularly considering that the risk tends to be higher in younger people.
All of this brings us back to what I started this post with: All of medicine is a balancing of risks versus benefits. One reason I was so disturbed by the proliferation of whole-body imaging studies being marketed by unscrupulous companies on a cash basis is because, in an asymptomatic patient, the risks from radiation from such studies on average probably outweigh any conceivable benefit, especially if we take the risks of false positives leading to invasive tests such as biopsies into account. Still, there is no doubt that CT scans are highly beneficial when it comes to diagnosing disease and, these days, to guiding physicians in doing less invasive needle biopsies for diagnosis where before a surgical biopsy might have been required. That leaves the question: What to do with these results?
One approach to reducing radiation exposure from medical imaging would be to be to try to standardize imaging studies more, so that the dose of radiation for each one varies less, and, even more importantly, to find ways to decrease the dose of radiation for each test without sacrificing image quality or diagnostic sensitivity or specificity. The authors of both studies agreed on these tactics. However, far more difficult will be tactics designed to change physician behavior.
Clearly, the first thing we as a profession should do is to make ourselves very aware that a CT scan (or any scan involving a significant radiation dose) is not an entirely benign thing. We sometimes do treat them that way, and this must stop. There are several strategies to reduce the risk from these imaging studies. One obvious one, of course, is to order fewer studies and to stop ordering them for questionable indications. Critical to this approach would be better data and studies that help us clearly define when such tests are appropriate and indicated; i.e., a more rigorous application of science-based medicine to medical imaging. Sadly, this is not as much the case now as it should be, as the author of the accompanying editorial3, Dr. Rita Redberg, points out:
In addition, it is certain that a significant number of CT scans are not appropriate. A recent Government Accountability Office report on medical imaging, for example, found an 8-fold variation between states on expenditures for in-office medical imaging; given the lack of data indicating that patients do better in states with more imaging and given the highly profitable nature of diagnostic imaging, the wide variation suggests that there may be significant overuse in parts of the country.4 For example, a pilot study found that only 66% of nuclear scans were appropriate using American College of Cardiology criteria—the remainder were inappropriate or uncertain.5
Indeed, medical imaging is highly profitable. Moreover, sometimes laziness rules. It is easier just to order a CT scan than to use more mundane methods of trying to figure out what’s wrong with a patient, and the current malpractice climate often leads to physicians practicing “defensive” medicine, part of which may involve, for example, ordering a CT scan for a patient with abdominal pain “just in case” even when it’s known that the diagnostic yield is likely to be very low. At the risk of getting myself in trouble, I’ll point out that patients, too, bear some of the blame, just as they do for the overuse of antibiotics that leads to resistant organisms. Some just won’t be reassured without an imaging study; although they might be if they were more carefully informed of the increased risk of cancer from medical imaging studies. In any case, all of these factors combine to drive the explosion in CT imaging, which has increased faster than evidence of its benefit.
Finally, it is critical to remember that, for individual patients, the risk of any single imaging study is pretty low, and the potential benefit, when the study is ordered appropriately according to science- and evidence-based guidelines, will almost certainly far outweigh the slightly increased risk of cancer. For example, if you’re in the emergency room with severe chest pain, the last thing you should be worrying about is the radiation you’ll receive from a cardiac catheterization and angioplasty. Even if your chance of developing cancer from the radiation is increased by 1 in 100, that pales in comparison to your chance of dying now if your blocked coronary artery isn’t identified and opened up. If you’ve been in a car crash and might have a lacerated spleen or liver that needs repair or might have a subdural hematoma that could squish your brain against the inside of your skull, the risk from the radiation due to the CT scans that would diagnose these problems is nothing compared to your risk of death or serious disability now.
The problem is that the indications for CT scans have expanded to the point where they are often done even when they don’t provide information that will change the course of management for a patient. For instance, it used to be that general surgeons (of which I still count myself one) could diagnose acute appendicitis in a young male (who doesn’t have female reproductive organs, disorders of which can be confused with appendicitis) by history and physical exam alone and be highly accurate doing so. Yet these days, even young men with right lower abdominal pain get a CT scan that tells the surgeon that, yes, they have acute appendicitis before going to the OR. Many patients with acute peritonitis don’t need a CT scan for a surgeon to know that they need an operation. A very ill-appearing febrile patient lying perfectly still because the slightest movement causes him intense abdominal pain doesn’t need a CT scan; most of the time, he needs a trip to the OR as soon as possible to fix whatever intraabdominal catastrophe is going on. (This reminds me of a surgical aphorism that some attendings used to use to tweak residents examining a patient with peritonitis, which went, “What are you waiting for? Even the janitor can see that this patient needs an operation!”) Unfortunately, these days it seems that virtually all patients presenting to the ER with abdominal pain get a CT scan. As Dr. Redberg points out, “more and more often patients go directly from the emergency department to the CT scanner even before they are seen by a physician or brought to their hospital room.” This approach is all too easy and seductive, and all too often even general surgeons have allowed it to become the rule rather than the exception because it’s far easier to wait for the CT scan than to get out of bed to determine if a patient really needs a CT scan. Indeed, back when I still did general surgery call and chastised an ER doc for ordering a CT scan that I didn’t consider indicated, the response was that all the surgeons there wanted a CT before he even called them about a patient with abdominal pain and would get irate if he didn’t have one. This happened over ten years ago.
The bottom line is that, when the test is indicated based on guidelines constructed using science and evidence, the benefits of doing a CT scan or other medical imaging procedures requiring similar amounts of radiation outweigh the risks. The problem is that all too often these scans are not ordered using science-based guidelines and in all too many cases the evidence is not clear that doing a CT scan will improve patient outcomes. Clearly, we require more and better studies that define when the benefit of doing a CT scan outweighs the risk from the radiation. In the meantime, physicians and patients need to be aware of data like these regarding the risk of cancer due to radiation from CT scans, and physicians need to exercise some restraint and–dare I say?–clinical judgment when deciding to order these tests.
MORE INFORMATION:
The NCI Factsheet on Computed Tomography: Questions and Answers
REFERENCES:
1. Berrington de Gonzalez, A., Mahesh, M., Kim, K., Bhargavan, M., Lewis, R., Mettler, F., & Land, C. (2009). Projected Cancer Risks From Computed Tomographic Scans Performed in the United States in 2007 Archives of Internal Medicine, 169 (22), 2071-2077 DOI: 10.1001/archinternmed.2009.440
2. Smith-Bindman, R., Lipson, J., Marcus, R., Kim, K., Mahesh, M., Gould, R., Berrington de Gonzalez, A., & Miglioretti, D. (2009). Radiation Dose Associated With Common Computed Tomography Examinations and the Associated Lifetime Attributable Risk of Cancer Archives of Internal Medicine, 169 (22), 2078-2086 DOI: 10.1001/archinternmed.2009.427
3. Redberg RF (2009). Cancer risks and radiation exposure from computed tomographic scans: how can we be sure that the benefits outweigh the risks? Archives of internal medicine, 169 (22), 2049-50 PMID: 20008685
4. Brenner DJ, & Hall EJ (2007). Computed tomography–an increasing source of radiation exposure. The New England journal of medicine, 357 (22), 2277-84 PMID: 18046031