Tag: overdiagnosis

The return of marketing hype for “whole body scans”…now with AI!
Two decades ago, I cut my skeptical teeth countering advertising for whole body scans by companies making extravagant promises for their products. This particular medical fad faded for a while, but now it's back with a vengeance...with AI! Looking at these products, what I see is basically the quackery that is functional medicine on steroids and powered by AI.

Antivaxxers misuse the Defense Medical Epidemiology Database to demonize COVID-19 vaccines
Over the last couple of weeks, a claim that the Defense Medical Epidemiology Database (DMED) shows that COVID-19 vaccines have caused a massive increase in cancer, neurological, and cardiovascular diseases in military personnel has gone viral. A closer look shows that the increases are almost certainly spurious and due to underreporting in previous years.

The Frenetic Frenum Freeing Frenzy
What problems do tongue-ties cause? Do all of them need to be clipped?
We are not “losing the war on cancer” (belated 2021 edition)
The narrative we hear time and time again is that we are "losing the war on cancer". The latest cancer statistics show that this narrative is not true.

Melanoma: A Pseudoepidemic of Skin Cancer Prompts New Screening Recommendations
There appeared to be an epidemic of melanoma skin cancer, but it seems to be a pseudoepidemic caused by overdiagnosis. Screening everyone with skin exams does more harm than good and can no longer be recommended.
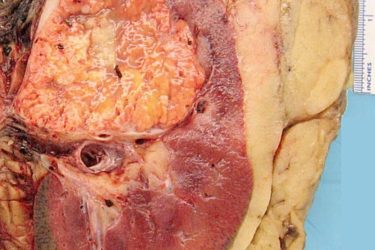
Kidney Cancer and Incidentalomas
Kidney cancer diagnoses are increasing but there has been no increase in mortality or rate of metastases. Kidney cancer is most often diagnosed as an incidental finding on a CT scan that was done for unrelated reasons. Treatment may not always be needed.
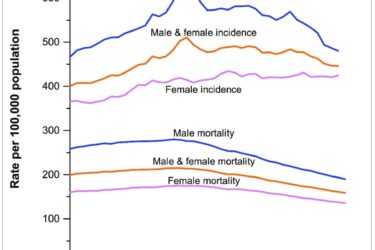
Cancer Death Rate Continues to Decline
The new data are in – cancer deaths continue to decline at a steady rate.

Osteopenia: When Does Decreased Bone Density Become a Disease Requiring Treatment?
Osteoporosis is routinely treated with bisphosphonates to prevent fractures. A new study suggests that osteopenia should be treated too. But questions remain.
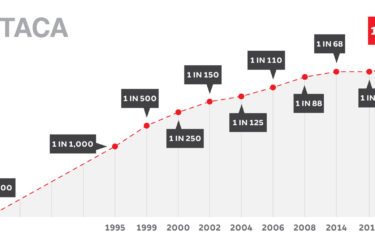
Autism prevalence increases to 1 in 59, and antivaxers lose it…yet again
Autism Awareness Month isn't as full of news stories about autism with false balance between science and antivaccine pseudoscience advocates as it was in years past. Every few years, though, when new autism prevalence figures are released, we can count on antivaxers losing it. 2018 is just such a year.

PSA Screening for Prostate Cancer
PSA testing is controversial. A new study finds that PSA screening for prostate cancer offers no survival benefits.

