Tag: surgery
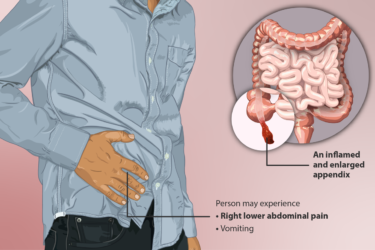
Appendicitis: Surgical vs. Medical Treatment
Surgery or antibiotics for appendicitis? This new study can help with the decision.

Bouffant caps versus skull caps in the operating room: A no holds barred cage match
Over the last few years, AORN and the American College of Surgeons have been battling it out over AORN's 2014 guideline that has increasingly led to the banning of the surgical skull cap in the operating room in favor of the bouffant cap. Lacking from this kerfuffle has been much in the way of evidence to support AORN's guideline, but unfortunately that...

Alternative medicine kills cancer patients, “complementary” edition
By definition, alternative medicine has not been shown to be effective or has been shown to be ineffective. Thus, alternative medicine is ineffective against cancer and can best be represented as either no treatment at all or potentially harmful treatment. It is thus not surprising that cancer patients who choose alternative medicine have a higher risk of dying from their cancer. A...

Alternative medicine kills cancer patients
By definition, alternative medicine has not been shown to be effective or has been shown to be ineffective. Thus, alternative medicine is ineffective against cancer and can best be represented as either no treatment at all or potentially harmful treatment. It is thus not surprising that cancer patients who choose alternative medicine have a higher risk of dying from their cancer. A...

You’ve been diagnosed with breast cancer. How soon do you need treatment?
Timely surgery for breast cancer is obviously better than delaying surgery, but how long can a patient safely wait for surgery once diagnosed. Because a randomized controlled clinical trial to answer this question would be unethical, this has been a difficult question to answer. Fortunately, a new study provides an estimate of how much of a delay it takes before outcomes start...
Worshiping at the altar of the Cult of the Brave Maverick Doctor
One of my favorite television shows right now is The Knick, as I described before in a post about medical history. To give you an idea of how much I’m into The Knick, I’ll tell you that I signed up for Cinemax for three months just for that one show. (After its second season finale airs next Friday, I’ll drop Cinemax until...
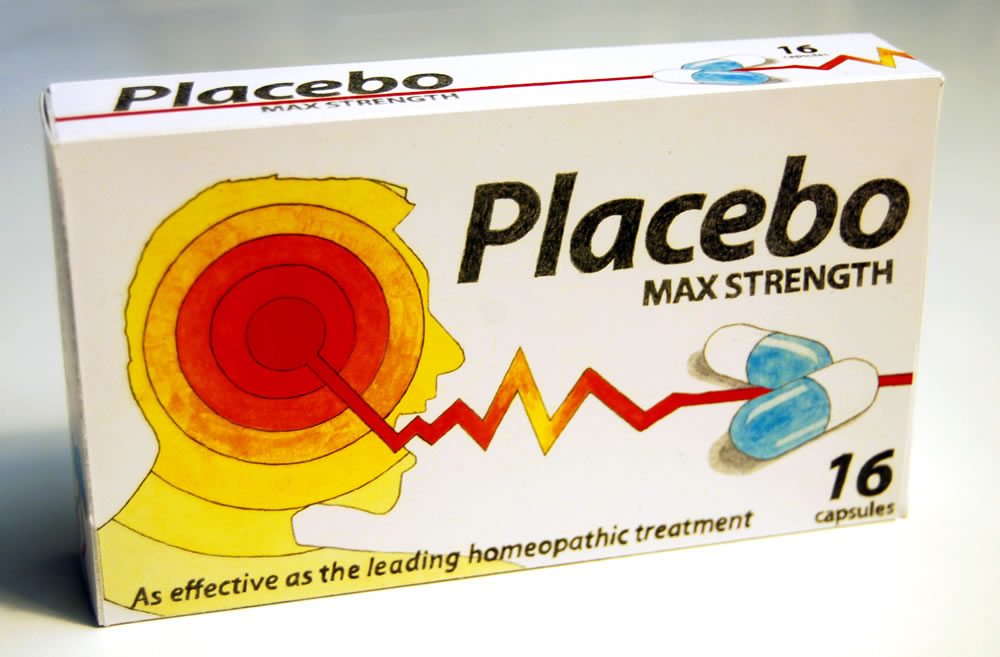
Should placebos be used in randomized controlled trials of surgical interventions?
Trials of new experimental drugs frequently compare them to placebo, particularly when there is a large subjective component to the disease being treated, such as pain. In contrast, placebo-controlled trials are rarely undertaken in surgery, mainly because it's been considered ethically dicey to do sham surgery on one group. Should this change? Should we be more open to doing randomized, placebo-controlled surgery...

Breast cancer myths: No, antiperspirants do not cause breast cancer
Antivaccine activists frequently claim that aluminum salts used as adjuvants in vaccines cause autism. However, if you listen to the quacks and cranks, that's not all aluminum does. Oh, no, that nefarious metal is also being blamed for breast cancer. But don't throw away your antiperspirant just yet. The evidence cited to support this connection is utterly unconvincing. Much of it even...

Medicine past, present, and future: Star Trek versus Dr. Kildare and The Knick
I love the new Cinemax series The Knick, which is set in 1900 and portrays a brilliant maverick surgeon named Dr. John Thackery on the cutting edge of medicine at the time. I also love Star Trek's Dr. "Bones" McCoy and have recently come to like the old radio show featuring Dr. Kildare. Looking at how the three shows portray medicine in...
When urgency to cure beats research ethics, bad things happen
Editor’s note: Just for your edification, here’s a “bonus” post. True, you might have seen this recently elsewhere, but it’s so appropriate for SBM that I couldn’t resist sharing it with those of you who might not read the other source where this was published recently. 🙂 I’ve written a lot about Stanislaw Burzynski and what I consider to be his unethical...

