“Complementary and alternative medicine” (CAM), now more frequently referred to as “integrative medicine” by its proponents, consists of a hodge-podge of largely unrelated treatments that range from seemingly reasonable (e.g., diet and exercise) to pure quackery (e.g., acupuncture, reiki and other “energy medicine”) that CAM proponents are trying furiously to “integrate” as coequals into science-based medicine. They do this because they have fallen under the sway of an ideology that posits a false dichotomy: To practice true “holistic” and “preventative” medicine, physicians and other health care professionals must embrace the pre-scientific, pseudoscientific, or anti-scientific ideas about medicine that underlie much of the “alternative medicine” being “integrated.”
Unfortunately, they’ve been largely successful over the last 25 years or so. From my perspective, the strategy that has been the most effective in mainstreaming quack practices as part of “integrative medicine” has been what I like to call the “rebranding” of practices that could and should be part of standard, science-based medicine. I’m referring, of course, to nutrition and dietary interventions, as well as lifestyle interventions, specifically exercise. To the extent that standard medicine might have undervalued such interventions over the past few decades, we practitioners of science-based medicine might be said, to some extent at least, to have brought this on ourselves. On the other hand, it is not as though doctors haven’t been advising our patients to quit smoking and moderate their drinking and to lose weight through altering their diet and exercising more for many decades. We do this because we know it works. For instance, when some naturopathic quack touts “curing” type II diabetes with a vegan diet plus exercise, we know that can work because we know that losing weight can normalize blood sugar values in many cases of type II diabetes. Heck, the Endocrine Society itself even says so, declaring “lifestyle optimization” as “essential for all patients with diabetes” and recommending that all patients with type II diabetes “strive to attain and maintain an optimal weight through a primarily plant-based diet high in polyunsaturated and monounsaturated fatty acids, with limited intake of saturated fatty acids and avoidance of trans fats,” that they lose weight through physical activity, and get enough rest. A vegan diet just takes that dietary advice to an unnecessary extreme, and any supplements recommended are almost always unnecessary.
Yet, through the wonders of “integrative medicine,” these sorts of diet and lifestyle interventions are “rebranded” as somehow “alternative” or “integrative” and then wedded to all sorts of quackery, like acupuncture, reiki, and dubious supplements. This “rebranding” unfortunately allows the respectability of effective interventions to be commingled with treatments based on prescientific vitalism or pseudoscience, like acupuncture. Worse, these science-based interventions end up being blended with the same sort of nonsense. For instance, I’ve often said that yoga is simply a system of exercise if you strip it of its mystical ideas of kundalini, which are based in vitalism. Ditto Tai Chi. I’ve often noted that exercise, at least gentle exercise, is good for almost everything, most importantly, general health, and speculated that yoga or Tai Chi is unlikely to be any better than other forms of exercise that encourage and develop similar levels of cardiovascular fitness and musculoskeletal flexibility. But yoga and Tai Chi are “cool,” “hip,” and “alternative.” So they’re sexier, but probably no more effective than other similar interventions, as a paper in published in the Annals of Internal Medicine showed.
Tai chi versus osteoarthritis
Tai Chi, for those of you unfamiliar with it, is a martial art that combines slow, deliberate, graceful stretching with breathing exercises, relaxation, and visualization. I’ve also discussed a seemingly positive study published in the New England Journal of Medicine looking at Tai Chi as an intervention in fibromyalgia patients. At the time, I pointed out that fibromyalgia symptoms could potentially be helped by exercise, and that Tai Chi, therefore, would appear to be at least as good a candidate exercise regimen as any because of its gentleness, requirement for control, and relaxation. It is not at all unreasonable to hypothesize that Tai Chi might benefit patients with fibromyalgia, as it does appear to benefit some patients with other conditions, although not for any reasons of “energy flows” or alterations of the flow of qi. I was actually underwhelmed, asking “What is ‘alternative’ or ‘complementary’ about any of these findings?”
Similarly, it’s not unreasonable to hypothesize that gentle isometric exercise might benefit patients with osteoarthritis of the knee, and physical therapy is already known to be an effective intervention. That’s why I was interested to note on the National Center for Complementary and Integrative Health (NCCIH) blog a reference to a study that was described thusly: “Study Shows Tai Chi and Physical Therapy Were Equally Helpful for Knee Osteoarthritis.” Of course, NCCIH sells this study as Tai Chi being “as helpful as physical therapy in reducing pain and improving physical functioning.” After what I’ve heard from a lot of integrative medicine advocates touting Tai Chi for all manner of ills, I can’t help but refer to the study as having found that Tai Chi is no better than physical therapy. The actual study was published in the Annals of Internal Medicine by a research group mainly based at Tufts University, along with recommendations for patients, both as Online First prepublications.
One thing I can’t help but point out here is that one of the key prerequisites for doing a comparative effectiveness study for two interventions is that both interventions need to have been validated in randomized clinical trials as being safe and effective. So it’s only natural to ask whether Tai Chi reaches that bar. The authors state in their introduction:
Tai Chi is a multicomponent traditional Chinese mind–body practice that combines meditation with slow, gentle, graceful movements; deep diaphragmatic breathing; and relaxation (6). Previous studies have indicated that Tai Chi can reduce pain and improve physical and psychological health among patients with chronic rheumatic disorders, such as rheumatoid arthritis and fibromyalgia (7–13). In our previous randomized trial, participants with knee osteoarthritis who completed 12 weeks of Tai Chi showed greater improvements in pain, physical function, depression, and health status compared with an attention control group (12). A 2013 updated meta-analysis of 7 studies that included 348 participants with osteoarthritis showed significant reductions in pain and improvements in physical function after 8 to 24 weeks of Tai Chi training compared with a waiting list, attention control, or usual physical activity (14).
Those prior trials suggested that Tai Chi could provide a practical exercise regimen with an integrative mind–body approach to manage knee osteoarthritis. The physical component provides exercise benefits that are consistent with recommendations for knee osteoarthritis (physical function, balance, and muscle strength) (15), and the mind component promotes psychological well-being, life satisfaction, and improved perceptions of health (9, 16). To date, however, no randomized trials have directly compared Tai Chi and standard care treatments. The primary goal of this study was to compare the effectiveness of Tai Chi versus a physical therapy regimen among a large sample of patients with symptomatic and radiographic knee osteoarthritis who were seen in the clinical setting and followed for 12 months.
The one thing that stands out here is that none of the Tai Chi studies listed had anything resembling a proper control group. They all compared Tai Chi with wait list, usual activity, or attention groups, which means, in essence, that Tai Chi was compared to no specific treatments with physical activity above and beyond what patients normally did. The NCCIH itself is less sanguine about the benefits of Tai Chi for osteoarthritis, summarizing the science, citing a single small 2009 randomized study funded by the NCCIH that found that Tai Chi was associated with “improvement in pain and physical function as well as in depression and health-related quality of life when compared to participants enrolled in an education and stretching program.”
Personally, although I’m not entirely convinced that Tai Chi is all it’s cracked up to be for osteoarthritis, it does appear to be a modality worth testing in comparative effectiveness research.
Tai chi versus physical therapy for knee osteoarthritis: The cage match
So let’s look at the study itself. Its design is pretty straightforward as these things go: A randomized, single-blind comparative effectiveness trial comparing standard physical therapy with Tai Chi for 52 weeks. Patients were randomly assigned to either Tai Chi (2 times per week for 12 weeks) or physical therapy in a clinical setting (2 times per week for 6 weeks, followed by 6 weeks of rigorously monitored home exercise). If you want the gory details of the design of the clinical trial, they were published in 2014 at BMC Complementary and Alternative Medicine. The primary outcome measured is pain as estimated by the Western Ontario and McMaster University (WOMAC) Index pain subscale. Secondary outcomes measured include WOMAC stiffness and function domain scores, lower extremity strength and power, physical performance tests, psychosocial functioning (mental health, self-efficacy, stress, depression, mindfulness, and social support), durability of effect after treatment ends, healthcare utilization, outcome expectation, adherence, and occurrence of adverse events.
The study population consists of 204 people ≥ age 40 who meet the American College of Rheumatology criteria for symptomatic knee osteoarthritis confirmed by the study rheumatologist and who have radiographic evidence of knee osteoarthritis confirmed by a radiologist. Exclusion criteria include prior experience with Tai Chi or other similar types of complementary and alternative medicine such as Qi Gong or yoga, or prior experience with physical therapy programs for knee OA in the past year; serious medical conditions that limit their ability to safely participate in either the Tai Chi or physical therapy programs; any intra-articular steroid injections or reconstructive surgery in the three months prior to baseline screening on the most severely affected knee (study knee); any intra-articular hyaluronic acid injections in the six months prior to baseline screening; inability to pass the Mini-Mental Status examination; or inability to walk without a cane or other assistive device for the entire duration of the baseline assessments. Pregnancy and inability to speak English were also exclusion criteria.
The interventions to which subjects were randomized included either Tai Chi or physical therapy. The Tai Chi instructors taught Yang-style Tai Chi, which is apparently the most popular of the five main styles of Tai Chi and looks like this:
The Tai Chi taught to the subjects was standardized, and the investigators condensed the 108 postures of classical Yang style Tai Chi to 10 forms that could be learned by older subjects with knee osteoarthritis within 12 weeks, selecting these forms because they are easily learned, represent progressive degrees of stress to postural stability, and are likely to improve physical function without unduly stressing the knee joints. In contrast, the physical therapy sessions consisted of a personalized program developed by one of the physical therapists after assessment of the diagnostic and physical findings to address specific treatment goals developed collaboratively and consistent with current evidence-based recommendations. After six weeks, the participants transitioned to an at home exercise program. For both groups, along with primary and secondary outcomes, changes in medication use were tracked.
Overall, 1,195 patients were prescreened for participation, leading to 282 being assessed, of which 204 met the eligibility criteria and were randomized. The mean age was 60 years. Of these, 70% were women, and the racial/ethnic composition was diverse (53% white). Participants were pretty well-balanced.
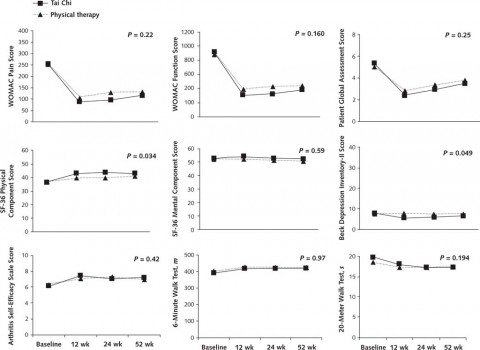
Overall, the results are summarized in the graphs below (click to embiggen):
As you can see, most of the differences between Tai Chi and physical therapy are not statistically significant, and those that are turn out to be small in magnitude, as you can see. Given that, it’s important to keep in mind that this study is only single-blinded. Only the research study nurses, physical function assessors, and sponsor personnel were blinded to the treatment assignments, while the participants, obviously, knew what group they were in, as did the Tai Chi instructors and the physical therapists. This led the investigators to concede:
Limitations of this research include patients’ awareness of their treatment group assignment and preconceived notions of treatment benefit potentially influencing their health and functional outcomes. For a study involving complex, multicomponent mind–body therapy, searching for and finding a feasible, useful, and valid sham comparison group remains challenging, with no well-accepted solution (40). Our study was necessarily single-blinded, a design with well-known limitations. To try to mitigate the influence of preexisting beliefs and expectations about the relative benefits of the interventions, we explicitly informed potential participants that the study was designed to test the effects of 2 different types of exercise programs. By emphasizing equipoise, we hoped to decrease expectations and minimize bias by not mentioning Tai Chi specifically. Using the Outcome Expectations for Exercise Scale to assess the possibility of bias, we found that participants’ expectations of benefit from their randomly assigned treatment regimen were similar (Tai Chi, 3.9 [SD, 0.5]; physical therapy, 3.9 [SD, 0.6]). Furthermore, total session attendance rates were similar between groups (74% for Tai Chi and 81% for physical therapy).
Of course, the participants knew what they were getting after they were randomized and could easily have evolved as they continued in their assigned program over the course of 52 weeks. Personally, I consider the single-blind nature of the study to be likely enough to explain the two seemingly positive results found, which were basically the ones most susceptible to placebo effects. In addition, one glaring weakness in the study that I can’t help but note is that the subjects using Tai Chi were instructed twice a week for 12 weeks before being on their own, while the physical therapy group only had therapy with a physical therapist for six weeks before being set loose on a “monitored” exercise program, whatever that meant. It almost seems as though clinical trial was set up in a way designed to minimize the effect of physical therapy relative to Tai Chi. I rather suspect that insurance considerations might have played a role, as insurance tends to be reluctant to pay for more than 4-6 weeks of physical therapy for anything, and insisting on more would have necessitated a funding source to pay for the additional sessions.
Tai chi versus physical therapy: A draw but a victory of rebranding
This study’s results simply reinforce what I’ve been saying all along. For the most part, gentle exercise and joint mobilization are gentle exercise and joint mobilization and the specific form they take doesn’t much matter, as long as care is taken to make sure they are not potentially injurious. It surprises me not at all that this study found a course of Tai Chi and physical therapy to be basically the same in effectiveness at relieving pain and stiffness due to osteoarthritis of the knee. Had I known about this trial when it was first announced, that’s the result I would have predicted.
So what’s the problem?
Here’s the problem. The vitalistic component of Tai Chi is being touted as the reason why it’s seemingly more effective at alleviating depression. For instance, see this quote by an “integrative physiotherapist” named Patricia Ladis in an article about the study:
“Top factors that determine physical therapy success have been getting 7-9 hours of sleep while in treatment, and connecting with their physical therapist. This is in contrast to “Tai Chi, where you are in an introspective space,” she emphasized. “You can be quiet in your mind as you explore and focus on the movements of your body.”
Ladies offered “that is a hugely beneficial thing for healing from pain. A quiet mind leads to a quiet body. Similar to the beneficial effects of meditation, someone in a daily introspective practice like Tai Chi or Yoga can have great health benefits.”
And:
“Sometimes people can not even endure Tai Chi because any global movement hurts, and in those cases physical therapy is crucial,” said Ladis. “Tai Chi is a great movement practice and has been very efficient at restoring proprioception and balance that physical therapy aims to accomplish. But it is also balancing to the mind and mobilizes the chi (energy) of the body which is crucial when we have degenerative changes and as we age. This is why this ancient practice is adopted by many and has helped so many. I believe for prevention or post physical therapy, Tai Chi can be very beneficial,” she added.
No, no, no. If Tai Chi is as effective as physical therapy in relieving pain and stiffness due to osteoarthritis, it’s because of the exercise, because it mobilizes the affected joints in a gentle manner. Chi has nothing to do with it, but, thanks to the rebranding of exercise as somehow “integrative” or “alternative” through Tai Chi, Qi Gong, or yoga, woo is legitimized, and you get even orthopedic surgeons characterizing Tai Chi as “more holistic than traditional physical therapy offered in North America” and going on to say:
Romeo further explained that “Tai Chi as taught by Tai Chi masters includes a very holistic approach to the person, including not only the physical requirements, but also the balance in mental health, whole body stability, meditation, breathing, and mind-body focus or connection. This helps people develop more positive mental attitudes and well-being, which is likely to also play a role in overall recovery from the stress musculoskeletal impairment.”
No, exercise works, whether it’s Tai Chi, yoga, Qi Gong, or the regimen developed by a physical therapist. No woo is needed, but that’s not how studies like this are reported by CAM advocates.
Unfortunately, “rebranding” works.