Why haven’t we cured cancer yet?
If we can put a man on the moon, why can’t we cure cancer?
If we can harness the atom, why can’t we cure cancer?
How many times have you heard these questions, or variants thereof? How many times have you asked this question yourself? Sometimes, I even ask this question myself. Saturday was the two year anniversary of the death of my mother-in-law from a particularly nasty form of breast cancer, and, even though I am a breast cancer surgeon, I still wonder why there was nothing in the armamentarium of science-based medicine that could save her from a several month decline followed by an unpleasant death. That’s why, to me at least, the timing of the publication of a study examining the genome of prostate cancer that was published in Nature and summarized in this Science Daily news story was particularly apt. Performed as part of the National Cancer Institute’s Cancer Genome Project, the study undertook complete genome sequencing of seven advanced and aggressive prostate cancers. The results, as ERV put it, revealed what can be describe as a “train wreck.”
Personally, I’d describe it as looking as though someone threw a miniature grenade into the nucleus of a prostate epithelial cell. You’ll see what I mean shortly.
Of course, although that image does give you an idea of the chromosomal chaos in the heart of prostate cancer cells, it is inaccurate in that it implies a sudden explosion, after which the damage is done, and if there’s one thing we know about cancer it’s that in most cases it takes many years for a normal cell to progress to a cancer cell fully capable of metastasizing and killing its host. I’ve written in detail about the complexity of cancer before, of course, and have even pointed out before that when President Nixon launched the “war on cancer” 40 years ago scientists had no idea how difficult it would be. Indeed, before I discuss the current study, it’s probably useful to reiterate a bit why, in order to put the study in context.
Cancer is not a single disease, and cancers are different
I’m sure that it probably becomes tiresome for readers to read this time and time again, and, believe me, sometimes I find it tiresome to keep repeating it, but it must be said: Cancer is not a single disease. It’s hundreds of diseases. Although there are many common themes in cancer, such as loss of responsiveness to growth signals with a resultant ability to grow unchecked. Other common capabilities of cancer cells include evasion of programmed cell death (apoptosis), inducing the surrounding tissue to provide a blood supply (angiogenesis), evading the immune system, and invading the blood or lymphatic systems to travel elsewhere in the body and take up shop in other organs, such as liver, lung, or bone. Although there are, again, common molecular themes by which cancers do this, individual cancers acquire these necessary (to the cancer) abilities by many different ways.
Even cancers arising from the same cell type can be quite different. For instance, the breast cancer that killed my mother-in-law was a rare spindle cell variant, which is quite different from the much more common invasive ductal carcinoma that is estrogen and progesterone receptor positive. Indeed, even within individual cancers, different populations of cells can be quite different. In many solid tumors, there are cells now referred to as “stem cells.” Personally, I consider this term a bit of a misnomer that I really don’t like because these cells are not really pluripotent, and the cell types into which they can differentiate are rather limited. Moreover, this nomenclature has also made the concept of the cancer stem cell more controversial scientifically than it really needs to be. What we are really talking about are a relatively small population of cells in many tumors that are endlessly self-renewing and, in general, resistant to chemotherapy. In mice, these are the only cells that can actually form a new tumor when transplanted into a new mouse, and these are the cells that appear to be responsible for relapse after chemotherapy and radiation therapy. Indeed, cancer progression can be viewed as being due to a case of evolution in which the tumor cells that survive selection to continue to grow are the ones that become best at doing all the things that tumor cells need to do to evade the body’s defenses and overcome its growth control signals.
One of my favorite examples of how cancer progression can be understood using evolutionary principles was a study of esophageal cancer by Carlo Maley, PhD, a researcher at The Wistar Institute, that was published nearly five years ago. In essence, Maley applied population biology principles, specifically the Shannon Diversity Index, to predict which cases of Barrett’s esophagus (a precancerous condition in which the cells lining the lower esophagus are changed by chronic inflammation such that they look more like the cells that line the inside of the stomach) are most likely to progress to invasive esophageal cancer.
Not only is cancer not a single disease, but individual cancers are made up of multiple different clones of cancer cells under selective pressure to become ever more invasive and deadly. Looking at it this way, it’s a wonder we don’t all die of cancer. We do, however, virtually all have small foci of cancer within us, as I’ve pointed out before. Yet most of us do not develop cancer, and fewer of us end up dying of cancer, even though cancer is currently duking it out with heart disease as the number one cause of death in industrialized societies. Fortunately, the steps required for cancer to become deadly are difficult and numerous, and the body’s defenses against cancer are formidable.
Mechanisms of carcinogenesis are not simple
Let’s take a trip in a time machine back to 40 years ago, around the time that Nixon signed the National Cancer Act of 1971. I was a child, and molecular biology was in its infancy. Few of the fancy tools that scientists take for granted these days when it comes to studying genes, proteins, and how they interact even existed. Heck, polymerase chain reaction (PCR)—at least, as we know it now—wasn’t even invented for another 12 years and didn’t become widespread until the late 1980s and early 1990s. (Nearly 20 years later, I still chuckle at the memory of the monster of a PCR machine, the only one in our department, that I occasionally tried to use in graduate school. The thing took up the better part of a benchtop.) In 1971, the very first oncogene discovered, src, had only been reported the previous year, and it hadn’t even been demonstrated that oncogenes were defective protooncogenes; i.e., genes involved in cell growth that were mutated in cancers. That discovery would not come until 1976. Tumor suppressor genes were not discovered until nearly 10 years later, when the retinoblastoma (Rb) gene was characterized in 1986. An even more famous tumor suppressor gene, p53 (or TP53), had been discovered in 1979 by Lionel Crawford, David P. Lane, Arnold Levine, and Lloyd Old, but had initially been thought to be an oncogene. Burt Vogelstein demonstrated its function as a tumor suppressor gene in 1989, and ultimately it was demonstrated to be a critical gene for responding to DNA damage. How that ten-year voyage from oncogene to tumor suppressor played out is described in detail here. It makes interesting reading how a scientific concept can change as new evidence comes in.
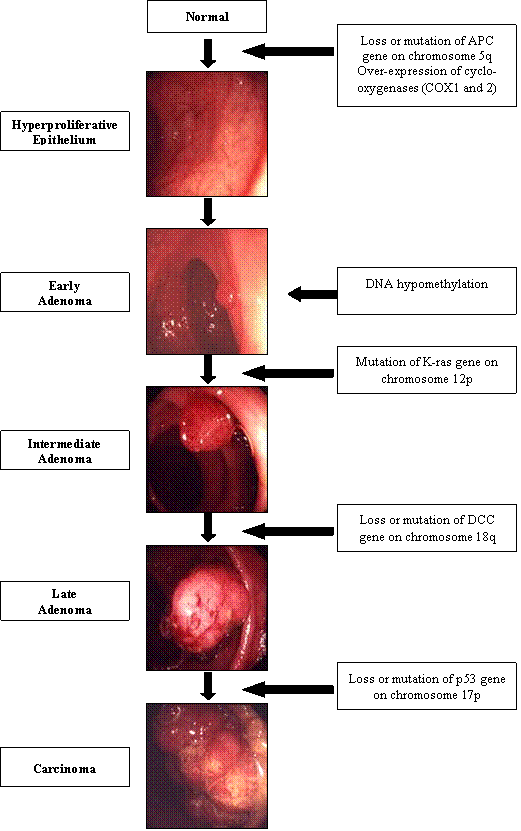
Thus, over the first 25 years or so after the National Cancer Act of 1971, it was all about the genes and mutations. The picture that began to emerge was that oncogenes drove tumor growth along with loss of tumor suppressor gene activity. This seemed to fit in nicely with Alfred G. Knudson’s “two-hit” hypothesis, which stated that not only were “hits” required in oncogenes to cause cancer but in tumor suppressors as well. Later, Burt Vogelstein developed a model of multi-stage carcinogenesis that required at least six mutations:
As you can see, things were getting pretty complicated. Even so, based on what we know now, even Vogelstein’s increasingly sophisticated models in retrospect turn out to have been fairly simplistic. We discovered this over the last decade or so, because, with the advent of expression array profiling (a.k.a. “gene chips” or “cDNA microarrays”) in the late 1990s, it became possible to measure the level of expression of thousands of genes at the same time. Before then, we did not have the computational power or the technology necessary to do this, but over the last decade or so, it’s become more apparent than ever before that it is not primarily individual genes that determine cancer, or even a handful of genes, but hundreds or even thousands of genes that form complex networks of interactions. Also, around 1998 it was discovered that there is a whole new class of RNA, known as microRNAs (miRNAs), which regulate gene expression. More recent evidence suggests that miRNA expression patterns might actually tell us more about how cancer develops than whole genome expression array profiling because individual miRNAs often regulate the expression of hundreds of genes.
And I’m not even getting into deep sequencing of whole genomes in cancer yet, or the metabolic derangements that characterize cancers and allow them to grow where normal cells cannot, derangements that are probably just as critical to the process of carcinogenesis as genetic alterations.
So, putting it all together as we understand it in 2011, cancer cells not only have mutations that result in dysregulated expression of oncogenes and tumor suppressors, but these changes result in the alteration of expression of hundreds of genes, and in different types of cancer it will be different batteries of genes and miRNAs that are messed up in different ways. In fact, in individual tumors, there will be different populations of cells with different sets of genes and miRNAs messed up in different ways. Even worse, as a tumor progresses, it tends to become more heterogeneous, meaning that the number of different populations of cells tends to increase. Looking at it this way, it’s amazing that we have been able to do as well as we have with various forms of “targeted” therapy directed at specific single molecular targets or a class of molecular targets in cancer cells. Gleevec®, for instance, has been amazingly successful as a targeted agent directed against several members of a class of enzyme known as a tyrosine kinases, and by that mechanism it has been phenomenally successful as a treatment for gastrointestinal stromal tumors and certain types of leukemia. Even hoary old Tamoxifen is a targeted therapy directed at the estrogen receptor, and it still remains a mainstay of treatment for estrogen receptor-positive cancers to this day, along with a newer class of drugs known as aromatase inhibitors.
Unfortunately, in the grand scheme of things relatively few tumors are responsive to the targeting of single agents.
The prostate cancer genome
So what does this study tell us? Basically, scientists working at the Broad Institute, Weill Cornell Medical College, the Weizmann Institute of Science, Yale University, and Harvard University completely sequenced the entire genome of seven different prostate cancers and catalogued the abnormalities found by comparing the genome in prostate cancer with that found in the white blood cells of each patient, which were used as the normal control. Of course, this is what’s known as a “hypothesis-generating” study (a.k.a. a “fishing expedition” to those more inclined to disparagement). Personally, I have no problems with “fishing expeditions,” because without them we would have a serious lack of hypotheses to test. Moreover, this sort of fishing expedition is one where, almost no matter what scientists found, they would learn something useful about prostate cancer. True, it may not be the sort of knowledge that can be translated into therapy quickly. In fact, going in I would have predicted that it almost certainly would not be the sort of understanding that would lead to rapid improvement in prostate cancer treatment, and the results of this study show that it is not. What it does show is just how messed up the genome of cancer cells tends to be.
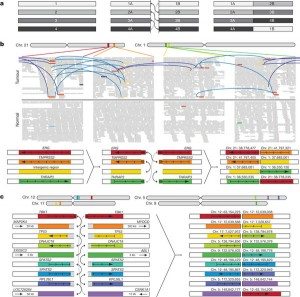
So what did the investigators find? Rearrangements and translocations. Lots and lots of intrachromosomal rearrangements and interchromosomal translocations. In fact, they found a median of 90 rearrangements and translocations per cancer genome (range: 43–213). They even included a pretty picture to represent the rearrangements. Known as a Circos plot, this graph shows the genomic location in the outer ring and chromosomal copy number in the inner ring (red, copy gain; blue, copy loss). Interchromosomal translocations and intrachromosomal rearrangements are shown in purple and green, respectively. (click on the picture to go to the Nature website and see the full size version):
These rearrangements were, as noted above, both within chromosomes (intrachromosomal) and between chromosomes (interchromosomal). These are represented in the following figure (again, click on the figure to see the full-size version):
Panel a shows an idealized picture of how these translocations work, with chromosomal breaks and rejoining with pieces of other chromosomes. It’s not necessary for me to go into the details other than to point out that in panels b an c we see that the break points have a disturbing propensity to be located right smack dab in the middle of important genes, like tumor suppressors. For instance, in PR-2832, break points appear in the middle of TP53 and ABL1. In other tumors, investigators found recurrent rearrangements that involved CADM2 and PTEN. PTEN is a known tumor suppressor gene, but CADM2 (cell adhesion molecule 2). This result appears to be confirmatory of recent results implicating CADM2 as a tumor suppressor gene in prostate cancer. Overall, scientists observed some new rearrangements, and ones that had been detected before.
Or, to put it even more simply, as William Phelps, program director for Translational and Preclinical Cancer Research at the American Cancer Society, put it:
Here’s one way to conceptualize the alteration, Phelps said: “If the genome was a book, instead of just looking for out-of-place letters or misspelled words, whole genome sequencing looks for whole paragraphs that are in the wrong place.
“Because [the researchers] sequenced everything, they were able to map not only individual base changes but also how whole genes or segments of the chromosomes had moved around,” Phelps said. “By sequencing everything and comparing the normal DNA (in white blood cells), they could see that not only were there individual base changes in the genes, but the genes themselves had been reshuffled in the tumor as part of the process of becoming cancer,” he explained.
“If we could use those changes as a diagnostic tool that would be tremendously valuable,” he added.
Whole genome sequencing also enables scientists to look not only at “coding” genes, but also “noncoding” DNA around the genes that was once thought to be “junk” but is now known to play an important regulatory role within cells, Phelps said.
I’ll admit that when it was announced, I was skeptical of the utility of the cancer genome project. I still am, actually. Basically, it’s one massive fishing expedition. However, as the years have gone by, I’ve become less skeptical, although I can’t say that I’ve exactly embraced it. This study leads me to consider that perhaps I was wrong in my original assessment.
More interesting than whether I screwed up five years ago when I first heard of this project, these sorts of rearrangements have long been appreciated as being important in leukemias and lymphomas, but in solid tumors they had not—until relatively recently. One thing that is important to keep in mind is that these scientists focused on aggressive, advanced pancreatic cancer. Consequently, they were selecting for most “messed up” genomes. As more and more cancer genomes are sequenced, scientists will be able to make comparisons between aggressive and indolent tumors. It is possible that one day doctors will be able to sequence a patient’s tumor and use what is learned from this to tell whether the tumor is aggressive or not—or potentially whether it even needs treatment or not. I’ve written extensively about the problem of overtreatment and even about spontaneous regression. Wouldn’t it be great if we could identify patterns of rearrangements and mutations (or lack thereof) that are associated with slow growing, indolent tumors compared to patterns associated with fast-growing, deadly tumors like the one that killed my mother-in-law, and then be able to use that information to target therapy or to decide that a cancer patient can be safely treated with watchful waiting? Until the last few years, we really didn’t have the technology and computing power to make such a dream a possibility, but now we do.
So why haven’t we cured cancer, anyway?
I close with the same question with which I opened. Why haven’t we cured cancer yet, anyway? Yes, I know it’s a bit of a misleading question, given that we can actually cure quite a few cancers, including several leukemias and lymphomas, which are curable with chemotherapy and radiation, and solid tumors like breast and colorectal cancer which are curable with a combination of surgery, chemotherapy, and radiation. Unfortunately, although we do fairly well (and in some cases very well) against early stage cancer, we don’t do so well against stage IV metastatic disease, particularly solid tumors. The vast majority of these are not curable, and, very likely, the vast majority are much like the prostate cancer specimens studied by these researchers, full of chromosomal rearrangements and mutations leading to abnormalities in many different signaling pathways.
Last year, the tenth anniversary of the announcement of the results of the Human Genome Project provoked a veritable flood of “Why haven’t we cured cancer yet?” or “Why haven’t we cured this disease yet?” For example, Nicholas Wade wrote a painfully simplistic article last June entitled A Decade Later, Genetic Map Yields Few New Cures. It’s an article I should have blogged about; perhaps even eight months later it would be worth doing, although you could always read this perspective instead. Let’s put it this way: The technology, techniques, and knowledge developed during the Human Genome Project laid the groundwork that has made it possible to sequence the entire genome of prostate cancer tumors and compare them this way. Come to think of it, I’m really dreading December 23, 2011. That will mark the 40th anniversary of Richard Nixon’s signing of the National Cancer Act of 1971. I just know that the month of December will be filled with stories lamenting, “Why haven’t we cured cancer yet?” or proclaiming the “war on cancer” to have been a failure. Some will be from the mainstream media, and even more will come from places like NaturalNews.com and Dr. Mercola’s website. That’s one prediction you don’t have to be a psychic to make. I also predict a whole bunch of articles and blog posts trying to claim that we’d be able to cure cancer “if only,” as in “if only” we’d be less conservative in our research approach (never mind that there are lots of high-risk approaches, and the ones that work only appear obvious in hindsight), “if only” we’d educate our kids in science better, “if only” we’d get rid of the FDA (yes, this guy was serious, as silly as his argument is), or “if only” doctors didn’t make so much money treating cancer with drugs and wouldn’t make any money treating it with “natural” therapies.
In preparation for this landmark event, I’ll begin with a pre-emptive answer (which I’ll no doubt have to repeat in December). Why haven’t scientists cured cancer yet? Leaving aside the trite answer of “Which cancer?” I can say this: Because it’s hard. It’s very, very hard. It’s harder than going to the moon; it’s harder than building the nuclear bomb; it’s harder than wiping out smallpox. All of those were, of course, also very, very hard too, but cancer is a harder nut to crack still. It’s hundreds, perhaps thousands, of diseases. Each type of cancer can be many, even dozens, of different diseases in itself. Each tumor can be many diseases that are constantly evolving, both in response to the environment in which the cancer cells grow and to treatments that are thrown at them.
And most cancer cell genomes probably look like the prostate cancer genomes analyzed in this paper. There’s a less thorough study that suggests that the breast cancer genome does.
Does that mean I have no hope? Of course not! Otherwise, I wouldn’t keep doing what I’m doing. I am simply expressing humility in the face of a protean foe that has thus far withstood our best efforts to eradicate it. That does not mean that it will continue to do so. After all, never before have we had the tools that we have now to probe deeply into the biology of cancer at the whole genome level as we do today.
Still, it will be hard.