Sometimes, weird things happen when I’m at meetings. For example, I just got home from the Society of Surgical Oncology (SSO) meeting in Houston over the weekend. Now, one thing I like about this meeting is that, unlike so many other meetings these days—cough, cough, ASCO, I’m looking at you—at the SSO there wasn’t a single talk I could find about “complementary and alternative medicine” (CAM) or, as its proponents like to call it now, “integrative medicine.” It’s also a great chance to get caught up on new science and clinical guidelines in cancer surgery, as well as to see people I tend only to see at these meetings.
However, I must admit that by the last day I tend to be “meeting-ed” out and sometimes my attention wanders. Unfortunately, there are ample ways to indulge that attention deficit. Actually, it’s my iPhone. And it’s Twitter. So it was an odd coincidence that right after a talk by Dr. Deanna Attai about whether surgical oncologists can or should offer genetic counseling services to their patients, when I somehow let myself get into an exchange with Sayer Ji, the “natural health expert” responsible for GreenMedInfo, over BRCA1 mutations and the risk of breast and ovarian cancer, in other words, exactly the sort of thing that Dr. Attai had just discussed. For example:
@ackdoc @sayerjigmi Where are your ncbi citations, or Gorski’s? Its remarkable how unicorn and not evidence-based supposed skeptics are.
— GreenMedInfo (@GreenMedInfo) March 28, 2015
After a bit of back-and-forth, I got fed up:
.@ackdoc @GreenMedInfo The sad thing is, @sayerjigmi‘s misunderstanding of genetic and biology is dangerous to patients.
— David Gorski (@gorskon) March 28, 2015
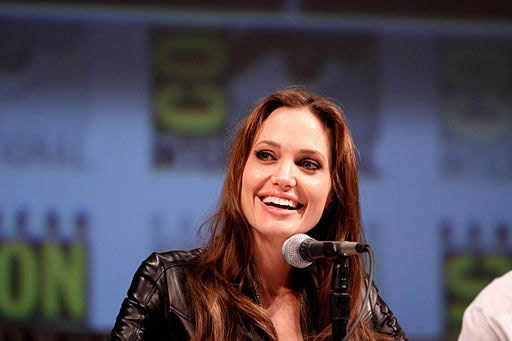
This minor Twitter exchange came about because of Angelina Jolie’s announcement in a New York Times op-ed last week entitled “Diary of a Surgery” that she had had her ovaries removed to prevent ovarian cancer due to her being a carrier of a high-risk mutation in BRCA1. As you might recall, I wrote about Jolie’s case two years ago, when she first announced in a NYT op-ed entitled “My Medical Choice” that she had undergone a bilateral mastectomy with reconstruction to decrease her BRCA1-related risk of breast cancer. Although I had discussed the story before, I thought it worth doing again here in a bit more detail.
Now, let’s just say that Ji is not known for his science-based proclamations, and he’s hostile to evidence-based medicine. Although he wields the peer-reviewed scientific literature like a sword and shield to protect his pseudoscientific blather, to anyone who actually understands the science, it’s painfully obvious that he doesn’t know what he’s talking about but is good at misunderstanding and cherry-picking studies that make it appear to lay people that he does. In particular, he’s very hostile to the concept that there is a genetic cause of cancer, as he demonstrated when Jolie first announced her mastectomy. That’s why hereditary cancers and how they are prevented really set him off. This time around, he doubles down on his genetics denialism. Ji’s cherry picking and misinterpretation of studies can be either amusing or infuriating, depending on my mood. More on that later. First let’s look at the story.
Angelina Jolie and BRCA1 mutations
Back in 2013, Angelina Jolie startled the world by announcing in a NYT op-ed that she had had both of her breasts removed to prevent cancer because she had been found to have a specific BRCA1 mutation that results in a high risk of cancer. At the time, knowing what had been disclosed by Jolie, I considered the decision to be a reasonable one, although I was not pleased with the publicity her surgery gave to the Pink Lotus Breast Center, a Los Angeles-area breast center that puts the “integrate” into “integrative medicine,” using a homeopathic concoction to prevent wound breakdown and various “detox” regimens to eliminate anesthesia from the system. Still, Jolie’s decision to decrease her risk of breast cancer this way was quite reasonable, given this:
We often speak of “Mommy’s mommy,” and I find myself trying to explain the illness that took her away from us. They have asked if the same could happen to me. I have always told them not to worry, but the truth is I carry a “faulty” gene, BRCA1, which sharply increases my risk of developing breast cancer and ovarian cancer.
My doctors estimated that I had an 87 percent risk of breast cancer and a 50 percent risk of ovarian cancer, although the risk is different in the case of each woman.
As I’ve discussed on more than one occasion, BRCA1 and BRCA2 are genes in which certain mutations are most commonly associated with either breast or ovarian cancer, although they are also associated less strongly with several other cancers as well, such as cervical cancer, uterine cancer, early onset prostate cancer (men) and colon cancer (BRCA1) or pancreatic cancer. BRCA1 codes for a protein known as breast cancer type 1 susceptibility protein, a protein belonging to the RING-type zinc finger (RNF) family whose function involves repairing damaged DNA. Specifically, it repairs double-stranded breaks. In the nucleus of a variety of normal cells, the BRCA1 protein interacts with other proteins, such as RAD51 and BARD1, to repair double stranded breaks resulting from radiation and other environmental exposures, as well as breaks that occur during natural processes, such as homologous recombination, or just from living. The BRCA1 protein is important in multiple functions, including transcription (conversion of the DNA sequence to RNA message), repair of double-stranded DNA breaks, ubiquitination, and other functions. If BRCA1 can’t repair the break, it then promotes cell cycle arrest and apoptosis (programmed cell death). The result of defects in BRCA1 function is increased sensitivity to anything that causes DNA damage and an increased risk of the development of cancer. BRCA2 encodes a protein that, while very different in structure from BRCA1, serves a similar function, namely the repair of double-stranded DNA breaks.
Mutations in BRCA1 and BRCA2 are associated with familial cancer syndromes, most commonly involving breast and ovarian cancer, but not limited to these cancers. Moreover, I must emphasize again that BRCA mutations are not binary. You do not either “have the mutation” or not “have it.” There are many mutations, some of which confer a very high risk of cancer, as high as an 87%. Indeed, family-based studies by the international Breast Cancer Linkage Consortium looking at 237 BRCA1 carrier families that have four or more members with breast cancer estimated a 72-95% (overall 87%) lifetime risk of breast cancer due to BRCA1 mutations and a 63% lifetime risk of ovarian cancer. These are high numbers. Overall, looking at a survey of recent studies that include family-based and population-based studies, BRCA1 mutations can produce a lifetime risk of breast cancer ranging from 45% to 87% and of ovarian cancer ranging from 31% to 63%. By any stretch of the imagination, these are high risks of potentially-deadly cancers.
When Jolie wrote about her decision to have both breasts removed, she did point out that she was told by her physician that she had a lifetime risk of ovarian cancer of 50%. Think of it this way. The average woman has a lifetime risk of ovarian cancer on the order of 1.8%, which makes Jolie’s estimated risk more than 25-fold elevated. In comparison, given that the average woman has a lifetime risk of breast cancer on the order of 10-12%, an 87% lifetime risk conferred to Jolie by her BRCA1 mutation is well over seven-fold higher. Again, these are high risks, and it is in the context of such high risks that considering risk-reducing prophylactic surgery becomes reasonable.
Now for the irony. As I said, this exchange with Ji occurred in the Q&A session after a talk about whether surgeons can effectively provide genetic counseling to breast cancer patients. It’s easy for surgeons like myself, who practice in large cities, particularly surgeons like myself who practice in NCI-designated comprehensive cancer centers with excellent genetic counseling programs, simply to refer patients to genetic counseling. A good genetic counselor will go through these risks and explain the significance of the dozens of mutations that are known. This complexity is why I generally have been a firm believer that genetic testing for BRCA mutations should usually not be done outside of a center with either skilled genetic counselors or a physician trained in genetic counseling who can explain the risk and help the patient weigh the pros and cons of genetic testing and, if that testing is positive, the various surveillance and preventative strategies available for women carrying such mutations. Unfortunately, there is a huge shortage of qualified genetic counselors in many states (I seem to recall Dr. Attai saying that, for example, Wyoming has none). So sometimes surgeons do need to do genetic counseling. At the very least, we breast surgeons need to know the indications for genetic counseling and how to take a proper family history. Also important is to weigh the ethical and practical issues of genetic testing, such as whether a mutation carrier should inform her family, what effects that it might have on her ability to obtain health insurance, and the many other issues that are inextricably bound with genetic testing.
In other words, as I like to say, recommendations should be personalized by practitioners using science-based practice. It should also be remembered that in the US, BRCA mutations account for only a small minority of cases of early onset breast cancer (2-3%) and ovarian cancer (8%), a proportion that can vary widely based on geography and ethnicity. To put it another way, approximately 25% of women with a breast cancer diagnosis are younger than 50 years, and almost 10% of these women will have a BRCA mutation.
There’s also the issue of just how nasty ovarian cancer is compared to breast cancer. The main reason ovarian cancer is so nasty is that it’s rarely caught when it’s confined to just the ovary or Fallopian tube. Rather, the symptoms of early ovarian cancer tend to be vague and nonspecific abdominal or pelvic complaints. Usually, it has started to spread throughout the abdomen before it is discovered, and by then the surgery needed to control it becomes much more extensive, and the chemotherapy needed to mop up the leftover tumor deposits after surgery becomes more grueling. Corresponding with this, the chances of curing ovarian cancer go down considerably. Also, unlike the case for breast cancer, there is no good screening test that has been shown to decrease mortality from ovarian cancer when applied to the general population.
Surgery is effective, too. Bilateral prophylactic mastectomy reduces the risk of breast cancer in women with high risk BRCA1 mutations by at least 90%. (See, for example, Hartman et al, 1999; Domchek et al, 2010; Rebbeck et al, 2004; Meijers-Heijboer et al 2001.) Removal of the ovaries is also highly effective in reducing mortality from ovarian cancer in such patients, lowering the risk by 70-90%. (See, for example, Kauff et al, 2002; Kauff et al, 2008; Finch et al 2014.) That prophylactic oophorectomy to prevent ovarian cancer and prophylactic bilateral mastectomy to prevent breast cancer in carriers of high-risk BRCA1 mutations are highly effective is not even controversial. Such recommendations are “baked” into major evidence-based guidelines, like those of the NCCN, as a significant option for women found to have such mutations to consider. Other options exist, such as enhanced screening (which has not been shown to be effective in ovarian cancer) or chemoprevention. Tamoxifen may decrease the risk of breast cancer in BRCA1 mutation carriers, and oral contraceptives can decrease the risk of ovarian cancer. None of these options are as effective as prophylactic surgery, unfortunately, meaning that, for carriers of dangerous BRCA1 mutations, there just aren’t any really good options.
Jolie, in her NYT article, explained why she decided to have her ovaries and Fallopian tubes removed:
TWO years ago I wrote about my choice to have a preventive double mastectomy. A simple blood test had revealed that I carried a mutation in the BRCA1 gene. It gave me an estimated 87 percent risk of breast cancer and a 50 percent risk of ovarian cancer. I lost my mother, grandmother and aunt to cancer.
I wanted other women at risk to know about the options. I promised to follow up with any information that could be useful, including about my next preventive surgery, the removal of my ovaries and fallopian tubes.
Unfortunately, as was the case last time, she also couldn’t resist layering in a bit of woo:
I did not do this solely because I carry the BRCA1 gene mutation, and I want other women to hear this. A positive BRCA test does not mean a leap to surgery. I have spoken to many doctors, surgeons and naturopaths. There are other options. Some women take birth control pills or rely on alternative medicines combined with frequent checks. There is more than one way to deal with any health issue. The most important thing is to learn about the options and choose what is right for you personally.
In my case, the Eastern and Western doctors I met agreed that surgery to remove my tubes and ovaries was the best option, because on top of the BRCA gene, three women in my family have died from cancer. My doctors indicated I should have preventive surgery about a decade before the earliest onset of cancer in my female relatives. My mother’s ovarian cancer was diagnosed when she was 49. I’m 39.
See what I mean? I’m glad that Jolie ultimately decided upon a reasonable, science-based course of action, but I really wish she could have restrained herself from including this passage and in essence representing quacks on the same level as surgeons and oncologists. Naturopaths? Need I repeat how much quackery is embedded in naturopathy? Rely on alternative medicines and frequent checks? There is no known “alternative medicine” that can reduce ovarian or breast cancer breast in BRCA1 mutation carriers; so this strategy is akin to just close surveillance, which is ineffective in ovarian cancer. And don’t even get me started on the fallacy of “Eastern” versus “Western” medicine again! How many times do I have to point out that that is a rather racist construct, in which the “East” is implied to be more “holistic” and woo-ey, while the “West” is cold, reductionist and scientific? Medicine is medicine. The only thing that matters is the evidence supporting it. Still, at least Jolie in the end made a medically-reasonable and justifiable choice to have her ovaries removed in order to prevent ovarian cancer down the road. It was probably the least bad of bad options for her, and her bringing attention to this issue is to be commended.
That is, unless you’re a quack.
Sayer Ji steps in it
Regular readers might remember that when actress Angelina Jolie first announced in a New York Times opinion piece that she had undergone bilateral prophylactic mastectomies because of her BRCA1 mutation, quacks were not pleased, not at all. For example, Mike Adams, ever the restrained one, declared “Angelina Jolie inspires women to maim themselves by celebrating medically perverted double mastectomies.” Interestingly enough, given Adams’ attempt to reinvent himself as a legitimate food safety researcher, that article might have had too much crazy in it even for him. There is now a message there about how “this article has been removed because it is no longer aligned with the science-based investigative mission of Natural News” now that Adams has “transitioned from outspoken activist to environmental scientist.” You can still find generous samples of Mike’s original rant in my original discussion of it. The text of Adams’ followup article, “How Angelina Jolie was duped by cancer doctors into self mutilation for breast cancer she never had“, has also disappeared, to be replaced by the same bizarre message. Again, you can see just how bad it was for yourself in the same discussion of this despicable article, in which Adams claimed Jolie could have reduced her risk of cancer to very low levels with “natural” methods, an utterly ridiculous claim for a woman with a BRCA1 mutation.
The reason alternative medicine mavens were not pleased with Jolie’s decision to remove first her breasts and then her ovaries to try to prevent the cancer that her BRCA1 mutation had a high probability of causing is because of what I like to term “genetics denialism.” Because alternative medicine is all about “control” (or, as I like to call it, a “Secret”-like form of wishful thinking in which we have near-absolute control of our bodies simply by willing what we want and willing ourselves to do the “right” things, eat the “right diet,” take the “right” supplements, and think the “right” thoughts,”) alternative medicine practitioners deny that genes have anything to do with disease. It’s what I refer to as the “central dogma” of complementary and alternative medicine, namely that wishing makes it so.
Often genetic denialists invoke the science of epigenetics, often with hilariously (or infuriatingly) wrong conclusions. It always comes off in much the same way that creationist tropes about “junk DNA” do: With a superficial understanding of science that, because it is so superficial, is twisted into supporting unscientific arguments. Sayer Ji is a master of this technique. No, that’s not a compliment.
What Ji lacks in Adams’ penchant for histrionics, he makes up for in verbal prestidigitation that ignores medical knowledge. He also was fast out of the gate, throwing together this article the same day Jolie’s article appeared, entitling it ‘Beware of Organ Removal for “Cancer Prevention”: Jolie’s Precautionary Tale.’ It’s basically a rehash of an older article of his, “Ovarian Cancer: What We Think We Know May Harm Us“, and both articles include the same sort of misinformation about overdiagnosis that is irrelevant to BRCA1 carriers because Ji cites studies of screening in the general population. The misinformation begins early and comes fast and furious:
With Angelina Jolie’s recent announcement that she had her ovaries and fallopian tubes removed because of both a BRCA ‘gene defect’ and a history of breast and ovarian cancer in her family, the idea that genes play a dominant role in determining biological destiny and cancer risk is proliferating in the mainstream media and popular consciousness uncontrollably like a cancer.
See the genetics denialism? Again, the idea is that you can control your health, so much so that genes don’t matter, at least not that much. Examples abound, with Deepak Chopra attacking genetic “determinism” and Mike Adams claiming that human DNA is incapable of storing the complete blueprint of the human form and referring to genetics as a “big lie.” If you listen to Ji, you’ll see he’s basically saying, “Never mind that pesky BRCA1 mutation.” He further tells women they have nothing to worry about:
The reality is that the average woman’s lifetime risk of ovarian cancer is exceedingly small, with the overall risk of developing ovarian cancer by 65 years of age being 0.8 percent and the lifetime risk 1.8 percent.[2] For those with a first-degree relative developing ovarian cancer, as is the case for Jolie, the risk estimates show increases to 4.4 and 9.4 percent, respectively.[3]
It is also important to realize that lifetime ovarian cancer risk does not exist in a vacuum. Considering that it is not cancer (at any site) but heart disease that is the #1 killer of women, focusing on ovarian cancer risk as the primary threat to health is myopic at best, faulty reasoning with deadly consequences at worse. If Jolie had chose [sic] to go without radical surgical intervention, it is statistically more likely she would have died from heart-related death than cancer of any kind. The reality is that the lifetime risk of heart disease related death in women is in top position at 23.5%, according to CDC statistics, versus cancer which takes #2 position at 22.1%. And within cancer related deaths in women, breast, lung, colorectal cancer, uterine, thyroid, non-Hodgkin’s lymphoma and melanomas are top on the list, with ovarian cancer in the 8th in position.
Can anyone spot the fallacies here? These are numbers for women who don’t have a documented BRCA1 mutation!!! They are irrelevant to Jolie’s situation, where she has a mutation that, according to her doctors, confers an estmiated 50% lifetime risk of developing ovarian cancer. The study cited by Ji was, in actuality, a case control study that only examined the three known major risk factors by history: a history of ovarian cancer in the mother or sister, years of oral contraceptive (OC) use, and number of term pregnancies. That’s it. It didn’t even look at the known BRCA1 mutation that Jolie had.
Next up, Ji goes on to discuss overdiagnosis of ovarian cancer resulting from ultrasound screening. Yes, as I’ve pointed out more times than I can remember, any time you screen for a disease, you will diagnose more cases and some of those cases will be overdiagnosed; i.e., disease that would never progress within the lifetime of the patient to cause serious health problems. He even invokes the case of ductal carcinoma in situ (DCIS), a premalignant condition of the breast whose prevalence has skyrocketed with the advent of mammographic screening. Here’s the thing. The frequency of overdiagnosis is related to the chance of disease in the population being screened. The lower the chance of disease, the greater the chance that a positive screening test results in overdiagnosis. That’s why we don’t screen women under 40 for breast cancer; the expected prevalence of disease is too low. Indeed, as I’ve discussed many times, even age 40 might be too young, hence all the controversy over the USPSTF recommendations five years ago.
Can you see where I’m leading? With Jolie’s expected lifetime risk of ovarian cancer being 50%, Ji’s discussion of overdiagnosis is also irrelevant to her case. Yes, there is a problem with screening for ovarian cancer. It doesn’t work very well, if it works at all, and there’s a lot of overdiagnosis. That doesn’t mean that it’s not appropriate to screen a woman at a risk far higher than the general population for the disease.
Ji concludes by cherry-picking evidence suggesting that BRCA1-associated ovarian cancers might be less aggressive. Indeed, it’s a point he brought up again on Twitter:
@gorskon How do you resolve the fact that there are over 500 BRCA SNPs identified, with variations like BRCA1 K1 183R reducing cancer risk?
— GreenMedInfo (@GreenMedInfo) March 28, 2015
Note that @GreenMedInfo and Sayer Ji are one in the same. Ji switched from the Twitter account under his name to his blog account during the exchange.
In his article, one study Ji cites found that it’s likely a better response to platinum-based chemotherapy in BRCA1-associated cancers that results in better outcomes. Indeed, a recent meta-analysis suggests that BRCA1 carriers who develop ovarian cancer do indeed have higher overall survival, but that such women who develop breast cancer have a worse survival (which has been known). My answer? So what? They still develop a cancer that has an unfortunately high probability of killing them! Yes, the ovarian cancers they develop might be less deadly than ovarian cancer that just “pops up,” but they’re still plenty deadly! Holy hell, Ji angers me with this line of “reasoning,” if you can call it that, that because the average woman has a relatively low chance of developing ovarian cancer, and heart disease kills far more women than ovarian cancer, it is inappropriate to try to reduce the risk of ovarian cancer in a woman with an ovarian cancer-predisposing mutation.
After that, I needed a chuckle, and Ji gave me one, namely that he thinks he understands promoter hypermethylation, an epigenetic process. Basically, he cherry picks a study that shows a lot of methylation (attachment of methyl groups chemically) to the promoter (the DNA region near a gene that controls how much protein the gene makes) silencing (shutting off) BRCA1 in ovarian cancer and concludes that BRCA1 mutations are irrelevant to ovarian cancer because epigenetics is more important:
Up until now, most of the focus on breast and ovarian cancer risk has been on the inherited BRCA1 mutations and how they interfere with proper BRCA function. The new study reveals that epigenetic processes, working from the outside in, as it were, can produce the same functional outcome as an inherited mutation. BRCA gene deactivation through hypermethylation can be stimulated through chemical exposures, such as to dioxins, for instance. There is also research indicating this can be prevented through natural compounds such as resveratrol and soy, putting diet – and so-called nutrigenomic interventions – at the forefront of cancer prevention and treatment.
Any geneticists or cell biologists out there? I know you’re there. I hope I didn’t cause you too much pain by quoting that passage. As you know, what the study cited by Ji really shows is the importance of BRCA1 in ovarian cancer and how loss-of-function can lead to cancer development in sporadic ovarian cancers; i.e., ovarian cancers not associated with a specific gene mutation. Somehow, during the process of carcinogenesis epigenetic mechanisms silence BRCA1 in a lot of ovarian cancers, which just goes to show how important BRCA1 is for the development of ovarian cancer. Now here’s the thing. High-risk mutations impair or destroy the function of the BRCA1 protein permanently, epigenetics be damned. Ji must not understand that you’re not going to restore the function of BRCA1 through epigenetics if the gene itself has a mutation in it that leads to its protein product not functioning. I don’t care how much resveratrol and soy a woman consumes.
None of this stops Ji from plumbing the depths of his ignorance of genetics near the end of his article:
The concept – the meme – that hereditary determines one’s biological destiny is archaic. After the first draft of the human genome project was completed in 2005, they only found 23,000 genes! That’s not enough protein-coding genes to explain the existence of our body, which contains at least 100,000 different proteins. What this epic failure revealed is that it is not the genes themselves that determine health or disease, rather, what factors in our environment, lifestyle and nutrition that activate the expression of certain genes, and silence the expression of others. In the case of BRCA1 and BRCA2, we now know that silencing these genes from the ‘outside in’ results in the same result as being born with a defective gene from the ‘inside out,’ with the important difference that epigenetic – ‘outside in’ – gene silencing can actually be reversed or mitigated. Our genome results from millions of years of evolution, whereas our epigenome is influenced by day to day decisions, many of which depend on what we decide to eat or avoid eating, right now. Choice, therefore, becomes central to determining disease risk. And given that Jolie’s decision to remove her breasts, and subsequently her ovaries, was predicated on a belief that she is helpless in the face of predetermined risk – her decision does not reflect the evidence and biological science itself.
How do we end up living in a world where people believe that their genes – which they do not have access to without biomedical surveillance — determine their destiny? How we end up thinking that ‘gene defects’ are so powerful that removing healthy organs from our body is the only reasonable way to prevent experiencing cancer within them?
If we take this logic to its fullest expression, why wouldn’t someone determined to have a greatly increased risk of brain cancer remove their head prophylactically?
One can only wish that Ji would take his own advice. That part about the 23,000 genes but 100,000 proteins was truly ignorant. Has Ji never heard of alternative splicing? (Speaking of which, check out this cool animation of RNA splicing.)
Yes, depending on the disease, it is not uncommonly a mixture of environment and genes that determine what happens. However, that ratio is not the same for every disease, and for many diseases it’s many genes that influence development of the disease. Single-gene diseases, like cancer due to BRCA1 mutations, are a lot less common than sporadic cancer. There’s also the concept called penetrance, which describes how likely a person harboring a certain allele or mutation is to demonstrate the phenotype (i.e. physical characteristic like height, eye color or disease) associated with that allele. 100% means everyone with that mutation gets the phenotype. 50% means half do, like Angelina Jolie’s BRCA1 mutation and ovarian cancer. It’s generally not 100% or none; penetrance is a spectrum. Ji seems to think the variable penetrance of different BRCA1 mutations means that these mutations can’t cause cancer. Some of them can and do, some of them at a very high frequency, and no amount of changing one’s diet, lifestyle, or thinking is going to reverse biology. That’s not to say that women with deleterious BRCA1 mutations shouldn’t avoid things that can increase the risk of breast cancer, such as obesity or excess alcohol consumption, but the magnitude of the expected benefit will be tiny in comparison to the magnitude of risk due to the mutations. Unfortunately, the strongest risk reduction in the case of certain cancer-predisposing mutations comes from surgically removing the organ at risk.
Sadly, in the case of BRCA1 mutations, genetics does rule, by and large. We’ve already seen that for breast cancer, depending on the specific BRCA1 mutation, the lifetime risk of cancer can be as high as 90%. The same is true for a number of mutations that vastly increase the risk of colorectal cancer to the point where the vast majority of carriers develop colorectal cancer before middle age. Examples include the familial adenomatous polyposis (FAP), which is caused by mutations in a gene called APC that results in numerous polyps in the colon at a very young age, leading to colon cancer in nearly 100% of people carrying deleterious APC mutations, and hereditary nonpolyposis colorectal cancer (a.k.a. HNPCC or Lynch syndrome), which is due to mutations in the DNA mismatch repair pathway that lead to an 80% lifetime risk of colorectal cancer. Both of these syndromes, like BRCA1, also predispose a patient to other forms of cancer at a lower penetrance. In both of these syndromes as well, strong consideration of prophylactic surgery to remove the colon and rectum at a relatively young age is recommended.
Ji’s apparent belief that genetics doesn’t matter and “choice” is all, is nothing more than The Secret of epigenetics, in which wishing makes it so and we can completely control our health, genetics be damned. If only that were true. It’s not. In fact, in the case of ovarian cancer due to deleterious BRCA1 mutations, a very important recent study (Finch et al, 2014) showed that earlier prophylactic surgery likely results in better outcomes, which suggests that Jolie might have waited a bit longer than is currently considered advisable to have her ovaries removed. That same study showed a 77% overall decrease in a BRCA1 mutation carrier’s risk of death by age 70.
By promoting such flagrant misinformation about hereditary cancer, Sayer Ji endangers the lives of women with BRCA mutations everywhere. His arguments are nothing more than pure genetics denialism.