
Trust in science and vaccines continues to decline. Why?
Recent evidence shows that public trust in science and vaccines has declined markedly since the pandemic. Why is this, and is there anything we can do about it?

What the heck happened to The BMJ? (2023 version)
The BMJ, once a bastion of evidence-based medicine, has become disturbingly susceptible to publishing biased "investigations" that feed antivax narratives. Its latest report on VAERS by Jennifer Block, who in the past has defended Gwyneth Paltrow and Goop and whose history is not one of supporting science, is just another example of this deterioration.

Robert F. Kennedy Jr. comes home to his antivax roots…again
Robert F. Kennedy Jr. gave the keynote speech at the second annual meeting of his antivax organization, Children's Health Defense. Once again, he demonstrated that not only is he still antivax as hell, but that his proposals are even more bizarre than before. Truly, it was a homecoming for him.
Study laundering: IPAK, antivax “scientists,” and the return of living dead antivax studies
Antivaxxers don't like it when one of their crappy studies that they somehow managed to sneak into a decent peer-reviewed journal is deservedly retracted, as happened to Mark Skidmore's paper that estimated that 278K people might have died from COVID-19 vaccines. Fortunately for Skidmore and others, there exist fake journals that will launder their study by republishing it so that antivaxxers can...
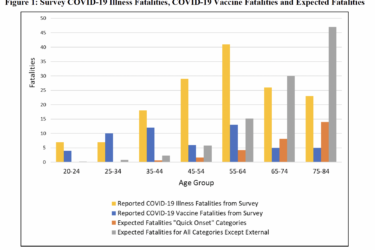
Has MSU economics professor Mark Skidmore been “exonerated” over his retracted paper claiming that COVID vaccines killed 278,000?
Tech bro turned antivax influencer Steve Kirsch is claiming that Michigan State University economist Mark Skidmore has been "exonerated" after having had a paper retracted claiming 278K deaths from COVID-19 vaccines in 2021 alone. In reality, Skidmore just republished a revised version of his retracted paper in an antivax journal after the MSU IRB failed miserably in its oversight duties.
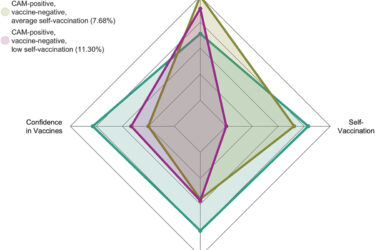
Alternative medicine and antivax: Two crappy tastes that taste crappy together—particularly when among physicians
A recent study reaffirms the high degree of correlation among physicians between antivax views and an embrace of quackery. This is an old finding that needs to be documented periodically and shows why the acceptance of non-science-based treatments by physicians endangers vaccination efforts.

He pushed hydroxychloroquine three years ago: Harvey Risch and false claim of “turbo cancers” caused by COVID-19 vaccines
Last week, I discussed Dr. William Makis' false claims of "turbo cancers" due to COVID-19 vaccines. Now it's hydroxychloroquine-promoting epidemiologist Harvey Risch's turn.
Dr. William Makis and “turbo cancer”: Falsely blaming COVID-19 vaccines for cancer
A prominent oncologist and cancer biologist, Wafik El-Deiry, recently amplified claims that COVID-19 vaccines cause "turbo cancer," wanting a "civil discourse about science and actual answers that are missing." Unfortunately, calls for "civil discourse" by an eminent oncologist about unfounded claims only lends undeserved credibility to them. So, once more into the fray...

Health misinformation now has powerful allies
Misinformation and conspiracy theories about health had long been a growing problem before the pandemic, but it took COVID-19 to get the government and researchers to take it seriously. Now, a new report in The Washington Post adds to previous reporting from multiple sources describing how allies of misinformation—and not just health misinformation—are striking back under the guise of defending "free speech."


