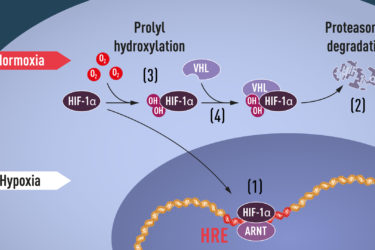
Nobel Prize in Physiology or Medicine 2019
Nobel Prize in Physiology or Medicine 2019 given to researchers who discovered the mechanisms of oxygen sensing in cells.

Fat Shaming Is Counterproductive
Fat shaming not only doesn't work, it is counterproductive. So what might help fight obesity?

Crystal Healing
Crystal healing is back and growing in popularity. What does that reveal about our society and alternative medicine?

Soft Drinks and Death Risk
New study linking soft drinks to increased mortality is correlational only, and should be interpreted with caution.
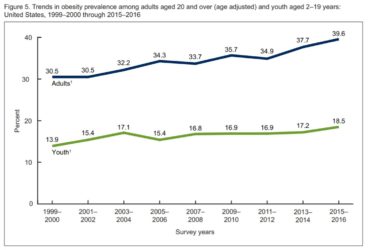
Update on the Obesity Epidemic
The obesity epidemic continues, and even accelerates, among continued debate about its causes and solutions.

Gluten Update
Non-celiac gluten sensitivity remains controversial, but the research continues.

Maternal Fluoride and IQ
New study purporting to show correlation between fluoride and IQ comes under heavy criticism.

FDA Warns About Miracle Mineral Solution
Jim Humble is still selling his industrial bleach as a fake cure, and the FDA gives another toothless warning.



Gary Null’s Attack on SBM
Gary Null's fact- and logic-free attack on SBM.