A bandwagon. Hop on, no science needed!
Earlier today, Steve discussed a new report hot off the presses (metaphorically speaking, given that it’s been published online) from the Bravewell Collaborative. Naturally, given the importance of the issue, I couldn’t resist jumping in myself, but before you read the blather I have to lay down, you really should read what Steve wrote about it. It’s that good. (Also, he’s our fearless leader, and I wouldn’t want him to be…unhappy about my having muscled in on his usual day to post.) Have you read it? Good. Now we can begin…
One of the most common (and potent) strategies used by promoters of “complementary and alternative medicine” (CAM)–or, as its proponents like to call it these days, “integrative medicine” (IM)–to convince the public and physicians either to use it (or at least to remain a shruggie about it) is in essence an argumentum ad populum; i.e., an appeal to popularity. Specifically, CAM/IM apologists like to use the variant of argumentum ad populum known as the “bandwagon effect,” in which they try to persuade patients and physicians that they should get with the CAM/IM program because, in essence, everyone else is doing it and it’s sweeping the nation in much the same way New Coke did in the 1980s. (Admittedly, CAM/IM apologists are, unfortunately, much better at sales than Coca-Cola was.) Not coincidentally, this is one type of method of persuasion much favored by Madison Avenue when selling cars, clothing, music, movies, food, beer, and nearly every other product–like Coca-Cola. I say “not coincidentally” because what CAM proponents are doing, more than anything else, is selling a lifestyle, a brand, a belief system, and, of course, many, many products whose value reminds me, more than anything else, of the aforementioned New Coke. In using this appeal to popularity, CAM/IM proponents try to portray stodgy physicians (you know, like pretty much every one of us at this blog) who insist on plausibility, science, and evidence to support the use of drugs and treatments as hopelessly behind the times, dogmatic, out of touch, and in general no fun to be around at all, particularly at parties.
Arguably no single private organization has been more effective at promoting the infiltration of CAM/IM into medical academia (or, as I like to call it, quackademic medicine) than the Bravewell Collaborative. Co-founded by Christy Mack (yes, that Christy Mack), wife of John J. Mack, the former CEO and Chairman of the Board of Morgan Stanley who now serves as a Senior Advisor, and Penny George, the Bravewell Collaborative was formed when Mack and George hit up a bunch of wealthy, woo-friendly donors to form a charitable organization in 2002 to support the “advancement of integrative medicine.” One result has been the proliferation of quackademic departments in medical centers all across North America like so much kudzu fertilized by Bravewell Collaborative money topped off with a bit from the National Center for Complementary and Alternative Medicine (NCCAM) lovingly applied by true believers choking off science-based medicine. Known as the Consortium of Academic Health Centers for Integrative Medicine, this group of divisions, institutes, and departments of quackademic “integrative medicine” now numbers fifty and includes some of the most famous medical schools in the nation, such as, for example, Duke, Harvard, Stanford (as much as Wally Sampson hates to admit it), Yale (as much as Steve Novella hates to admit it), and my alma mater the University of Michigan (as much as I hate to admit it).
So successful has the Bravewell Collaborative been in inserting pseudoscientific and prescientific “healing” modalities right into the heart of medical academia that it decided to update a project that it called a “nationwide mapping project” whose purpose was: (1) to describe the patient populations and diseases most commonly treated with integrative medicine, (2) to define the core practices and models of integrative care, (3) to determine how integrative care is paid for, and (4) to identify the biggest factors driving successful implementation. Christy Mack wrote in 2010 that she hoped the project would be complete by, well, the end of 2010, but apparently there were some glitches along the way, because the project was just released to the Bravewell website as a report entitled Integrative Medicine in America: How Integrative Medicine Is Being Practiced in Clinical Centers Across the United States (executive summary here). As Steve so aptly put it, it’s a massive case of putting the integrative cart before the the science horse in that it is looking at what Bravewell has wrought in terms of promoting quackademic medicine without paying attention to whether any of this stuff actually works or whether “integrating” this woo into medicine does anything whatsoever to improve the quality of care at the medical centers that have jumped on the “integrative” bandwagon.
Before getting into the meat of the report, it’s worth noting that this is not the first survey of this kind. In fact, Bravewell was beaten to the punch by another major promoter of CAM/IM, the Samueli Institute. Together with the Health Forum, the Samueli Institute published a report five months ago entitled 2010 Complementary and Alternative Medicine Survey of Hospitals, which I reviewed in depth. The difference between the Bravewell report and the Samueli report is that the Samueli report focused way more on motivations (i.e., why hospitals decided to start CAM/IM programs), means (how they started up their CAM/IM programs), and finances (how much of do these programs cost and do they make any money?) than the Bravewell report does. The two reports do, however, show considerable overlap in trying to survey the specific CAM/IM modalities offered by the hospitals surveyed that reported having CAM/IM programs. Also, the Samueli report had more breadth and less depth in that the investigators sent out a surveys to nearly 6,000 hospitals, while Bravewell focused its attention on 29 hospitals, nine of which were Bravewell Consortium members, the rest of which were not. In other words, the differences between the Samueli survey and the Bravewell survey can be summarized as looking at a broad sampling of all hospitals (or at least trying to) and taking a focused look at true believers.
Like the Samueli report, the Bravewell report begins with the same distortions of language to which we’ve become accustomed from CAM/IM apologists:
The Bravewell Collaborative, a philanthropic organization that works to improve healthcare, defines integrative medicine as “an approach to care that puts the patient at the center and addresses the full range of physical, emotional, mental, social, spiritual, and environmental influences that affect a person’s health. Employing a personalized strategy that considers the patient’s unique conditions, needs, and circumstances, it uses the most appropriate interventions from an array of scientific disciplines to heal illness and disease and help people regain and maintain optimum health.”
Over the past two decades, there has been documented growth in the number of clinical centers providing integrative medicine, the number of medical schools teaching integrative strategies, the number of researchers studying integrative interventions, and the number of patients seeking integrative care. But whether integrative medicine was being offered in the same, similar, or disparate ways was unknown. In addition, while previous studies focused on the prevalence and use of complementary or alternative medicine (CAM) by patients1, 2 or by practitioners in hospital settings3 by enumerating the use of single CAM therapies, very little information had been collected regarding the actual practice of integrative medicine, which by definition treats the whole person.
That was from the executive summary, but the same sort of language pervades the introduction to the report proper, in which the authors go on and on about how “all factors that influence health, wellness, and disease are taken into consideration,” “care addresses the whole person, including body, mind, and spirit in the context of community,” and how care is “individualized” (in reality this is fake individualization) Note the canard of “holism,” in which (or so it is claimed) CAM/IM is supposedly capable of taking care of the “whole patient” in a way that scientific medicine is not. This is, of course, utter nonsense built on a false dichotomy that says that a practitioner has to embrace pseudoscience and prescientific beliefs, such as those behind homeopathy, “energy healing,” and the like, in order to take care of the “whole patient.” It’s been a successful ploy in that quite a few physicians have apparently bought into the lie inherent in the very name “integrative medicine.” If they hadn’t, there wouldn’t be so many CAM/IM programs that have sprung up over the last ten years, to be surveyed now.
The report is fairly easy to read, and it tells us all sorts of things, including that the most common model of CAM/IM care is consultative care, with less than half of the centers surveyed offering primary care (thank heaven for small favors). We also learn tidbits about which I care almost nothing at all, such as that 72% of CAM/IM centers surveyed use electronic medical records (yawn) and, oddly enough, 72% also offer self-care and wellness programs for their practitioners and staff (double yawn). One notes that my university offers self-care and wellness programs; so this isn’t particularly impressive to me. But I’ll take science-based care over woo any day, and “wellness” is a term that’s been so thoroughly co-opted by CAM/IM that I can’t help but grimace just a little whenever I read or hear it. Then, of course, a huge number of these programs say they do research, which makes me wonder what has become of the word, or, to repeat yet again one of my favorite bit: Research. You keep using that word. I do not think it means what you think it means. Either way, these little tidbits, while useful, were not particularly novel.
More interesting to me were the specific modalities offered in CAM/IM centers in their order of frequency:
The interventions prescribed most frequently across all conditions, in descending order, are:
- Food/Nutrition
- Supplements
- Yoga
- Meditation
- TCM/Acupuncture
- Massage
- Pharmaceuticals
Notice anything? I do. Look at what the number one most frequently prescribed treatment by these CAM/IM centers. It’s nutrition or food. When I saw that, I had two questions. First, when, exactly, did nutrition or food become somehow “alternative” or “integrative”? Did I miss something somewhere? Nutrition is a science-based field (or should be), and the use of nutrition to prevent and alleviate illness is (or should be) science-based medicine. Yet, here nutrition is magically “rebranded” as somehow being part of CAM or IM! That’s what we here at SBM mean when we describe the “bait and switch” of CAM/IM. Plausible, potentially science-based treatments are reborn as CAM/IM and then used as evidence that CAM works. They’re also the Trojan horse that CAM/IM proponents use to trick the guardians of SBM into bringing into fortress of academia. After these modalities have been accepted as “CAM,” out jumps the real woo, such as “energy healing,” to take over. It’s not so far-fetched, given that my alma mater has a program in Steinerian woo known as anthroposophic medicine. I can’t wait until its botany department starts offering courses in biodynamic farming.
Snark aside, note that, out of the top seven modalities reportedly used, only one of them is truly “alternative,” namely TCM/acupuncture, while one is borderline (supplements). For the rest, the same observation I have about nutrition applies. Massage? Since when is that “alternative,” badly interpreted studies of massage notwithstanding? Pharmaceuticals? You might as well see a real doctor! Yoga? Stripped of its woo, it’s just a form of exercise. Meditation? It’s just a variant of relaxation therapy. Supplements could be woo or non-woo, depending upon how they’re used, but when naturopaths, homeopaths, and chiropractors use them they’re almost always woo. And, of course, traditional Chinese medicine and acupuncture are nearly all woo.
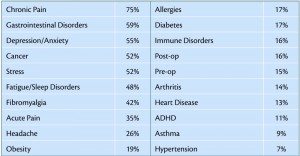
Particularly revealing is a section in which the survey asks for what diseases/conditions does IM produce “success.” That is, of course, a question so incredibly vague that, unless the patient dropped dead immediately upon contact with the therapy recommended, centers could claim some level of “success” with almost anything, and they do. No metrics for what constitutes “success” are described. Instead, the survey just takes the word of center directors for it. Basically, center directors were asked what conditions they considered to be conditions “among their top five most successfully treated conditions.” This generated the following, utterly useless table (click to enlarge):
Cancer was number five, with 52% of institutions claiming it to be in their top five conditions for which they have “success”? What do they mean? Certainly they don’t mean better survival, because I’d sure like to see that data if their claim is that they are successful treating cancer with CAM that way. I do have to admit that I chuckled grimly at this passage:
Cancer Treatment Centers of America (CTCA) at Midwestern Regional Medical Center in Zion, Illinois and The Integrative Medicine Center at MD Anderson Cancer Center in Houston, Texas. These two institutions only treat people with cancer. At CTCA, all treatment teams include a dietician, naturopathic doctor, mind-body therapist, chiropractor, and pain management clinician (including an acupuncturist) as well as a medical oncologist. MD Anderson’s integrative medicine center offers acupuncture, massage therapy, and mind-body-spirit practices such as meditation, guided imagery, yoga, tai chi, and music therapy. Therapies are provided to caregivers as well as patients.
Yes, Bravewell actually lumped together the Cancer Treatment Centers of America and M.D. Anderson Cancer Center. In woo, apparently, they are equals, which is far more an indictment of M.D. Anderson these days than it is praise for CTCA.
Next up, this survey touts the “personalized” care that these CAM/IM centers allegedly offer, with 93% of the centers surveyed claiming to offer “individualized care plans” for their patients. No, I’m not doubting that these centers come up with “personalized” care plans designed for each of their patient based on whatever “integration” of science-based medicine and pseudoscience takes their fancy. After all, when a Tarot card reader gives you a reading it’s personalized, as are psychic readings. What irritates me is that this CAM/IM apologists claim they are so much better at “individualizing” care than SBM, a claim that is pure nonsense. In breast cancer, I make individualized care plans for each of my patients as well. Nearly all of our breast cancer patients have multidisciplinary plans individualized to each of them involving multiple specialties (usually surgery, medical oncology, and radiation oncology, sometimes with genetic counseling as appropriate). In other words, Bravewell’s claim and that of its respondents are meaningless. The only thing that surprised me was that it wasn’t 100% of centers that claimed to offer “individualized care plans.” In fact, I’m downright amazed that two of the 29 didn’t claim to make them. It must have been the evil reductionistic “Western” scientists who forced them into offering “one-size-fits-all” treatments, just like us evil reductionistic “Western” doctors.
Finally, I found it interesting to look at where the rubber hits the road, so to speak, namely the practitioners whose salaries these centers are willing to pay (click to enlarge):
Not surprisingly, nearly all of these centers employ MDs. After all, we can bill and feed the referral machine. They also nearly all employ massage therapists and acupuncturists, both of which are what I like to view as gateway CAM, although massage can be justified easily without an appeal to pseudoscience or mysticism. What surprised me is that only 28% of them employ naturopaths, 21% employ osteopaths (maybe they’re all too busy being real doctors), and only 17% employ Ayurvedic practitioners, the last of which is no different than the number employing homeopaths. What didn’t surprise me is that some of these centers employ reflexologists and Rolfers, although I must admit that I have no idea what an “energy psychologist” is. Nor do I really want to know.
So now that we know the “what,” as in what services are offered, what are the outcomes? As it turns out, that is where this survey is unintentionally revealing. Basically, there are no medical outcomes reported. There are, however, lots of patient satisfaction surveys showing that patients like the woo being offered. Sadly, there is little or no discussion of actual efficacy and safety other than self-reported efficacy with no metrics to let us know whether or not the ideas of the center directors filling out the surveys of what constitutes efficacy had any connection with real measures of efficacy when they listed the conditions for which their centers have the most success.
All of this is very thin gruel upon which to base the conclusions of the report, such as:
The number of centers included in this study who expressed to the authors that their patient numbers were growing and/or their roles in their respective healthcare systems were expanding, suggests an increasing acceptance of integrative medicine by the American public and the medical professions.
Remember, there were only 29 centers surveyed. That’s a mighty big conclusion to rest on such a little study, particularly given that the survey used couldn’t measure acceptance of IM by the public anyway. One wonders why it took Bravewell so long to finish the study. Maybe it was the difficulty in figuring out a spin to put on it, although a blog from at least one institution surveyed in the study had no difficulty doing so.
The authors also conclude that IM really, really needs three things, the first of which is outcomes data. No kidding! On the other hand, as Steve points out, this is still putting the cart before the horse, as outcomes studies are usually indicated only after a treatment has been shown scientifically through a combination of basic science and translational research plus well-designed randomized clinical trials to be efficacious and safe. Until that evidence is there, there really aren’t any good reasons to study outcomes because there aren’t any scientifically valid reasons to be using these therapies to begin with. Oh, wait. The whole point of this survey is for Bravewell to congratulate itself on how much it’s managed to legitimize CAM/IM. Never mind. Be that as it may, if there aren’t any good reasons to be doing outcomes research, then there really aren’t any good reasons to be trying to identify best practices, which is the second recommendation of the report. After all, how does one identify best practices when there is so little scientific evidence to support the practices being examined? But don’t worry! Bravewell will definitely be doing another survey. It says it will. That is, after all, its third recommended next step.
None of this stops the authors from concluding:
One of the most striking, though perhaps predictable, conclusions of this study is that integrative medicine is, in fact, integrative. It integrates conventional care with non- conventional or non-Western therapies; ancient healing wisdom with modern science; and the whole person — mind, body, and spirit in the context of community.
The breathtaking inanity of Bravewell’s conclusion took my breath away, and all your bases are belong to us.
My conclusion is different. I conclude that “integrative medicine” integrates pseudoscience with science, quackery with medicine. Where it fails to do that, it rebrands science-based modalities like nutrition as somehow being “alternative” so that it can be listed as being CAM. On the other hand, one thing the writers of this report tell us in no uncertain terms is that, whatever you do, don’t call “integrative medicine” CAM. Just don’t do it, because Bravewell really, really hates it:
As was well articulated by Benjamin Kligler, MD, and Roberta Lee, MD, in the textbook Integrative Medicine: Principles for Practice, “Integrative medicine is not synonymous with CAM.” This survey has shown that integrative medicine centers embrace a group of core values that inform and radiate through their practice and interactions with their patients. Integrative care is, in practice, patient-centered care and is a fundamentally collaborative enterprise fostering cooperation between patients and practitioners, and among the practitioners themselves.
The problem, once again, is that it is not necessary to “integrate” pseudoscience with science-based medicine in order to practice collaborative patient-centered care. It’s really not, just as it’s not necessary to “integrate” pseudoscience into SBM in order to be “holistic” or to “take care of the whole patient.” Bravewell keeps selling that false dichotomy. I’m not buying, and neither is any member of the SBM team. Unforunately, though, a lot of doctors and medical centers are buying what Bravewell’s selling. They seem to want to view themselves as special flowers, but, no matter how much Bravewell, NCCAM, and other CAM/IM apologists try to convince patients and physicians otherwise, as our very own Harriet Hall has so frequently and eloquently said about naturopaths and CAM/IM practitioners, “What they do that is good is not special, and what they do that is special is not good.”
One of these days I’m going to have to try to come up with a statement that so succinctly and accurate describes CAM/IM, but I doubt that I will ever succeed.