Category: Cancer
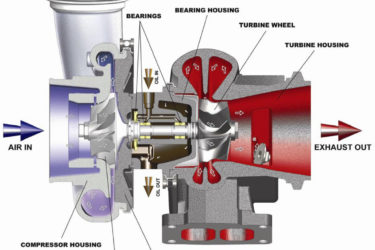
COVID-19 vaccine-caused “turbo cancer” nonsense just keeps getting more turbocharged
No matter how implausible it is or how weak the evidence for it is, the myth that COVID vaccines cause "turbo cancer" just won't die. Quite the contrary, alas. Antivaxxers are—dare I say?—turbocharging it with bad science.
There is no evidence that COVID-19 vaccines are causing cancers associated with “accelerated aging”
A recent presentation at AACR found a link between markers of accelerated aging and an increased risk of cancer. Then antivaxxers got a hold of it to blame COVID-19 vaccines not just for cancer, but for "accelerated aging" causing it.
Mark Sircus and “natural allopathic medicine”? Now I’ve heard everything from quacks
The term "allopathic medicine" was invented by homeopaths in the 19th century as a disparaging term for medicine. So to see a quack like Mark Sircus try to coopt it as "natural allopathic medicine" is quite something.

Best Hospital Eye Roll
Science: Figuring things out is better than making things up. A tee shirt I recently saw. Except… In a recent post Mayo Clinic Promotes Reiki, Steve seemed surprised that the Mayo was offering Reiki. I don’t know. Maybe he was channeling Louie. I know the Mayo is a top hospital, but I trained in Minneapolis at Hennepin County and we would have...

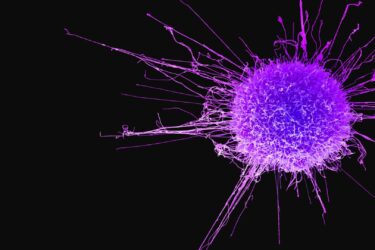
Fenbendazole is fast becoming the laetrile of the 2020s
Antivaxxers who "repurposed" deworming drugs like ivermectin and fenbendazole are peddling cancer "miracle cure" testimonials that remind me of laetrile and Stanislaw Burzynski. Truly, everything old is new again.

False balance in an NBC news story on whole body MRI scans
Over the weekend, NBC News aired a story on whole body MRI scans. Although it did include the usual cautions about false positives and the harm they cause, the caution was diluted by the story's focus a rare case of a woman who had a brain tumor detected. Overall, it was false balance that reminded me of vaccine/autism stories 20 years ago.

COVID-19 antivax quacks are now “repurposing” ivermectin for cancer
A year ago, I noticed that COVID-19 quacks were touting the "repurposing" of ivermectin to treat cancer. Now, familiar COVID-19 antivaxxers—cough, cough, FLCCC—have turbocharged this quackery.

A good journal breaks bad: AAP spreads misinformation about glyphosate
The latest report from the American Academy of Pediatrics is filled with misinformation and missing key articles that support the well-researched conclusion that there is no legitimate evidence of negative health effects of glyphosate.

He pushed hydroxychloroquine three years ago: Harvey Risch and false claim of “turbo cancers” caused by COVID-19 vaccines
Last week, I discussed Dr. William Makis' false claims of "turbo cancers" due to COVID-19 vaccines. Now it's hydroxychloroquine-promoting epidemiologist Harvey Risch's turn.
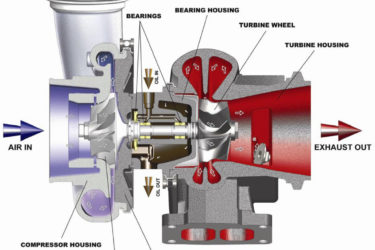
Dr. William Makis and “turbo cancer”: Falsely blaming COVID-19 vaccines for cancer
A prominent oncologist and cancer biologist, Wafik El-Deiry, recently amplified claims that COVID-19 vaccines cause "turbo cancer," wanting a "civil discourse about science and actual answers that are missing." Unfortunately, calls for "civil discourse" by an eminent oncologist about unfounded claims only lends undeserved credibility to them. So, once more into the fray...

