Category: Science and Medicine
The Residency Match is Broken
The National Resident Matching Program (Match), the program to align med school applicants with their preferred residency program, is broken and filled with disincentives. The fix might be easy.

More Data Supports Delayed Antibiotic Prescribing for Kids with respiratory infections
Overuse of antibiotics is a big problem. New data supports delaying that prescription for kids with respiratory infections.
What the heck happened to John Ioannidis?
John Ioannidis is one of the most published and influential scientists in the world, someone whose skewering of bad medical research we at SBM have frequently lauded over the years. Then the COVID-19 pandemic hit. Since then, Prof. Ioannidis has been publishing dubious studies that minimize the dangers of the coronavirus, shown up in the media to decry "lockdowns," and, most recently,...

Did Microwaves Harm US Employees at Its Embassy in Havana?
A recent review of unexplained symptoms in employees of the US Embassy in Havana pointed to microwaves. Was it mass psychogenic illness instead? Or something entirely different?
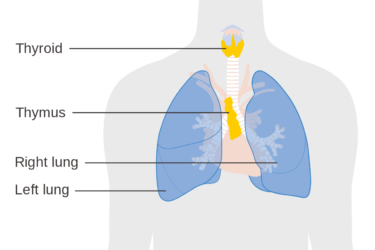
Who Is Amy B. Scher?
Amy B. Scher is a proponent of energy medicine and things like astrology and homeopathy. She claims to be a "science geek," but how could anyone who understands science think that tapping on the breastbone will fix the thymus?
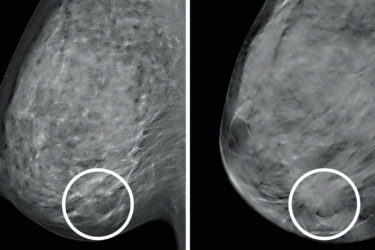
COVID-19 vaccination and screening mammography
Reports of enlarged lymph nodes under the arm after COVID-19 vaccination have led doctors to tweak mammography guidelines. Antivaxxers, unsurprisingly, have tried to weaponize this observation to spread fear and confusion about these vaccines.
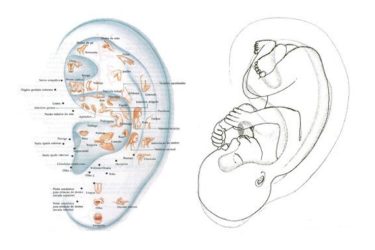
Ear Acupuncture for Procedural Pain in Neonates: More Randomized Controlled Nonsense
A recently published multicenter randomized and placebo controlled study attempted to answer the question of whether or not magnetic acupuncture beads stuck on premature baby ears reduced pain during a common screening exam. They don't. And they might have made things worse for these babies.
Countering Geert Vanden Bossche’s dubious viral open letter warning against mass COVID-19 vaccination
Geert Vanden Bossche is a scientist who published an open letter warning of global catastrophe due to deadly variants of COVID-19 selected for by mass vaccination. His argument sounds a lot like an argument Andrew Wakefield once made for MMR. There’s even grift likely involved!

The Brownstein protocol is not a proven treatment for COVID-19
Dr. David Brownstein is a "holistic" physician who practices in Dr. Gorski's neck of the woods. Unfortunately, he just wrote a book promoting an unproven protocol involving vitamins, nebulized hydrogen peroxide and iodine, and intravenous ozone to treat COVID-19. There is no evidence that his protocol works, other than a very poor quality case series.

Nonsense for Elephants: The Houston Zoo Promotes Kinesiology Tape
The Houston Zoo is promoting a bogus therapy as a treatment for aging elephants.

