Category: Science and Medicine
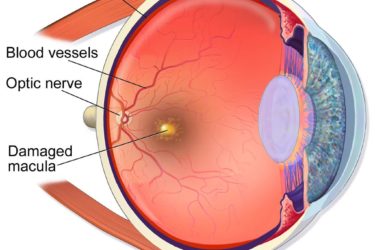
Macular Degeneration, Genes, and Grandma’s Vitamins: To test or not to test?
Is genetic testing necessary to optimize treatment for patients with a potentially blinding eye disease? The stakes are high and the answer depends on which of the two feuding, financially-conflicted groups you believe. In the end, the best evidence wins!

Coca’s Pulse Testing to Diagnose “Allergies”
In the 1950s, Dr. Arthur F. Coca invented an elaborate method to diagnose a new kind of "allergy" by testing the pulse rate. He thought "allergies" were the underlying cause of most disease. His method has never been tested, but there is every reason to think it is bogus.
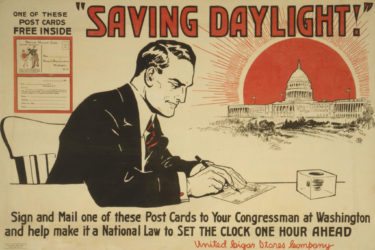
The adverse health effects of the lunacy that is Daylight Saving Time
Daylight Saving Time has been around for over 100 years. Why does it still persist when there's little or no evidence that it does what it was intended to do (save energy) and growing evidence of adverse health effects related to the twice a year time change? That's a good question. It's time to get rid of this antiquated practice.

A Miscellany of Medical Malarkey Episode 3: The Revengening
A setback for bogus marketing claims for fancy athletic tape. E-cigarettes aren't a good Christmans stocking stuffer for your kids. An update on the European measles outbreak. That's right, it's time for another miscellany of medical malarkey!

Are we all contaminated with chemical toxins?
Are we all being gradually poisoned by environmental toxins? And what is the evidence for detoxification kits and cleanses?

The 2018 Flu Epidemic: Hives and other Influenza Related Nonsense
While it isn't likely to be the flumaggedon, it is shaping up to be a really bad flu season. Unfortunately there is a lot of overzealous news coverage that I fear is causing more anxiety among parents than is warranted.

Rabies Claims the Life of a 6-Year-Old Florida Child: The Tragic Case of Ryker Roque
Rabies is an incredibly deadly infection, but one that is virtually 100% preventable. Unfortunately a Florida child recently paid the ultimate price when his parents failed to seek out appropriate medical care for a bat bite, and despite an experimental but flawed treatment protocol.
Georgian College’s Homeopathy Program: Magical Thinking Presented as Fact
Georgian College in Ontario, Canada is now offering a 3-year advanced diploma in the pseudoscience of homeopathy.

Legionnaires’ Disease: The Other Disneyland Outbreak
As 2017 came to a close, Disneyland again played a role in the outbreak of an infectious disease, this one much more deadly than measles.

Medical Marijuana: Where is the evidence?
Marijuana is widely touted as an effective medicine for an array of conditions. But what does the evidence actually tell us?

