NOTE: Today we offer a double feature on the treatment of cervicogenic headache: this post and Dr. Harriet Hall’s post, “When Headaches Are a Pain in the Neck: Spinal Manipulation vs. Mobilization for Cervicogenic Headache.” They complement each other, as well as Dr. Hall’s post from last week on the possible risk of stroke with neck manipulation.
A cervicogenic headache has been defined as a secondary headache (beginning in the suboccipital area) caused by nerve pain referred from a source in the upper cervical spine. According to the American Migraine Foundation, “To confirm the diagnosis of cervicogenic headache, the headache must be relieved by nerve blocks….Treatment includes nerve blocks, physical therapy, exercise, Botox injections, and medication. Physical therapy and an ongoing exercise regime often produce the best outcomes.”1
There are a number of published studies advocating use of upper cervical manipulation as a treatment for cervicogenic headache,2 often without adequate consideration of the danger of such treatment. While upper neck manipulation might sometimes be an effective treatment for a cervicogenic headache, care must be taken to avoid upper cervical manipulative techniques that may pose risk of stroke by damaging vertebral and internal carotid arteries.
Most headaches are of the tension-type variety, often originating in the myofascial structures of the head and neck. There are many other types of headache, some of which can be life-threatening or unbearably painful, none of which are neck related. Headache caused by a leaking brain aneurysm may portend possible rupture of a swollen blood vessel. A migraine or a cluster headache is less serious but can cause agonizing pain. Sudden appearance of neck pain with headache can be a symptom of spontaneous vertebral artery dissection, which can result in a full-blown stroke if aggravated by neck manipulation. When a headache is sudden, severe, or persistent, it is important to have a medical evaluation before concluding that you have a neck-related headache or before submitting to neck manipulation, especially upper cervical manipulation that involves rotation of the atlas on the axis.
Rotation in atlanto-axial joints
The greatest amount of rotation in the cervical spine occurs in the atlanto-axial (C1-2) joints in the upper cervical spine where vertebral arteries are most often injured. There are no interlocking joint surfaces and no intervertebral disc to limit rotation of the atlas on the axis, which is restrained primarily by ligaments. When rotation of the atlas exceeds 45 or 50 degrees, vertebral arteries threading through transverse processes on each side of the axis and atlas (to enter an opening in the base of the skull) are stretched, risking stroke caused by vertebral artery dissection or clot formation. Vertebral arteries that are diseased and have lost some of their elasticity are more susceptible to injury caused by neck manipulation.
The prevailing view of neck manipulation, based on scientific consensus, suggests that rotatory upper cervical manipulation is unsafe and that there is no known benefit that outweighs the risk of such treatment. Unless a specific upper cervical problem has been identified that can benefit from manipulation that does not involve more than 50 degrees of atlanto-axial rotation, there may be no justification for use of upper neck manipulation.
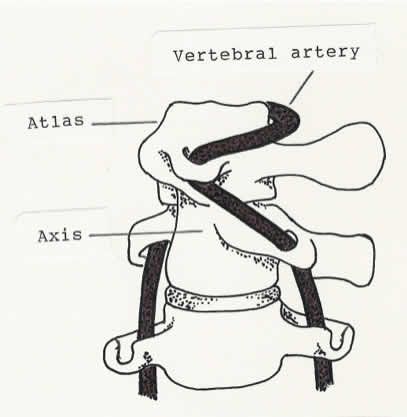
Forced rotation of the atlas on the axis past 45 or 50 degrees stretches the vertebral arteries.
Effects of cervical spine manipulation
Manipulative treatment such as massage, mobilization, or spinal manipulation applied to neck and upper back structures would probably be beneficial in relieving tightness and tension that triggers or contributes to a neck-related headache. Manipulating the cervical spine may have some neurophysiological effects in relieving head and neck pain as well as a mechanical effect in restoring mobility in cervical joints. There is reason to believe that spinal manipulation can temporarily relieve pain and muscle spasm by influencing pain (nociceptive) receptors and mechanoreceptors in muscles and joints. Noxious stimuli of any kind, such as acupuncture or a thrust-type manipulation, might relieve pain to some extent by stimulating the body’s production of endorphins (chemicals that interact with opiate receptors in the brain to reduce perception of pain). The popping sound of cavitation produced by spinal manipulation can have a powerful placebo effect, producing a psychological perception that the treatment is effective. Although such effects may provide temporary relief of pain, no permanent effect would occur unless the manipulation relieves muscle spasm or restores mobility in spinal joints.
The precautionary principle
There may be no positive proof that upper cervical manipulation can cause stroke by damaging the vertebrobasilar arteries3 (as is often said, “association is not causation”), but there are numerous case reports associating neck manipulation with stroke caused by injury to vertebrobasilar arteries, some occurring in young, healthy persons (most under the age of 45) immediately following a neck manipulation. Some of these injuries have been confirmed by imaging studies that show dissection of healthy arteries due to trauma.4,5 Considering the totality of evidence, it is logical to assume that reports associating neck manipulation with vertebral artery dissection in healthy persons strongly suggest a cause-and-effect relationship, providing reason enough to avoid upper neck manipulation.
The American Heart Association and the American Stroke Association offer this precautionary advice to practitioners who manipulate the cervical spine:
CD [cervical artery dissection] is an important cause of ischemic stroke in young and middle-aged patients. CD is most prevalent in the upper cervical spine and can involve the internal carotid artery or vertebral artery…. Although the incidence of CMT [cervical manipulative therapy]-associated CD in patients who have previously received CMT is not well established, and probably low, practitioners should strongly consider the possibility of CD as a presenting symptom, and patients should be informed of the statistical association between CD and CMT prior to undergoing manipulation of the cervical spine.6
Cavitation and rotatory manipulative techniques
Rotatory upper cervical manipulation is the technique most often associated with post-manipulative stroke. Extreme rotation of the top two cervical vertebrae ─ usually producing cavitation ─ is believed to be a cause of traumatic dissection of a vertebral artery. It is the extreme range of motion (uniquely upper cervical), not the cavitation, that injures a vertebral artery. While extreme rotation of the atlanto-axial joints should be avoided, with or without cavitation, cavitation is not always a bad thing.
The amount of rotation that takes place in high-velocity low-amplitude cervical spine manipulation depends upon the technique used. There are some techniques, such as lateral thrusting with a thumb contact, which can result in cavitation with little rotation. Cavitation in the cervical spine can also occur when pulling on the head at the end range of distraction (after taking up the slack) to stretch the spine with high-velocity low-amplitude traction while the patient is in a supine (face-up) position.
Note: Cavitation occurs when two contiguous joint surfaces are forcefully separated, creating a vacuum that pulls in gasses from synovial fluid, causing a pop. Joint surfaces are held together by a fluidic attraction that allows the joint surfaces to slide upon each other. When there is forceful movement of a joint, exceeding the normal range of movement (into the paraphysiologic space), the cavitation that occurs may temporarily increase range of motion or result in restoration of mobility if there is binding or fixation in the joint. The popping sound heard during manipulation can occur in normal joints and does not mean that a subluxation, an adhesion, or a misalignment was present. A joint that is freely movable is not subluxated or out of place and will always return to its anatomically dictated resting place after manipulation or cavitation. The alignment of freely movable joints cannot be changed.
Head rotation vs. neck rotation
When the head is actively rotated (a voluntary action), a little rotation takes place in all the cervical joints, including the atlanto-axial joints which rotate a little more than lower cervical joints but well within a safe range, allowing about 70 degrees of head rotation right and left. When the head is used to rotate the cervical spine with a long-lever technique, usually while the patient is in a supine position, a maximum amount of rotation occurs in the atlanto-axial joints, reaching ligamentous constraints where the vertebral arteries are most stressed. Extreme rotation in the atlanto-axial joints also occurs when a specific short-lever contact is used to rotate the atlas vertebra.
Needless to say, any manipulative technique that forces extreme rotation of the atlas on the axis should not be done.

Rotating the head to rotate the cervical spine forces an excessive amount of rotation in the atlanto-axial joints, as does a specific contact on the atlas in a rotatory manipulation.
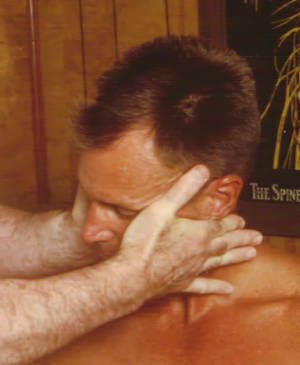
When I had occasion to use neck manipulation in my practice as a chiropractor, I usually sat the patient on a stool, using a four-finger contact on the side of the neck so that I could rotate the cervical spine as a whole. When the atlanto-axial joints are included in a full cervical contact for full cervical rotation, rotation in the atlanto-axial joints is not likely to be excessive. When the atlanto-axial joints are not included in a full-cervical rotation (below the C1 level), head rotation is considerably less, with little or no rotation of the atlas on the axis.
Cervical spine problems such as loss of mobility due to post-traumatic adhesions or entrapment of a cartilaginous fragment might benefit from full cervical rotation that does not force extreme rotation in the atlanto-axial joints, but such problems are questionable or not common and have not been adequately investigated.
Full cervical rotation does not force extreme rotation in the atlanto-axial joints.
Undetected contraindications for neck manipulation
There are many apparent contraindications for use of cervical spine manipulation, such as atlas instability in rheumatoid arthritis, nerve root impingement or disc herniation, osteoporosis, fever and other symptoms indicating disease or infection, use of blood thinners, carotid bruits, atherosclerosis, and so on. There are also some contraindications that may not be apparent in healthy, asymptomatic persons.
In addition to the danger of vertebral artery injury posed by excessive rotation of upper cervical vertebrae, undetected structural abnormalities in the cervical spine compound the danger of such treatment. A “retrolenticular vertebral artery ring,” for example, an abnormal bony bridge that encompasses the vertebral artery where it passes over the posterior arch of the atlas, can severely compress a vertebral artery during rotatory upper cervical manipulation.7 A Chiari malformation, a structural defect that allows a portion of the cerebellum to pass down through the foramen magnum and enter the spinal canal, can cause headache that begins on the back of the head and neck, resembling a cervicogenic headache or a muscle-contraction headache. Upper cervical manipulation in such a case would be dangerous.
Suffice it to say that no one should submit to neck manipulation as a treatment for headache without a careful history, a thorough exam, and a definitive diagnosis, and only with informed consent after first trying such physical treatment methods as massage and manual traction.
Note: The most common contraindication for upper cervical manipulation is a diagnosis of “subluxations” by some chiropractors who manipulate the neck of every patient they treat.
The bottom line
Because of the danger associated with upper cervical manipulation and the difficulty establishing a need for use of cervical spine manipulation, plus the difficulty finding a practitioner who uses cervical spine manipulation in a safe, conservative, and appropriate manner, I usually advise against submitting to neck manipulation when I am asked about such treatment. In most cases, time combined with use of such measures as exercise, postural ergonomics, sub-occipital massage, and manual axial (longitudinal) traction will be sufficient treatment for mechanical-type neck pain or a headache related to a neck problem ─ provided an orthopedic evaluation has ruled out complicating factors.
References
- Robert T. Cervicogenic Headache – The Basics. American Migraine Foundation. 2012. Return to text
- Dunning JR, Butts R, Mourad F, et al. Upper cervical and upper thoracic manipulation versus mobilization and exercise in patients with cervicogenic headache: a multi-center randomized clinical trail. BMC Musculoskelet Disord. 2016; 17:64. Return to text
- Church EW, Sieg EP, Zalatimo O, et al. Systematic review and meta-analysis of chiropractic care and cervical artery dissection: no evidence for causation. Cureus. 2016; 8(2):e498. Return to text
- Jatuzis D, Valaikiene J. Migraine-like presentation of vertebral artery dissection after cervical manipulative therapy. Perspectives in Medicine. 2012; 1(1-12):452-454. Return to text
- Jones J, Jones C, Nugent K. Vertebral artery dissection after a chiropractic neck manipulation. Proc (Bayl Univ Med Cent). 2015; 28(1):88-90. Return to text
- Biller J, Sacco RL, Albuquerque FC, et al. Cervical arterial dissections and association with cervical manipulative therapy. Stroke 2014; 45: 3155–74. Return to text
- Rao SR, Swamy G, Vasudha TK, Rao TR. Unusual foramen on the posterior arch of atlas. Journal of Science. 2015; 5(12):1165-1167. Return to text

Sam Homola is a retired chiropractor who has been expressing his views about the benefits of appropriate use of spinal manipulation (as opposed to use of such treatment based on chiropractic subluxation theory) since publication of his book Bonesetting, Chiropractic, and Cultism in 1963. He retired from private practice in 1998. His many posts for ScienceBasedMedicine.org are archived here.


