If you google “low testosterone” you’ll see lots of ads for testosterone replacement. Some are from pharmaceutical companies that sell testosterone, others from obvious snake-oil salesmen.
Both types of ads list vague sets of symptoms, encourage you to believe that they are pathologic, and want to sell you something to make you better. For example, the pharmaceutical company Solvay gives you a handy guide for speaking to your doctor, and a quiz to see if you have “low T”. The quiz asks some questions that may be useful, but also asks very general questions about your sense of well being, and includes this gem:
I don’t feel sick, I just don’t feel like myself anymore. Could I have Low T?
The ad then gives this advice:
Because Low T signs and symptoms may not be clear and apparent, they may seem to be a normal part of aging or assumed to be caused by other health conditions. But talk to your doctor if you have symptoms of Low T. And ask to get tested. All it takes is a simple blood test that can be done during a routine checkup. If you do have Low T, your doctor may recommend treatments that can help bring testosterone up to normal levels and keep them there.
If you have diabetes, you should ask your doctor for a Low T test. The Endocrine Society recommends that all men with type 2 diabetes have their testosterone levels checked. Patients who have been diagnosed with diabetes have an increased chance of also having Low T.
Let’s step back for a moment. What is being claimed is that low testosterone levels in males is a common cause of certain symptoms, and that testosterone replacement therapy can alleviate these symptoms. To evaluate this claim from the perspective of science-based medicine, we need to ask specific questions.
- Is there a plausible connection between testosterone levels and certain symptoms?
- What is a normal testosterone level?
- Are there specific symptoms that correlate with lower levels?
- Does replacement therapy correct these symptoms?
Testosterone is an important hormone in males, and the effects of complete testosterone deprivation are easily observed. Castration has different effects on males depending on whether it is done before puberty or after. Given the effect of total androgen (testosterone) deprivation, it is plausible that partial deficiency may lead to physiologic problems.
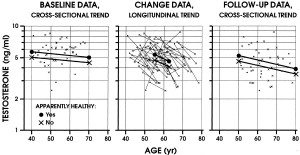
Defining normal testosterone levels is problematic though. Most studies show a decline in testosterone levels with age. What is “normal” at 30 is not “normal” at 70. Does this decline correlate with symptoms?
The answer isn’t clear. Studies have shown that low testosterone levels are associated with different symptoms at different ages. In older men with sexual dysfunction, low testosterone levels were associated with severe erectile dysfunction and decreased frequency of intercourse. In younger men, low testosterone levels were associated with a decrease in nocturnal erections and reduced libido. In the middle of the studied age range, there were no significant associations between testosterone levels and sexual symptoms. What this may tell us is that in older men, low levels of testosterone likely contribute to severe symptoms of sexual dysfunction.
The answer to question 2 is that normal testosterone levels vary with age, the type of test used, and the time of day the blood is drawn. Testosterone decreases with age, and this decrease correlates with certain symptoms. Because of these and other data, the recommendation of the Endocrine Society (the most comprehensive and authoritative source) is to restrict the diagnosis of testosterone deficiency to men who have consistent symptoms and an unequivocally low testosterone level.
Question 3 has a difficult answer. As we’ve seen, in certain age groups, certain sexual symptoms correlate well with low T levels. There are some weak associations between less specific symptoms and testosterone deficiency (symptoms such as fatigue, loss of vigor, depressed mood, decreased physical performance). Most of these less specific symptoms can be caused by a variety of problems or by none at all.
So, the data support a connection between certain symptoms and low testosterone levels. Can testosterone replacement therapy (TRT) improve these symptoms?
The evidence is mixed. There seems to be good evidence that testosterone replacement improves libido, but has little effect on erectile dysfunction (especially in younger patients). There is a paucity of placebo-controlled studies of TRT, but non-placebo-controlled trials show some improvements in energy and sense of well-being.
Several medical conditions are correlated with low T. Obesity fairly strongly correlated with low testosterone levels, but there are no consistent data that show an improvement in obesity with TRT.
In sum, testosterone deficiency is a real problem that may affect a small but significant number of men. The symptoms most consistent with low T are sexual problems, especially with age. Replacement therapy seems to help with these symptoms in some men. The ads for testosterone replacement therapy are, in my opinion, very problematic, nearing the point of deception. They seem to link all manner of vague and common symptoms to low T, and imply that the use of their product is likely to fix these problems. These ads explicitly instruct patients to ask for testing that may not actually be required. They shift the focus from a careful, methodical analysis of a difficult problem to frank disease mongering, encouraging the pathologizing of what may be normal symptoms, and offering up a costly therapy that may be no better than placebo, but with additional risk.
References
Corona, G., Mannucci, E., Ricca, V., Lotti, F., Boddi, V., Bandini, E., Balercia, G., Forti, G., & Maggi, M. (2009). The age-related decline of testosterone is associated with different specific symptoms and signs in patients with sexual dysfunction International Journal of Andrology, 32 (6), 720-728 DOI: 10.1111/j.1365-2605.2009.00952.x
Spetz, A., Palmefors, L., Skobe, R., Str??mstedt, M., Fredriksson, M., Theodorsson, E., & Hammar, M. (2007). Testosterone correlated to symptoms of partial androgen deficiency in aging men (PADAM) in an elderly Swedish population Menopause, PAP DOI: 10.1097/gme.0b013e318057786b
Allan, C., Forbes, E., Strauss, B., & McLachlan, R. (2008). Testosterone therapy increases sexual desire in ageing men with low–normal testosterone levels and symptoms of androgen deficiency International Journal of Impotence Research, 20 (4), 396-401 DOI: 10.1038/ijir.2008.22
Reyes-Vallejo, L., Lazarou, S., & Morgentaler, A. (2007). Subjective Sexual Response to Testosterone Replacement Therapy Based on Initial Serum Levels of Total Testosterone The Journal of Sexual Medicine, 4 (6), 1757-1762 DOI: 10.1111/j.1743-6109.2006.00381.x
Bhasin S, Cunningham GR, Hayes FJ, Matsumoto AM, Snyder PJ, Swerdloff RS, Montori VM, & Task Force, Endocrine Society (2010). Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. The Journal of clinical endocrinology and metabolism, 95 (6), 2536-59 PMID: 20525905
Araujo, A., Esche, G., Kupelian, V., O’Donnell, A., Travison, T., Williams, R., Clark, R., & McKinlay, J. (2007). Prevalence of Symptomatic Androgen Deficiency in Men Journal of Clinical Endocrinology & Metabolism, 92 (11), 4241-4247 DOI: 10.1210/jc.2007-1245