There are few home-runs in medicine. Most of our choices have some sort of trade-off – drugs have side effects, interventions have risks, and many treatments have marginal benefits. Sometimes, however, medical science hits one out of the park and develops a treatment that is safe, effective, cost effective, and convenient. Any dispassionate view of the evidence can only lead to one conclusion, leading to the absence of any legitimate scientific or medical debate.
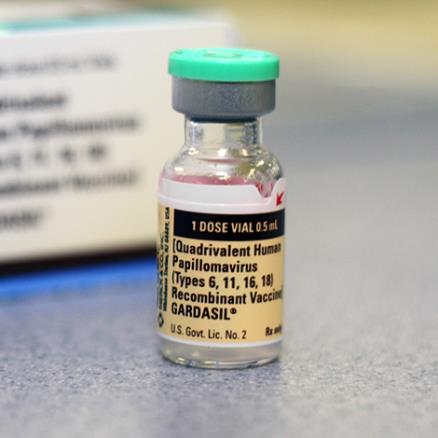
I think the human papilloma virus (HPV) vaccine falls into this category. We have learned that many oral and genital cancers are caused by a sexually transmitted virus, HPV. Getting vaccinated against several strains of this virus prior to becoming sexually active effectively protects against infection by the virus, and dramatically reduces the risk of these cancers. Think about it – we can prevent cancer with a vaccine. This is a no-brainer.
HPV DNA was detected in 90.6% of cervical, 91.1% of anal, 75.0% of vaginal, 70.1% of oropharyngeal, 68.8% of vulvar, 63.3% of penile, 32.0% of oral cavity, and 20.9% of laryngeal cancers, as well as in 98.8% of cervical cancer in situ (CCIS). A vaccine targeting HPV 16/18 potentially prevents the majority of invasive cervical (66.2%), anal (79.4%), oropharyngeal (60.2%), and vaginal (55.1%) cancers, as well as many penile (47.9%), vulvar (48.6%) cancers: 24 858 cases annually. The 9-valent vaccine also targeting HPV 31/33/45/52/58 may prevent an additional 4.2% to 18.3% of cancers: 3944 cases annually.
The new 9-valent vaccine covers more strains. The study suggests that there are over 28,000 cases of cancer each year in the US that could be prevented by this vaccine.
Yet, a 2010 survey found that only 11% of 13-17 year olds had received the complete series of three injections, while 25% had received at least one dose. Further, for those who do get vaccinated almost half are starting later than they should or taking longer than they should to complete the series. These figures are improving, however. The latest figures from the CDC for year 2013 show a sharp increase, with 37.6% of girls completing the series, and 13.9% of boys.
The HPV vaccine is also not just for girls. Boys benefit as well, and this benefit is increasing as oral-genital behavior seems to be increasing in the younger population, leading to greater HPV rates associated with oral cancers. Male HPV vaccinations are cost effective, although it is still more cost effective to increase the compliance rate among young females.
A number of studies have looked at barriers to HPV vaccine uptake. A systematic review found:
Twenty-one barriers to vaccination were identified. Cost was the most frequently reported barrier, followed by feelings that vaccination was unnecessary, and concerns regarding vaccine safety and side effects. Facilitators included perceived benefit of vaccination, health care provider recommendations, and social norms. Few studies specifically sought to isolate the views of adolescents, though not being sexually active was the most commonly reported barrier among this group.
This is a situation in which education is likely to be an effective measure. Preventive measures in medicine are most effective when they cover the target population, which in this case is all pre-teens. The HPV vaccine is most effective when the series is completed prior to becoming sexually active. Not being sexually active is therefore not a reason to avoid the vaccine.
Pediatricians also need to be educated. Lack of recommendation by their doctor was given as the reason for not vaccinating in 13% of girls and 22% of boys.
The safety of these vaccines has been widely studied and monitored. The HPV vaccines are extremely safe, with only minor side effects. Of course, anti-vaccine propaganda will cite the Vaccine Adverse Event Reporting System (VAERS) data which shows reports of 1,671 serious adverse events following HPV vaccines by 2013 (after 67 million doses). The problem with citing this data, however, is that it is not controlled. This is a voluntary reporting system with no filters. It is, in essence, a massive exercise in correlation, without any way to assess causation.
Fortunately the data has also been looked at in a more scientific way, comparing the rates of adverse outcomes in those who receive the HPV vaccine vs those who did not. Such comparisons show that there are no serious adverse events that are more likely in the HPV vaccinated than unvaccinated population.
Antivaxxers are doing their best to spread fear and misinformation. It is easy to scare parents about side effects, so they have an advantage in their misinformation campaign. Most notorious are reports of deaths following HPV doses. With 67 million doses given, there are going to be random associations with other outcomes, including death. There have been 97 reports of deaths following HPV vaccine as of March of 2014. The CDC investigated every case. In 47 of the cases they had sufficient information to make a determination, and in every one they found that the death was completely unrelated to the vaccine.
Conclusion
The HPV vaccines are safe, effective, and cost effective. There is sufficient evidence to confidently conclude that they are an effective public health campaign, with the potential of preventing thousands of cases of a very serious disease – cancer. There are some practical barriers to full implementation, but they can be and are being overcome, mostly through education.
The only real barrier to full implementation is ideology – distrust of science, medicine, government, or corporations, irrational worship of the concept of “natural”, belief in magical medical nonsense, or the misguided belief that preventive measures promotes immoral behavior.
