Legal to sell, yes. But ethical to sell?
Complementary and alternative medicine (CAM) is no longer fringe, and anything but the mom-and-pop image that manufacturers carefully craft. CAM is big business, and most Americans today take some sort of supplement. The impetus for my blogging (and tilting at CAM windmills) emerged from years spent working in a pharmacy with a heavy reliance on CAM sales. If it was unorthodox, this store probably sold it. Conventional drug products (the ones I was familiar with) were hidden off in a corner, and the store was otherwise crowded with herbal remedies, homeopathy, and different forms of detox kits and candida cleanses. All of this was unlike anything I’d ever seen or heard about in pharmacy school – so I started researching.
I looked at CAM from a scientific evidence perspective, the one I was taught in pharmacy school, using the same approach I’d take when assessing a new drug. Did the evidence support the claims made about these products, or not? The answers, as you might expect, were often the same. There was little or no credible evidence to demonstrate CAM had any meaningful benefits. I started blogging my own reviews as a way of documenting my own research, while offering some information to anyone on the Interwebs who might be searching for evidence.
Over time my blogging focus expanded, as I asked myself the inevitable questions: How could implausible products with no scientific backing even be approved for sale at all? I discovered the regulatory double-standard allowed for anything considered a dietary supplement (or in Canada, a “natural health product“) and the history and politics that have made CAM the “Wild West” of health care, with a marketplace that prioritizes a manufacturer’s right to sell over a consumer’s right to purchase a product that is safe and effective. Given the retail marketplace that’s been established by regulators like the FDA and Health Canada, I’ve turned my focus on to health professionals, who have an ethical responsibility to put patient interests above that of commercial interests. From a professional practice and medical ethics perspective, I have argued that health professionals that sell or promote CAM are on ethically shaky ground, and compromise the credibility of the profession.
Despite the lack of evidence that CAM (in general) offers any health benefits at all, it’s been remarkable to watch its popularity grow, to the point where even large pharmacy chains now sell aisles of products that are implausible and often highly questionable. Generally meeting these changes with a collective shrug, the pharmacy profession has even tried to lower its own ethical standards. While I do get the occasional encouragement from some of my peers, most just say “it’s business” or “the customer wants it, and these are legal products.” My argument today is CAM fails even this lower ethical bar.
Last fall I joined Professor Chris MacDonald of Ryerson University to give a talk as part of Ryerson’s business ethics speaker series. The topic was complementary and alternative medicine (CAM), and the ethics of selling these products. (You can watch that presentation here.) I’m pleased to announce that we have now published a peer-reviewed paper on the same topic in the journal Bioethics, “Alternative Medicine and the Ethics of Commerce.” Here’s the abstract:
Is it ethical to market complementary and alternative medicines? Complementary and alternative medicines (CAM) are medical products and services outside the mainstream of medical practice. But they are not just medicines (or supposed medicines) offered and provided for the prevention and treatment of illness. They are also products and services – things offered for sale in the marketplace. Most discussion of the ethics of CAM has focused on bioethical issues – issues having to do with therapeutic value, and the relationship between patients and those purveyors of CAM. This article aims instead to consider CAM from the perspective of commercial ethics. That is, we consider the ethics not of prescribing or administering CAM (activities most closely associated with health professionals) but the ethics of selling CAM.
The paper is currently open access – so go grab a copy, read it, and come back to discuss.
An ethical framework for CAM
In our new paper, MacDonald and I pose (and answer) three primary questions:
- What is the case for selling CAM? We consider the value of a diversity of choice and the benefits of a free marketplace.
- What are the general ethics of commercial transactions? We outline an ethical framework that can guide an evaluation of CAM.
- What does this ethical framework say about the commercial sale of CAM?
- Is CAM merchantable – does it fail to function?
- Does the sale of CAM involve deception?
- Does the sale of CAM harm third parties?
What exactly is CAM?
The question of what exactly is CAM is one that’s been discussed again and again on this blog. This is a fair question and one which we considered carefully in drafting our paper. The boundaries of CAM are always in flux as science progresses. Rather than get bogged down with a specific definition, we used a general approach:
Further, it should be acknowledged that the borders of the entire category, CAM, are fuzzy. While it includes treatments that have not yet been tested, or lack sufficient evidence to be accepted as medicine, CAM also includes treatments that have been extensively tested, demonstrated to be ineffective from a scientific perspective, and consequently rejected from conventional medicine. Consequently what’s considered CAM may shift over time…Our solution is to offer a broad framework that can be applied to any healthcare product or service – indeed, to any product or service at all. While our topic is CAM, when it comes to evaluating a particular product or service, very little hangs on whether that product or service is ‘really and truly’ an example of CAM, or on whether it is an example of complementary, as opposed to alternative, medicine. Second, the examples used below generally involve treatment modalities – such as homeopathy and acupuncture – that are typically and uncontroversially considered central examples of CAM.
The argument for CAM
The argument for CAM is one which I hear regularly from the pharmacy profession. There are two important principles that provide legitimate support for the commercial sale of CAM:
Respect for individual (consumer) autonomy: It is morally good to respect the choices that people make in marketplaces, and it is generally better to avoid paternalism. More choices in the “marketplace” for health mean more unique needs can be met. If consumers prefer CAM, then it is good that these products be available to purchase.
The respect for a competitive marketplace: Markets tend to work effectively when there are lots of choices from many vendors. Competition keeps prices low and keeps firms competitive. Restricting CAM restricts markets. By definition these products are alternatives to medicine and in particular, often considered to be legitimate substitutes for products and services considered “conventional” medicine.
An ethical framework for considering CAM
In developing an ethical framework, we strived to make the model as simple as possible. Our approach was to outline a small set of norms that we feel are assumed and effectively endorsed by those that participate in commercial transactions. We note the assumption that market transactions are ethically legitimate. We agree with this presumption, but also highlight that their ethical legitimacy is conditional, as it’s based on assumptions that participants are well informed and that beneficial outcomes are expected by the participants. We propose the following:
Participants in commerce should endeavor to:
- Offer a product that works – a product that is, in the language of commercial law, ‘merchantable.’
- Only sell products to people who understand their fundamental characteristics, and who are reasonably capable of understanding (either on their own or with suitable professional help) whether that product will meet their needs. This implies a general demand for honesty on the part of sellers, and a refusal to profit from the ignorance of consumers.
- Take reasonable steps to ensure that third parties (those who do not consent to participate in a particular market exchange) are not harmed.
It should be fairly clear to anyone that looks at the actions of the FTC in the area of CAM that when this framework is grossly violated, regulators can and will act, prosecuting CAM vendors when products do not work or when sellers are not honest about the characteristics of their product. Green coffee bean, which I’ve blogged about extensively, is an example of rank fraud in CAM sales and marketing.
Considering the ethics of selling CAM
Does CAM work?
Any regular reader to this blog will know that there is little evidence to demonstrate that CAM offers any meaningful, beneficial medicinal effects. In fact, some CAM, such as homeopathy, is an elaborate placebo system, where most remedies contain no medicine at all – they are completely inert.
Some of the arguments for CAM efficacy are actually arguments against conventional medicine, a false dilemma suggesting that since some medical products lack efficacy, CAM must work. However, while some “conventional” medicine products may lack robust evidence of efficacy, explanations for how they might work do not rely on magical (or wishful) thinking. And while conventional medicine is far from perfect, its scientific foundation means that products can be tested for efficacy in ways that help us understand if effects are real, and if they cause harm. And we agree that this framework can also be applied to “conventional” medicinal products that may lack efficacy.
Another argument for CAM borders on post-modernism, where conventional medicine is felt to take a far too narrow view of what constitutes “evidence” of efficacy. We reject this argument:
We acknowledge that it is at least possible that some CAM modalities are not well suited to such study. However, we resist the implication that such difficulties do much to cast doubt upon the strong scientific consensus that says that most CAM treatments simply do not work. First, note that while treatment of particular patients may be highly individualized, this is true for patients of mainstream or conventional medicine too. And while treatment – whether alternative or conventional – may be highly individualized, it is inevitably based on broad clinical generalizations which ought to be susceptible to rigorous testing. Second, note that at least some clinicians who favour at least some forms of CAM believe that those forms are indeed capable of being fairly tested by means of randomized controlled trials. It should be noted noted [sic] that if CAM treatments are not rigorously tested, then ineffective CAM treatments will never be identified. But many such trials have been conducted, and on the whole the results have been dismal. Third, where there are legitimate reasons for thinking that the kind of rigour represented by the classical randomized controlled trial is out of place for testing a particular form of CAM, there remains a need for promoters of CAM to find some rigorous method – for example, something beyond intuition, tradition, and anecdote, something that goes some distance to overcoming the well-documented flaws to which personal observation is subject – for establishing efficacy. Where such non-RCT evidence is available, it is worthy of some measure of respect. But to the best of our knowledge, such credible, non-RCT evidence of effectiveness is not available for most forms of CAM.
Of course, some might object that we have too narrow a notion of what it means for a health product to ‘work.’ A particular treatment, even if it has no demonstrable physiological effect, may for example have religious, spiritual, or cultural significance. If a product satisfies the needs of some religious rite, for example, then it should count as a product that ‘works’ in the relevant sense. In some cases, such significance might constitute ethical justification for selling a product even in the absence of proof of biological efficacy. But there are strict limits to such justification. In particular, if that is the sense in which the product is expected to ‘work,’ then that must be an understanding that is shared between buyer and seller and acknowledged in communications between them. Note also that in some cases, people may perceive in CAM cultural (or other) values that simply are not there. As MacDonald, (2002) argues with regard to women’s health, for example, the popularity of CAM may be the result, in part, of a values-based rejection of modern society’s intense ‘medicalization’ of nearly everything related to women’s health. But as MacDonald argues, in some cases the use of CAM products may in fact constitute ‘the substitution of one commercialized expert understanding of women’s health and bodies for another.’12 A complex homeopathic regime offered by an ‘expert’ naturopath, perhaps at some considerable cost, may not in fact prove any less alienating than more mainstream options. Another example: homeopathy is often touted as an alternative to ‘Western’ medicine despite the fact it was invented in a western nation, namely Germany. Anyone who thinks of homeopathy as somehow part of an exotic Eastern tradition, and who values it for that reason, is not getting what they’re paying for.
But what about the vendor who truly does believe that their particular CAM does work? We do not doubt the sincerity of many providers of CAM. However, we argue that this is not an acceptable excuse:
However, it is not plausible to excuse vendors for selling a product that does not work simply because they have either not taken the time and effort to investigate whether their product works, or turned a blind eye to the evidence that is available to them. There is, after all, such a thing as willful ignorance. While the credulous seller of (for example) homeopathy may not be guilty of knowingly selling something that does not work, he or she is guilty of having culpably low epistemic standards. Such a person does not sell knowingly, but he or she does arguably sell recklessly.
We argue that vendors should be taking reasonable steps to determine if their product “works” based on the claims they are making about their product. Given the specific (and often measurable) claims made about CAM effectiveness for different conditions and circumstances, we believe it is the responsibility of the vendor to evaluate the best evidence available, taking care to ensure the statements they are making are backed by supporting evidence. If a product or service cannot be reasonably expected to deliver as promised, then ethically, a vendor should stop selling that product in the marketplace.
Does the sale of CAM involve deception, or does it profit based on the ignorance of consumers?
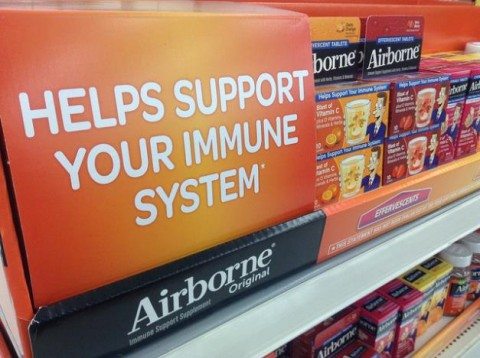
Many consumers lack access to good information on the effectiveness of CAM remedies. Look at the marketing of Airborne above. Airborne has no demonstrable efficacy, and even after the manufacturer settled false advertising charges, it is still sold openly (albeit without explicit claims of efficacy). Homeopathy is another excellent example. Homeopathic “remedies” are so dilute that most products don’t contain a single molecule of any medicinal ingredient – or even the ingredient that is listed on the label. Moreover, if homeopathy was to actually work, it would overturn much of what we know about biology, chemistry and physics. A similar argument can be made for acupuncture. Meridians and acupuncture points have never been shown to actually exist. There is no chi, and acupuncture is a theatrical placebo. Acupuncture doesn’t work. Yet few consumers know these facts, and regulators do not require manufacturers to provide them.
Does CAM harm third parties?
One need only look to the use of endangered species in CAM remedies to illustrate the point that CAM can definitely harm those outside commercial transactions – it is driving some species extinct. Homeopathy provides another illustrative example. Homeopaths and naturopaths sell “nosodes” which are marketed as alternative to real vaccines. These “nosodes” are inert sugar pills. Those that use “nosodes” in place of vaccines compromise public health by reducing population vaccination levels, putting some members of the population (e.g., the immunocompromised) at risk of infection. Finally there are multiple examples of children harmed by parental use of CAM in place of actual medicine.
Is selling CAM ethical?
Even setting aside medical ethics, we argue that the sale of CAM is unethical. CAM can violate all three ethical principles of commercial transactions. In order for commercial transactions to be ethical, they must involve products that work. They must be advertised and promoted fairly and honestly. Finally, these transactions must not harm innocent third parties. Much of CAM fails on one or more of these measures.
Photo via flickr user Mike Mozart under a CC licence.
