The cover of Georgetown Medicine Spring/Summer 2015 issue. This image will drive Mark Crislip crazy, as it features yet another acupuncturist not using gloves while sticking needles into people. Dr. Gorski loves watching Dr. Crislip’s reactions to such photos.
We frequently discuss a disturbing phenomenon known as quackademic medicine. Basically, quackademic medicine is a phenomenon that has taken hold over the last two decades in medical academia in which once ostensibly science-based medical schools and academic medical centers embrace quackery. This embrace was once called “complementary and alternative medicine” (CAM) but among quackademics the preferred term is now “integrative medicine.” Of course, when looked at objectively, integrative medicine is far more a brand than a specialty. Specifically, it’s a combination of rebranding some science-based modalities, such as nutrition and exercise, as somehow being “alternative” or “integrative” with the integration of outright quackery, such as reiki and “energy healing,” acupuncture, and naturopathy, into conventional medicine. As my good bud and fellow Science-Based Medicine (SBM) blogger Mark Crislip put it, mixing cow pie with apple pie does not make the cow pie better, but we seem to be “integrating” the cow pie of quackery with the apple pie of science-based medicine thinking that somehow it will improve the smell, taste, and texture of the cow pie.
I remember how, when I first discovered how prevalent outright pseudoscience and quackery had become in medical academia (which was before I became one of the founding SBM bloggers), I was in denial. I couldn’t believe it. Then I tracked this phenomenon with something I called the Academic Woo Aggregator. It turned out to be a hopeless endeavor because, as I soon discovered, the phenomenon was so pervasive that it was really hard to keep the Aggregator up to date. Since then, I’ve generally only focused on particularly egregious examples, naming names when institutions like my alma mater embrace anthroposophic medicine; “respectable” journals publish “integrative medicine” guidelines for breast cancer patients; cancer organizations include “integrative oncology” in their professional meetings; NCI-designated comprehensive cancer centers promote reiki to pediatric cancer patients or offer high dose unproven vitamin C treatment to patients; or respected academic institutions embrace traditional Chinese medicine (TCM) and the quackery that is function medicine. You get the idea. It’s depressing just how far medical academia has fallen in terms of being “open-minded” to the point of brains falling out when it comes to medical pseudoscience.
From time to time, I’ve briefly thought about reviving the academic woo aggregator, but quickly and inevitably ended up giving up trying to come up with lists of the worst of the worst. There are just too many now, and keeping such an aggregator up to date would be too much work, as I discovered when I wrote my Nature Reviews Cancer article on integrative oncology last year. However, I do believe in featuring specific institutions when something comes up that draws my attention to them, and this just happened last week with Georgetown University. Basically, a reader at my not-so-super-secret other blog pointed out the Spring/Summer issue of Georgetown Medicine Magazine. It’s an issue devoted to integrative medicine at Georgetown and it is horrifying to anyone who believes that medicine should be science-based. Not surprisingly, it was a Georgetown alumnus who was so shocked when he received this issue in the mail that his embarrassment knew no bounds for having come from that institution. Worse, from the tone of the articles in this issue, Georgetown is proud of its integrative medicine program, to the point where it is touting it as a strength and featuring it on the cover of its magazine. Just look at its cover, which features a picture of a woman preparing to get an acupuncture needle stuck somewhere, along with the title of the issue, “Caring for the whole person with integrative medicine”. Yes, it’s the “holistic” trope that drives me crazy because you don’t have to embrace quackery to be a holistic physician.
Integrating pseudoscience into the medical curriculum
Longtime readers might remember that I’ve discussed Georgetown before because it was a “pioneer” (if you can call it that) in “integrating” quackery into the medical school curriculum. Having received a grant from the then-National Center for Complementary and Alternative Medicine (NCCAM), renamed in December the National Center for Complementary and Integrative Health (NCCIH), to integrate CAM into its core curriculum, Georgetown proceeded to do just that. Here’s an example, a blast from the past if you will, quoted from a 2003 Georgetown brochure (retrieved again, thanks to Archive.org):
“One of the reasons CAM is usually offered as an elective is that there’s just no time or room in U.S. medical schools to fit in one more massive subject,” says Michael Lumpkin, Ph.D., professor and chair of the department of physiology and biophysics at Georgetown. “When the course is an elective, a self-selected group – maybe 10 or 20 students in a class of 180 medical students – will take it,” Lumpkin says. “What we’ve tried at Georgetown is rather than create all new courses, we take relevant CAM issues and modalities and weave them seamlessly into existing courses.
The “seamless” weaving of CAM into existing classes includes, for instance, a presentation by an acupuncturist on the “anatomy of acupuncture” in the gross anatomy course for first-year students. The same lecturer explores acupuncture’s application in pain relief in the neuroscience course…
Haramati and Lumpkin say Georgetown’s program is distinct from CAM initiatives in other medical schools in two ways: The school is integrating CAM education into existing course work across all four years of each student’s medical education, and the initiative includes a mind-body class to help students use techniques to manage their own health and improve self-care.
Teaching acupuncture points during gross anatomy? You can hear the cringing of advocates of science-based medicine everywhere, given that acupuncture points do not exist except in the minds of acupuncturists, as there are no anatomic correlates to them. So what’s been going on since then? Jane Varner Malhotra tells us in Georgetown’s Evolving Study in Complementary and Alternative Therapies. Here’s what happened after Georgetown got the $1.7 million grant in 2001:
Haramati recalls some uncertainty around the method for how to actually make it happen. “We were walking a path where the advocates were saying, ‘You’ve got to do more,’ while skeptics were saying, ‘What are you doing teaching nonsense?’” he recalls. “And we were going down the path saying, ‘We’re going to look at this objectively.’”
Objectively. You keep using that word. I do not think it means what you think it means. An objective analysis of acupuncture would not support “integrating” the teaching of acupuncture points into gross anatomy and neurology class. Once again, acupuncture points do not exist except in the minds of acupuncturists, and even then I’m not so sure.
The article also does the requisite rebranding of natural products pharmacology as somehow being “CAM,” when it’s not. There’s a pharmacologist named Hakima Amri, featured smiling with her arms crossed in one of those stereotypical poses that magazines like this like to use in their photos bragging how she had realized that in her research she was “using top-notch technology in the biomedical sciences,” such as PCR, animal studies, cell culture, all “to study a plant extract” (Ginkgo biloba). None of this, of course, is CAM.
And Georgetown credulously teaches homeopathy, The One Quackery to Rule Them All:
Amri enjoys seeing students open their minds to new concepts. Learning disciplines like homeopathy may require students to radically disregard their previous understandings about receptors and responses in toxicology, for example. “I tell students that for the next few hours, put aside all they have learned in biochemistry, pharmacology and cell biology—empty their brains—because homeopathy is a completely different concept. Then I see big eyes on their faces!” laughs Amri.
Yes, Georgetown is telling its medical students, forget all that boring old reductionist “Western” science you’ve learned all these years. Open your mind to the sympathetic magic that is homeopathy. Never mind that it has no basis in science and its precepts violate multiple well-established laws of physics and chemistry. Personally, I don’t mind a medical school teaching homeopathy, but only so that doctors know what it is and how utterly pseudoscientific it is. (Most doctors still think it’s just herbal medicine.) However, clearly that’s not what Georgetown is doing. How a pharmacologist can teach homeopathy as anything but as an example of the most abject pseudoscience is beyond me, but that’s what Amri sure appears to be doing, her claim that “we are teaching them [medical students] how to evaluate the science of the therapy, critically analyze it and learn about these medical systems in the most open-minded way” notwithstanding. She seems to be all about the open-mindedness and not so much about critical thinking, similar to the entire Georgetown CAM curriculum.
And its faculty are proud of Georgetown’s role in promoting quackademic medicine:
Since the early years of complementary medicine research and education at Georgetown, the university has held a critical place on the national scene. Hosting multiple cross-disciplinary dialogues, Georgetown has convened chiropractors and conventional doctors, acupuncturists and anesthesiologists to advance the science-based study of integrative medicine.
And:
Over the past 15 years, the way CAM has been taught at Georgetown has evolved, but the goals have remained constant: to train students to objectively and rigorously assess the safety and efficacy of various modalities, and explain the mechanistic basis for therapies like acupuncture, massage, herbs and supplements, and mind-body interactions.
If Georgetown teaches homeopathy as anything other than an example of pseudoscience and integrates acupuncture into its gross anatomy, physiology, and neuroscience curricula, it’s doing nothing of the sort. Let’s take a look at the sort of research into the “mechanisms” of acupuncture that Georgetown is so proud of.
Torturing rats in the name of acupuncture pseudoscience
In another article in the issue “Where’s the Evidence? Probing the Underlying Mechanisms of Acupuncture“, a recently-published study by a member of the Georgetown faculty is featured as a great example of how Georgetown is doing what it claims with respect to evidence for CAM. First, though, we learn that a nurse anesthetist and licensed acupuncturist Ladan Eshkevari, Ph.D., teaches sessions on acupuncture in the second year physiology class. There, she also teaches TCM medicine pulse analysis. Now, certainly every physician should know how to assess a pulse, but that’s not what’s going on here. What’s going on here is the teaching of an ancient, prescientific method of assessing pulses:
The professor of nursing, pharmacology and physiology shows the students three different pulse points on each hand used in TCM to diagnose the health of specific anatomical organs. The best practitioners employ over 70 different ways to describe the subtle variations in the human pulse, she explains, as the students touch their own wrists. Is the pulse skipping, surging, floating, faint? Determining the right descriptor can be a challenge, Eshkevari adds, but the richness of the options reveals the complexity and nuance of the ancient practice.
“In traditional Chinese medicine, organs are viewed by their energy function, not their anatomic function,” Eshkevari continues, showing visual maps of the body linking heart and small intestine, lung and large intestine. She explains that with holistic medicine, everything is connected, versus the more typical American, allopathic medical practice of dividing the body into compartments and developing specialties.
One notes that these “subtle variations” are in general not reproducibly detected from practitioner to practitioner and have little or no evidence to show that they reliably link to specific organs. The same is true of tongue diagnosis in TCM, in which different organs are mapped to different parts of the tongue, such that examining the tongue can lead to diagnoses of abnormalities of specific organs. It’s utter nonsense, of course, no more than a TCM version of reflexology, which does the same thing, only mapping organs and body parts to the soles of the feet and palms of the hand. Yet at Georgetown, TCM reflexology is taught as fact.
Let’s take a look at the study that is featured in a large chunk of this article:
Eshkevari turned to rats to help her find answers. Using a successful stress model developed by a fellow researcher at Georgetown, she exposed three of four groups of animals to one hour a day in a container with a layer of ice water on the bottom. After two weeks, the rats measured high stress hormone levels that would not come down to baseline. They had chronic stress.
Won’t someone think of the poor lab rats?
Ladan Eshkevari, Ph.D. in her laboratory. Truly, I need to have a picture of myself taken with such a kick-ass “I’m a scientist, ma-an!” pose in my laboratory. Sadly, I don’t have as much stuff on my lab bench and shelves, which mean I must not be as much of a true scientist as Eshkevari, but I could add Erlenmeyer flasks with colored solutions in the background for an even more “science-y” feel.
Note that in the accompanying photo, Eshkevari is shown in the same pose as everyone else, arms crossed, with the exception that the smile is missing and she’s wearing a lab coat standing in front of an impressive lab bench full of chemicals and instruments, the better to paint the picture of her in the mind of the reader as a Very Serious Scientist. At least the photographer restrained himself from filling up Erlenmyer flasks and beakers with multicolored solutions, which is the ultimate photographic cliché in stories of this sort. I also note that the Georgetown magazine story seems to be part of a PR offensive to promote this study, complete with a press release and breathlessly credulous descriptions of the story in the media with titles like “Rats help scientists get closer to solving the mystery of acupuncture.”
In any case, these stories follow a template. Basically, every study is represented as “the strongest evidence yet” that the “ancient Chinese therapy” (which, remember, really isn’t particularly ancient, at least not the way it’s currently practiced) is more than placebo and that a definitive mechanism has been found through which this magic works. In this particular case, notice how it’s claimed that acupuncture does the same thing as actual drugs used to treat stress and pain. So it must be real! In every case, if you go and look at the actual study, there’s way less there then is being sold. This case is no different, as I saw when I looked up the actual study, “Effects of Acupuncture, RU-486 on the Hypothalamic-Pituitary-Adrenal Axis in Chronically Stressed Adult Male Rats.”
The first thing I noticed about this study is that it uses a common bait-and-switch favored by acupuncturists, in which they do something called “electroacupuncture” (EA). Basically, EA is acupuncture plus electricity. Acupuncture needles are stuck in the subject at the various acupuncture points and hooked up to an electrical source, after which as weak electrical current is applied. Whenever I see this bait-and-switch, the first question that comes to my mind is: Those ancient Chinese must have been really brilliant to have discovered how to use electricity thousands of years ago! Obviously, attaching electrodes to acupuncture needles is a modern twist on acupuncture, which is why all the language about this “ancient Chinese therapy” is so grating. Indeed, the Georgetown Medicine article claims that acupuncture dates back 4,000 years, which is further than I’ve ever heard anyone claim. One wonders how Bronze Age craftsmen made such exquisitely thin needles. In any case, EA is not ancient at all, nor is it acupuncture. Really, it’s just transcutaneous electrical nerve stimulation (TENS) grafted onto acupuncture to produce a mutant Frankenstein’s monster of a therapy that has little to do with either. When I see a study like this, my usual reaction is a big, “Meh.” This doesn’t demonstrate that acupuncture works. If it demonstrates anything at all (which is questionable) it demonstrates that passing an electrical current through the skin has physiological effects.
Does this study demonstrate anything? Let’s take a look. There were two experiments. In the first, the investigators divided the rats into four groups. Three of these groups were stressed and divided into groups receiving electroacupuncture, sham acupuncture (delivered to an area that is not an acupuncture point), and a third group that did not receive acupuncture. A fourth group of animals served as controls; they received no acupuncture and were not subjected to the stress stimulus. The stressed animals were placed in a 1 cm deep ice water bath for one hour daily for 14 days, after which they were returned to their cages. On day 5 experimental treatments were begun, which consisted of acupuncture or sham acupuncture 30 minutes after the cold exposure. (Poor rats.) The acupuncture point used was St36, which in humans is on the leg, one finger width lateral from the anterior boarder of the tibia and four finger breadths below the patella. Its action and effects are said to include:
- Tonify deficient Qi a/or Blood.
- Tonify Wei Qi and Qi overall – low immunity, chronic illness, poor digestion, general weakness, particularly with moxibustion, very important acupuncture point for building and maintaining overall health.
- All issues involving the Stomach a/or the Spleen – abdominal/epigastric pain, borborygmus, bloating, nausea, vomiting, GERD, hiccups, diarrhea, constipation, etc.
- Clear disorders along the course of the channel – breast problems, lower leg pain.
- Earth as the mother of Metal – will support Lung function in cases of asthma, wheezing, dyspnea.
- Psychological/Emotional disorders – PMS, depression, nervousness, insomnia.
Whatever.
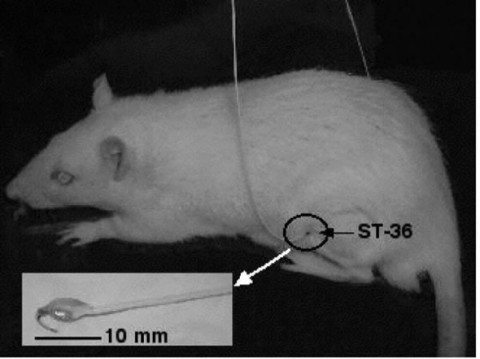
Here it is, the acupuncture point St36 that everyone’s been talking about. Of course, a rat’s leg bends differently than humans; so I have a hard time seeing how this was mapped from humans.
The nonacupuncture point used as “sham” for sham electroacupunture (sham-EA) was on the back 2 cm lateral to the tail region. The needles were then attached to an electroacupuncture machine via electrodes and were stimulated for 20 minutes at a frequency of 10 Hz with 2 mA output. Ten of the 14 rats in both the sham-EA and the EA St36 groups continued to receive EA for the 14 days that they were exposed to the cold stress. However, after 10 days, 4 of the animals in each of the sham-EA and EA St36 groups stopped receiving the EA treatments, whereas exposure to cold stress was continued for the remaining 4 days, to determine whether the effects of the sham-EA and/or EA St36 were long lasting.
In a second experiment, rats were assigned to five groups: Group 1 (no treatment and no RU-486); group 2 (no treatment but started RU-486 at day 10); group 3 (daily cold stress and start RU-486 at day 10); group 4 (sham EA + RU-486 + cold stress); and group 5 (EA + RU-486 + cold stress). The mice were also tested in other stress tests, including the forced swim tests and open field test. In this case, RU-486 was not used for its properties that allow it to work as a “morning after” pill, but rather for its ability to block the glucocorticoid receptor, the hypothesis being that however EA “works” it does so through glucocorticoid (steroids), a hormone signaling axis known as the hypothalamic pituitary adrenal (HPA) axis, which mediates stress.
The first thing I noticed was that levels of ACTH (which stimulates cortisol production) and cortisol were not impressively different, particularly ACTH (Figure 1; the paper is open-access if you want to check for yourself). Indeed, the differences in ACTH are so modest that my reaction was a yawn. Cortisol showed more difference, but a most unimpressive difference between EA and sham-EA. In the second experiment, there were a whole lot of graphs that didn’t show much difference in anything. The best that the authors could say is that RU-486 didn’t affect EA or sham-EA, but that ACTH didn’t go up in the St36 group. It was reported that stress behaviors were less in stressed EA St36 animals, but looking at the graphs sure didn’t impress me. Basically, the authors conclude that application of EA St36 after initiation of chronic stress prevents the stress-induced increases in the hormones evaluated, adding that “this action may be specific to EA St36 vs the sham points used, as sham-EA does not prevent the rise in stress hormones as effectively.” One notes that the sham treatment did have an effect. The effect, if real, was very modest.
There were a lot of other problems, as well. For instance, it’s important to note that the controls chosen were not exactly…robust. There was no group of rats in which the needle was inserted but no current was applied, nor was there another non-St36 control. (Choosing one “incorrect” acupuncture point to apply “sham” acupuncture to might be (barely) justifiable in human trials because of how hard it is to get enough subjects, but in an animal trial there is no excuse. How do the investigators know they weren’t just lucky picking their control? Also, there is no mention of blinding. Zero. Zilch. Since humans were evaluating behavior in the second experiment, it was critical that the observer doing the evaluations of how the rats reacted to the swim test and open field test were blinded to the experimental group from which the rats came. This appears not to have done. Finally, as noted on PubPeer, a website for post-publication peer review, Figures 6B and 6C appear to be the same figure even though they are said to represent different experiments.
The kindest description of the conclusions of this study is that it shows that running electrical current through the leg, as opposed to running current through the skin of the back, might decrease stress by decreasing the effect of stress hormones. It does not show that acupuncture works. A more realistic description of these results is that they don’t show much of anything that is scientifically interesting. One even wonders if, for instance, there is a simpler explanation, namely that having a needle stuck in the leg and having current run through it hurts less than having a needle stuck in the back and having current run through it. There’s no way of knowing because we can’t ask the rat. Alternatively, I also note that St36 is rather close to the sciatic nerve, whereas the acupuncture point on the flank used for the sham-EA control is nowhere near a major nerve.
Basically, this is a poorly done study with small numbers that doesn’t even test acupuncture but electricity. If this is the “evidence” for acupuncture that Georgetown touts, it’s thin gruel indeed. Yet it was published in a respectable journal, Endocrinology. Clearly, Endocrinology needs a better class of peer reviewers, as peer review utterly failed in this case.
Unfortunately, this doesn’t stop Eshkevari from wanting to “translate” these results to the clinic:
The next stage for her research will be human trials—an expensive and complicated endeavor but one she is determined to explore.
“This is where I’m now stuck,” she explains. “I’m trying to get grant funding to do research on humans to see if these discoveries translate.”
Eshkevari remains hopeful that, with rising interest from both the public and scientific communities, this next critical step will find support.
To me, it would be unethical to carry out a human study based on such poor quality and equivocal preclinical evidence. Unfortunately, it would not surprise me if Eshkevari succeeds in getting funding to do one. Such is the pernicious effect of quackademic medicine on clinical trial ethics. Eshkevari argues that doctors didn’t know how inhalational anesthesia worked when it was first discovered but used it anyway, the implication being that we should not be uncomfortable using acupuncture because we don’t yet understand its mechanism of action. Does anyone see the flaw in that reasoning? It’s obvious. That inhalational anesthesia worked was indisputable. In contrast, there is no good evidence that acupuncture works better than placebo. This brings up another problematic attitude in the mindset of quackademics:
“Western, allopathic physicians and nurse practitioners want to be able to point to the evidence, and see the research published in peer-reviewed journals,” says Eshkevari. “This helps us comfortably recommend complementary medicine to our patients. Finding the evidence—I think that’s the biggest step.”
In other words, rather than finding out if acupuncture works, quackademics like Eshkevari assume that it does work and then go chasing mechanisms. It is, as Harriet Hall so aptly described it, Tooth Fairy science.
Faith healing in the chemotherapy suite
I frequently call homeopathy The One Quackery To Rule Them All. However, there is a definite challenger for that title, which can be looked at a different way as well; i.e., as Saruman trying to usurp Sauron on his dark throne. I’m referring, of course, to “energy medicine.” Whatever form energy medicine takes, it’s based on prescientific vitalism of a variety that posits the existence of a “life energy” that can be manipulated or infused into the patient for healing effect.
The two most common forms of energy medicine in quackademia are therapeutic touch and reiki. Therapeutic touch (TT) is a misnomer in that it doesn’t usually involve actual touching (which negates the potential pleasure of a good massage or back rub), but rather involves the placing of hands close to the body. It rests on the concept that there is a human “energy field” that TT practitioners can manipulate to make patients feel better. It’s a concept so ludicrous that even an 11 year old girl could show that TT practitioners cannot detect a human energy field any better than random chance alone would allow them to guess. Unfortunately, TT is almost ubiquitous in nursing programs and hospitals. The second is reiki. The main differences between the two are that (1) reiki involves more elaborate hand gestures and (2) reiki posits the existence of an external source of life energy (the “universal source”) into which the reiki practitioner can tap to direct the healing energy into the patient. Reiki is, in essence, faith healing based on Eastern mysticism rather than the Christian religion. Unfortunately, reiki is commonly offered in many medical centers, academic or community, and even in NCI-designated comprehensive cancer centers.
Including Georgetown’s, apparently, as shown in the Georgetown Medicine article, “A Patient’s Experience With Energy Healing“:
For a long time Denise von Hengst had a secret she kept from friends and physicians alike. As she was undergoing treatment at Georgetown Lombardi Comprehensive Cancer Center for a particularly aggressive type of breast cancer—triple positive, HER2 positive—she was also regularly receiving Reiki, an ancient form of Japanese healing, to mitigate the debilitating anxiety and fear that accompanied her cancer diagnosis.
“At first I told no one about the Reiki,” says von Hengst. “Fear of the ‘woo-woo’ factor. People might think I’m nuts.”
No, a patient like Denise von Hengst is not “nuts,” although, it must be noted, she discovered reiki before coming to Georgetown for her cancer and ultimately became a reiki master. However, the Georgetown Lombardi Comprehensive Cancer Center is unethical and irresponsible for offering, in essence, magic to its patients as therapy. If I were not a physician and didn’t know anything about reiki, if an NCI-designated comprehensive cancer center offered it I’d think it must be evidence-based. That’s how most patients perceive it. The failure is on Georgetown’s part for offering reiki as though it were anything more than prescientific vitalistic superstition and claiming that it has a scientific basis, not on the part of patients like von Hengst, who trust that doctors are offering science-based therapy. In this case, Georgetown reinforced von Hengst’s initial attraction to reiki by giving it the appearance of scientific validity.
To her credit, the author of this article does acknowledge the “skepticism” that doctors have about reiki:
However, skepticism remains, not only in the general population, but also within the medical field. Recently, several clinical trials have emerged attempting to prove, or disprove, the effectiveness of Reiki. Many of these studies have been criticized for the trial. design, number of participants and reporting mechanisms. Results of the trials are often inconclusive.
Note that Bayes theorem tells us that “inconclusive” results plus an incredibly implausible mechanism = negative trial. So, yes, these are are negative trials. None of that matters, though, because the article quickly shifts gears to use anecdotal evidence and appeals to authority and popularity:
Yet as the anecdotal proof mounts and Reiki’s popularity increases, prestigious medical centers around the country are taking note and offering the treatment to patients at their facilities. Reiki can be found at hospitals and medical centers such as Boston Children’s Hospital, Dana Farber Cancer Institute, Stanford Health Care, Memorial Sloan Kettering Cancer Center, Duke University Health System and Cleveland Clinic, to name a few. Many academic medical centers such as Georgetown incorporate complementary therapies into their teaching curricula.
And all of these hospitals have failed to uphold a science-based standard of care. Sadly, they are not alone. Far from it. Worse, they are training the next generation of doctors to embrace pseudoscience.
Integrating quackery: The future of medicine?
Perhaps the most disturbing part of this issue of Georgetown Medicine is an article entitled “Putting Integrative Medicine Into Practice.” Basically, it’s a profile of medical students and recent Georgetown graduates doing exactly what the title says. It also includes a profile of an acupuncturist named Rebecca Berkson, who works at a Georgetown-affiliated facility, the Kaplan Center for Integrative Medicine in McLean, Virginia. In the name of Georgetown, she provides “acupuncture, its associated techniques including moxabustion and cupping, and Chinese herbal medicine.” Cupping, remember, claims to remove unnamed “toxins” from the skin thusly:
It’s a treatment almost as ridiculous as TT, and it’s being offered at Georgetown as though it has validity.
There’s also a medical student from the Howard University class of 2015 named Brian Nwannunu. He graduated from Georgetown’s CAM master’s degree program. Now he’s a believer:
My plan is to go into orthopedic surgery. For my patients experiencing back pain, I will work with CAM practitioners such as acupuncturists and chiropractors in addition to offering allopathic medicine. After my own experience with a low-back injury during a workout, I went to a chiropractor for a few weeks and felt tremendously better.
And:
I took a holistic medicine and pediatrics course last summer, and people were speaking quietly about homeopathy. I find it interesting to see how many practitioners approach complementary medicine like it’s voodoo. But that is changing. As holistic medicine becomes more prevalent, more students are talking about it, and we’re being taught to be aware and accepting.
Pardon me while I pound my head against the nearest wall.
Then there’s Megan Blunda, who graduated from Georgetown in 2011 and is now a family practice doctor:
I worked with Steve Schwartz, M.D., in the Introduction to Osteopathic Manipulative Medicine elective at Georgetown. I have carried the skills I learned in that course to my career as a family physician in Seattle. Over the last year and a half, I have been training in the art of cranial osteopathy. Through work with a mentor and an intensive 40-hour course, I have learned the skills to perform basic treatments for patients with headaches, neck pain and back pain. The ability to actually make a patient’s pain better, instead of masking it with medications, is incredibly fulfilling.
That’s right. Here’s a Georgetown graduate who is practicing cranial osteopathy, also known as craniosacral therapy, which is what Mark Crislip likes to call a “SCAM of infinite jest“—and for very good reason. Worse, Blunda is proud of this, claiming that her integration of such treatments into her practice allows her to “provide higher quality and more personalized care.”
Conclusion: The future of medicine is quacky
Unless checked, this is the future of medicine. Indeed, this entire issue makes the case that integrating quackery into medicine, bringing the Hogwarts School of Witchcraft and Wizardry to life as medical schools, is the future of medicine. Unfortunately, strive as we might against it, I’m having a hard time disagreeing. Proponents of “integrating” witchcraft like reiki, acupuncture, homeopathy, and craniosacral therapy into medicine will say that it’s not at all like Hogwarts. They have a point, but not in the way they think. In marked contrast to the magic gaining traction in the current world of quackademic medicine, in J.K. Rowling’s fictional world of Hogwarts, magic could be studied rigorously and actually worked. Would that this Brave New World of integrative medicine could say the same thing.
2 comments on PubPeer
