
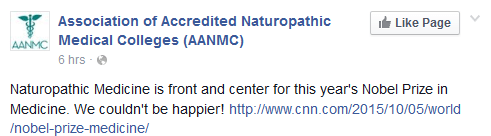
The 2015 Nobel Prize in Physiology or Medicine was awarded Monday, acknowledging the developers behind two drugs used to treat parasite infections. In a shared award, William C. Campbell and Satoshi Ōmura won for the discovery of avermectin, and Youyou Tu won for the discovery of artemisinin. Given both of these products are derived from natural substances, and “natural” remedies are used in different alternative medicine philosophies, it is perhaps not surprising that advocates claimed that this somehow validates practices like Traditional Chinese Medicine (TCM) and naturopathy. The Association of Accredited Naturopathic Medical Colleges (AANMC) made the following announcement on their Facebook page:
Which if you follow the link to the CNN story and actually read it, is surprising. It doesn’t mention naturopathy at all. In fact, when you look closer at the two drugs and their development, this year’s Nobel Prize is actually an excellent case study that illustrates the inherent limitations and weaknesses in alternative medicine systems like naturopathy, herbalism or TCM, while reinforcing just what science-based medicine is capable of delivering.
The problem with “natural” remedies
We’ve turned to the substances around us to serve as medicine well before we even knew what medicine was. Herbs and plant substances were probably our species’ first drugs. Philosophically, some believe that herbs and plant substances exist (or were placed) on earth expressly to cure our illnesses, and the challenge is simply to match the right plant to the right disease (sometimes based on ludicrous principles). The reality is much more interesting. Plants are amazing chemical factories that produce substances which may or may not have biological effects in humans. And Mother Nature is utterly indifferent to our health and survival: Some of the most toxic substances on earth are natural substances. As the study and use of herbs and plants moved from belief- and anecdote-based herbalism toward more the more rigorous and scientific study of their therapeutic use, the science specialization called pharmacognosy emerged. Unlike herbalism, naturopathy, or Traditional Chinese Medicine, pharmacognosy is the scientific study of drugs of natural origins (see some examples of pharmacognosy on SBM in these discussions of the Angel’s trumpet mushroom and the Thunder God vine). Research focuses on identifying biologically-active chemicals, isolating them, and turning them into useful medicines. It’s pharmacognosy that’s changed pharmacies from stocking jars of raw herbs into dispensing pharmaceutical dosage forms like tablets, creams, and injections, with predictable effects and standardized quality. In medicine, we don’t use raw substances that contain ingredients like opium, digitalis, and belladonna. Very few natural products are in active medical use, because in most cases the natural substances have some negative or inferior properties – such as unpredictable amounts of active ingredients. Once the active chemical substance has been identified and isolated, chemists go to work to synthesize it, standardize it, and even improve upon it. And that’s exactly what happened with the two drug products the Nobel committee cited.
Malaria, killer for millennia
Malaria has killed millions over the thousands of years we have coexisted with it. We’re lucky today as we may think of it only when we travel. I live in Canada and was amazed to learn that malaria was killing Canadians where I live in the 1800s and wasn’t actually eliminated from Canada until 1950. Worldwide, malaria remains a formidable killer. The World Health Organization estimates that 3.3 billion people in 97 countries are at risk of malaria – over half of the world’s population – and it continues to kill almost 500,000 people per year. Malaria is caused by the parasite Plasmodium, which is carried by mosquitoes and transmitted by bites.
Artemisinin (and related drugs) are without question the most effective malaria treatments ever created. Its discovery came just as existing treatments for malaria were beginning to fail due to drug resistance: Chinese soldiers were dying in Vietnam from drug-resistant infections. While the Cultural Revolution was putting many scientists and intellectuals into labour camps, Mao directed the army to identify new treatments. Hundreds of scientists were apparently recruited, and the early research focused on screening thousands and thousands of chemicals for efficacy. But it also looked to traditional medicine for clues, searching for fever “cures”. Dr. Tu found a reference to quinghao (artemisinin) in old texts that made references to fevers. She is credited by the Nobel committee as the first to investigate the substance scientifically and showed that aretemisinin was effective against the malaria parasite. Amazingly, she’s noted to have referred back to old texts as guides:
Also, after rereading a manuscript by Ge Hong, a fourth-century healer, prescribing qinghao steeped in cold water for fever, she realized that boiling, the typical extraction method, was destroying the active ingredient. She switched to ether, and qinghao became the first plant extract 100 percent effective at killing malaria in mice.
A host of factors stalled further research and development over the following years, but slowly published evidence began to emerge, and in 1982 The Lancet published an article from Chinese researchers. (Orac’s post on the Nobel Prize has more.) Alone, artemisinin isn’t effective as a treatment – it is eliminated too quickly from the body. What finally turned artemisinin into a useful drug and brought this treatment to patients was in fact Big Pharma:
A Swiss company, Novartis, finally broke the logjam. It bought a new Chinese patent on a mix of artemether, an artemisinin derivative, and lumefantrine, another Chinese drug, and took out Western patents, planning to sell it under the name Riamet at high prices to tourists and militaries; in 2001, it agreed to sell it nearly at cost to the W.H.O. under the name Coartem. The money to buy the drug on a large scale became available with the creation of the Global Fund to Fight AIDS, Tuberculosis and Malaria in 2002 and the Bush administration’s introduction of the President’s Malaria Initiative in 2005. Now, about 150 million doses of several combinations are bought for poor countries each year.
In part through the discovery of artemisinin, it’s estimated that malaria infections have been cut by 40% over the past few years, and mortality from malaria has been reduced by about 50%. There are likely few other drug discoveries that have produced (or will produce) this magnitude and extent of benefit.
The misery of roundworm
For many of us, the only worm infection we may ever recall is a case of pinworms as a child. But parasite worm infections cause catastrophic harms worldwide. The worms called Onchocerca volvulus are carried and transmitted by blackflies, causing the tropical disease river blindness which leads to skin and eye inflammation and sometimes blindness. Lymphatic filariasis or elephantiasis is an infection caused by Filariodidea roundworms and spread by mosquitos to hundreds of millions around the world. Infections cause abnormal swelling of different body parts, leading to pain, swelling and social stigma.
The discovery of avermectin also illustrates how applied science can improve upon natural substances. Satoshi Omura, a Japanese microbiologist, was a researcher of natural products who focused on identifying new Streptomyces bacteria, which produced substances known to have antibacterial properties. In 1974 some of the most promising Streptomyces bacterial cultures were acquired by (yep, Big Pharma again) Merck in the USA.
William C. Campbell, an American expert in parasite biology at Merck, worked with Omura’s cultures and demonstrated that one isolate was effective against parasite infections. That product was isolated, purified, and named avermectin. This product was subsequently chemically modified to be less toxic to humans and more effective against parasites. This new drug was named ivermectin. It is so effective that it only needs to be taken once or twice a year to clear Filariodidea infections. It should be noted that significant credit for the benefit of ivermectin needs to be given to Merck’s CEO at the time, Roy Vagelos, who brought the drug to market and then made it freely available to countries that needed it. As of 2012, over 200 million people have received the drug.
Beyond herbalism: Science-based practice
So what do these discoveries have to do with naturopathy? Nothing, really. Naturopathy is an alternative medicine philosophy based on pre-scientific principles. The central belief of naturopathy is “vitalism”, which posits that living beings have a “life force” not found in inanimate objects. Naturopathic treatment ideas are all grounded in the idea of restoring this “energy”, which may explain the enthusiasm for treatments based on “natural” remedies rather than being driven by looking at what actually works. Yet despite rejecting foundational issues essential to science-based medicine, naturopathy constantly seeks the credibility that science implies. Hence the declaration that this year’s Nobel winners are somehow naturopathic.
The histories of ivermectin and artemisinin are testaments to the power that science can bring to natural substances remedies and traditional medicines. Traditional practices of herbalism or natural medicine could never have turned either of these discoveries into life-saving medications. They wouldn’t even have been identified. Natural sources (and in the case of artemisinin, traditional medicine practices) helped identify candidate substances. But with each, there was a long and laborious development process that followed, from isolation, to testing, to trials and finally, manufacturing and distribution. Science delivered. And millions are alive, or live without disability, as a result.
