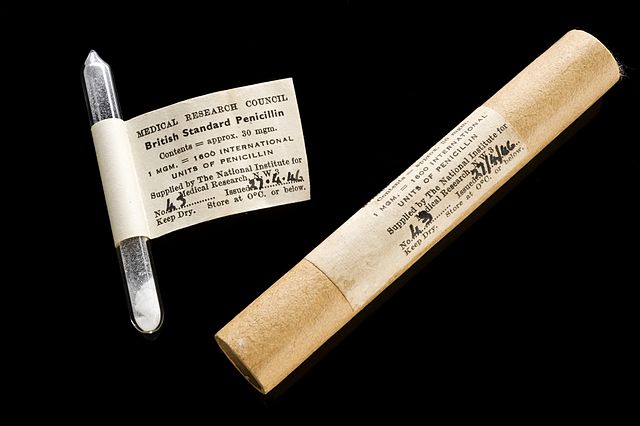
Phial of penicillin from 1946, marking the advent of the now-closing “antibiotic era”. Image from the Wellcome Trust via the Wikimedia Commons.
Recently I had a cutaneous abscess which was treated (quite painfully) with incision and drainage. My doctor told me that antibiotics were not strictly necessary, but I could have them if I wanted. The idea of any treatment that could resolve the abscess more quickly was appealing, but I did not want to contribute to the unnecessary use of antibiotics so I declined.
The use of antibiotics in cutaneous abscess is not straightforward, as there are indications – signs of systemic infection, failure to resolve quickly with just I&D, or in immunocompromised patients. Antibiotics may also reduce the risk of recurrence. These are, after all, bacterial infections.
If I were not very familiar with the issue of antibiotic overuse and emerging resistance I probably would have caved and accepted the antibiotics, and I suspect most patients do. Many patients probably request antibiotics or at least ask about them. I declined, and everything turned out fine.
The numbers
It has been known for a long time that antibiotics are prescribed more than they should, including to patients who likely have a viral illness which does not respond to antibiotics. Further, this contributes to antibiotic resistance, which is a serious problem. Some experts are warning that we are heading toward a post-antibiotic era.
A recently published study in JAMA, “Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010-2011,” is the largest survey of antibiotic use in the ambulatory (outpatient) setting to date. They estimated the number of antibiotic prescriptions that should be written per 1,000 people in the population and compared this to the number of antibiotic prescriptions that were written per 1,000 people. They found:
In the United States in 2010-2011, there was an estimated annual antibiotic prescription rate per 1000 population of 506, but only an estimated 353 antibiotic prescriptions were likely appropriate, supporting the need for establishing a goal for outpatient antibiotic stewardship.
That means that 153 out of 506 antibiotic prescriptions, or 30%, were likely unnecessary.
Sinusitis was the most common diagnosis treated with antibiotics in the outpatient setting, followed by otitis media and pharyngitis. Upper respiratory infections, also including colds and flus, were the most common type of infection treated with antibiotics, but antibiotic use was only appropriate in about half of cases.
Upper respiratory infections are usually caused by viruses, which do not respond to antibiotics, which are only active against bacteria. However, sometimes such infections can be caused by bacteria. This is often a bacterial superinfection – fighting off the viral illness leaves the tissue more vulnerable, allowing for bacteria to establish a second infection.
Why are antibiotics overprescribed?
Human behavior is always complex and it is difficult to tease out various factors. The question of why doctors are prescribing antibiotics when they shouldn’t is no exception.
When doctors are asked their most common response is that they are pressured by patients and parents of sick children to prescribe them. Other factors have also been suggested, however.
Patient education can be time consuming, and writing a prescription may be the pathway of least resistance for a busy practitioner. We also live in a time of waning trust in professionals. The old paternalistic model is dead. Now everyone feels it is appropriate to question experts, especially when it comes to their own health. This is reasonable to an extent, but it makes it more difficult for a physician to refuse a request by a patient who feels that they “know their own body” and what they need.
Even experienced doctors may also doubt themselves. We also live in an era of defensive medicine, in which a doctor may not wish to risk a complication, especially if they are going against the strong desires of their patient. This situation feels like a lawsuit waiting to happen.
By contrast, the risk of antibiotic resistance is diffuse and distant. Human psychology favors avoiding the immediate direct risk for the delayed indirect risk with diffuse responsibility.
It also should be recognized that it takes much more expertise to feel comfortable not doing something than it does to do something. Knowing when a treatment or diagnostic study is not necessary requires more knowledge and experience then knowing how to use the treatment or study. For this reason, increasing expertise tends to be associated with fewer interventions and more efficient practices.
I point this out because it is important to recognize that reducing inappropriate antibiotic prescriptions requires more than basic competence. It requires confident expertise and adequate support.
Related to this is the difference between analytical and intuitive thinking styles in medical practice. An intuitive style might be: this patient looks really sick and in my experience they are going to end up needing antibiotic, so I will give them a prescription now. An analytical approach would be: only a small percentage of patients with acute sinusitis statistically will require antibiotics, so regardless of my personal feelings and experience, I will practice according to published evidence-based guidelines.
Most physicians use a combination of analytical and intuitive thinking styles in practice, but it can be difficult for physicians, and especially so for patients, to do not what feels right, but what is dictated by cold hard numbers.
Where do we go from here?
Clearly overprescribing antibiotics is still a huge problem and needs to be addressed more aggressively. Physician education has been the primary mechanism of addressing this problem, and will likely remain the cornerstone of such efforts.
Physician education, at least as currently practiced, is apparently not enough, however. Physicians need to be educated not only about the evidence-based guideline of when and when not to prescribe antibiotics, but also how to feel confident in their decisions, and how to deal with patients who ask about, request, or even demand antibiotics.
Patient education is also critical. Public education about the problems of antibiotic overuse is underway, but given the recent data probably needs to increase.
Individual prescribers could also benefit from a support structure, in their practice or institution. This can include reviews of prescribing practices, educational material for patients, and feedback to improve prescribing practices.
We will never reduce inappropriate antibiotic prescriptions to zero. Medicine is too complicated, and there are many gray zones requiring judgement calls. Also, medical best practices often include a little buffer – you need to have a certain negative rate to make sure you are capturing all the positives. So, you may need to prescribe antibiotics to some patients who may not have needed them to make sure everyone who does need antibiotics gets them.
But clearly 30% is too high. Something like 5-10% is probably a realistic and appropriate goal.
The needs of the patient versus the needs of society
The final tricky part about this issue is that of the needs of the patient vs the needs of society. Physicians are trained, and our ethics demand, that we think first of the patient in front of us. We are their health advocate. We consider the risks vs benefits to that patient of any intervention.
In the case of antibiotics, however, we are being forced to consider the risks to society as a whole, which does also include the risk of future patients. A physician, therefore, might feel that the risk of unnecessary antibiotic use to their patient is small, while the risk of delayed treatment, if it turns out to be a bacterial infection, could be quite high. This calculation favors prescribing antibiotics liberally.
We are now being forced to consider, however, the long term effects to society in terms of antibiotic resistance. This means we have to perhaps accept a small increase in risk for the patient in front of us (at least it may feel this way, even if it is not strictly true) to avoid a very bad long term outcome.
To optimize success, I think it’s necessary for the physician and the patient to be partners. They both have to be on the same page, understanding the importance of following strict guidelines when it comes to antibiotic use. This is a societal problem, and fixing it has to be a societal effort.
