Hmm, what could have happened in the early 90s to explain the significant decrease in incidence of acute hepatitis B? Urkel?
For those of you new to Science-Based Medicine, I am a pediatric hospitalist and spend the majority of my time caring for newborns. It’s an extremely rewarding experience on most days. The babies are usually healthy, the parents are usually happy and appreciative, and I get to give a lot of good news. I also get to dispel a lot of myths and misconceptions regarding the care of infants, which as you can probably imagine, I take great pleasure in.
Parents ask a lot of questions, which I appreciate and encourage, but they also make a lot of claims about the care of children based on their prior experience, advice from well-meaning friends and family, or their evaluation of the online “literature.” Some of these claims I will challenge, nicely of course, when they are demonstrably wrong or increase the risk for a bad outcome. (“We read that babies should sleep inverted like a bat in order to increase blood flow to the brain.”) Some of these claims I acknowledge as an acceptable approach, even if I don’t agree with them myself, if there is low risk or a lack of available quality evidence to guide me. (“We burped our last baby every five minutes during feeds to prevent colic.”) Sometimes I even learn a thing or two from parents.
The safe, universally-recommended hepatitis B vaccine
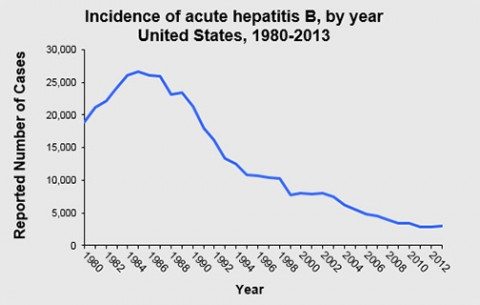
A topic that frequently leads to both questions and claims from concerned parents during rounds in the newborn nursery is the vaccination against the hepatitis B virus (HBV), something that has been recommended universally for infants by the Advisory Council on Immunization Practices (ACIP) since 1991. Their strategy was, and still is, to wipe this awful disease out in the United States. Over the years, the recommendation for timing of the first dose has changed from “at birth before hospital discharge or at age 1-2 months” to simply “newborns before hospital discharge” in 2002, with qualifiers of medical stability and weight greater than 2,000 grams added in 2005. Babies that weight less than 2 kg at birth still will get the vaccine at discharge home or at 1 month of age if still in the hospital. This last change was recommended because of concerns over efficacy rather than safety. It’s an extremely safe vaccine.
In addition to questions about the vaccine, the most common being about any associated risks and the necessity for a newborn dose, I also get a fair amount of refusals despite attempts to educate and reassure. Most of the time these aren’t anti-vaccine parents, they just don’t understand why it can’t wait until they take the baby in to see their primary care pediatrician. They may assert that their child doesn’t need it at such a young age, that it’s not necessary considering the infant’s low risk of exposure. Many are medically savvy enough to question the need for the vaccine given negative testing in the mother. Thankfully, most of these families do go on to allow their babies to receive all the recommended vaccines on the ACIP schedule.
Only once in my career of roughly 12 years have I had a mother with active HBV refuse the immunization for their newborn. That is an entirely different issue which I will get into shortly. Questions about the need for giving the baby of a mother who has tested negative for hepatitis B infection a vaccination to protect them from a disease commonly thought of as an adult affliction, and related to “adult” behaviors, are understandable. But before I explain why we have this recommendation in place, a primer on the disease we are trying to avoid is in order.
What is hepatitis B?
Hepatitis B is an infection of the liver caused by the hepatitis B virus (HBV). According to the CDC, there were 3,050 cases of acute infection reported in the United States in 2013, which comes out to roughly 1 case per 100,000 people. In children under the age of 15 years, the incidence is now only .02 per 100,000. The numbers of reported acute infections in kids has plummeted since the vaccine was first recommended for all infants in 1991, and is down from nearly 14 per 100,000 in the 1980s. Overall there has been an almost 90% reduction in the diagnosis of new cases.
It’s important to point out that these numbers likely significantly underestimate the actual number of new infections with HBV. Because the acute infection frequently doesn’t cause any symptoms, many cases go unreported. After taking this into account, the CDC estimates that there were actually close to 20,000 new cases in 2013. Most acute HBV cases will fully resolve without any need for intervention, however a certain percentage will go on to develop chronic infection, with younger patients being at higher risk. It is estimated that between 700,000 and 1.4 million people currently have chronic hepatitis B in the United States.
From a global perspective, HBV causes significantly more illness and death than in the United States. The World Health Organization, which also recommends universal immunization of newborns against HBV, puts worldwide cases of chronic disease at around 240 million people. And three quarters of a million people die each year from acute (130,000) or chronic (650,000) infection.
Acute hepatitis B infection
The presentation of acute infection with HBV is extremely variable, ranging from a complete absence of symptoms to severe and sudden onset of liver failure that is life-threatening and requires aggressive treatment. This is a rare complication that occurs in less than 1% of cases, however. In general, when signs and symptoms of illness do occur, they tend to be similar in presentation in all age groups with loss of appetite, nausea, an inflamed and tender liver, and jaundice being typical. Fatigue can be severe in some patients, and persist long after the other complaints have resolved, which usually takes one to three months. Some patients will also develop more significant systemic symptoms consisting of muscle and joint pain, hive-like rashes, and tender swollen lymph nodes.
Most patients over the age of five years who are acutely infected with HBV will clear the virus and go on to benefit from lifelong immunity. But almost 90% of infants and 25%-50% of children between the ages of one and five years will not be so lucky. In contrast, 95% of older children and adults will fight off the virus during the initial exposure. The ability to fight off the virus clearly improves with age. The younger the patient, the more likely they will develop chronic infection and be at risk for devastating future complications.
Chronic hepatitis B infection
Patients with chronic HBV infection are often asymptomatic for decades. Children typically develop as expected and without any disability, but can present with kidney disease long before any liver problems. But it is the slow and steady injury to the liver, although sometimes it can be sudden and severe, that can occur which causes the greatest risk for eventual morbidity and mortality.
How chronic HBV infection naturally plays out in kids is complicated, and like acute infection it presents in different ways. The complicating factor is something called immune tolerance, a unique result when infection occurs in younger patients, particularly newborns who acquire the infection from their mother around the time of birth. Immune tolerance is the state where, although there is evidence of viral replication in the patient, there is little to no laboratory evidence of liver inflammation. This phase can last for months to decades and can go undetected. Even when identified, treatment is generally not recommended because of poor efficacy and concern for inducing antiviral resistance.
Seroconversion and clearance of infection
At any point during the immune tolerant phase, it is possible for the patient to develop antibodies against a key component of the virus (“seroconversion”) and rarely, to even clear the infection. This is very unlikely to occur when a child is infected in early infancy, with a conversion rate of about 5% per year. Kids who acquire the infection a bit later and from a source other than their mother have better chances, even as high as 70%-80% over the first 20 years. Again, development of these antibodies doesn’t mean that a patient will clear the virus and be cured, only that they have a chance. And unfortunately, conversion and even clearance of the virus doesn’t necessarily prevent all long term complications.
Immune active infection
The next potential component of chronic HBV infection is the so-called immune active phase. For reasons we don’t fully understand, at any time a patient can develop increased replication of the virus and increased inflammation of the liver. This is where significant and prolonged liver injury can occur but it is also the time when the patient has the best chance to develop antibodies against critical components of the virus.
The longer that a patient is in the immune active phase, the higher the risk of cirrhosis of the liver and ultimately the development of hepatocellular carcinoma (HCC). That’s right, the hepatitis B vaccine was the first vaccine to successfully prevent cancer, not the vaccine against human papillomavirus. This stage is typically treated with antiviral medications in order to limit injury to the liver and help increase the likelihood of seroconversion, although the success rates aren’t great in children.
Inactive carriers, aka Hepatitis Mary
After seroconversion occurs, these patients are considered inactive carriers. They have no liver inflammation and low or undetectable viral replication. They have developed important antibodies against the virus, and have a chance to clear the infection, but they are still at risk. As many as 20% will revert back to the immune active phase at least once, and 20-30% will enter a reactivation phase where their viral load will increase and liver inflammation can return despite the improved immune response. The reactivation phase can result in rapid deterioration of liver function and is also frequently treated with antiviral medications, but these patients will rarely go on to ever clear the virus so will always be at risk for long term complications.
What are the long term complications of chronic hepatitis B virus infection?
Cirrhosis of the liver and hepatocellular carcinoma (HCC) are the primary long term complications of chronic infection with HBV acquired during childhood. These don’t tend to occur until much later in life but injury in the form of fibrosis, essentially scarring of the liver, is common within just a few years of infection. Unchecked fibrosis is what can lead to cirrhosis, and ultimately loss of liver function, years to decades down the road.
Liver cancer in the form of hepatocellular carcinoma, unlike fibrosis and cirrhosis, remains a potential bad outcome even in patients who have converted to less inflammatory phases of HBV infection, and even in patients who do eventually clear the virus. Adults who were infected as infants can have a rate of HCC diagnosis as high as 5% per year. In general, the more time that a patient spends with active inflammation of the liver, and the longer it takes for antibody conversion (if it happens at all), the higher the risk of HCC.
According to the CDC, one out of every four children who develop chronic infection with HBV will die as a result. Of the patients who are exposed outside of childhood and are unlucky enough to develop a chronic infection, 15% will ultimately die earlier than they should have because of it. There are a few thousand people every year that die from this vaccine-preventable illness, despite improvements in drug therapies and even liver transplantation.
How is the hepatitis B virus spread?
Historically in the United States, and currently in countries where HBV infections are endemic, the virus has most commonly been spread from an infected mother to their baby during the birth process. Babies are frequently exposed to a significant amount of blood and body fluids at delivery, so this should make sense. As it stands in the United States now, because of the success of the vaccine the virus is no longer endemic and infections are much less common. So the most common route of spread here is through sex with an infected partner or by being stuck with a contaminated needle.
But the virus can be transmitted from one person to the other through a variety of routes that don’t involve shooting up, healthcare workplace accidents, or risky sexual activity. Viral particles can be found in other infected body fluids, such as saliva contaminated by bleeding gums or biting the inside of the cheek. Children can spread it to each other during close contact in a household or if one toddler bites another. Transmission can also occur when sharing a toothbrush or borrowing a razor. These are all unlikely, but the risk is real and cases happen every year in young children and low-risk adults.
The people who spread the virus to others are often asymptomatic and don’t even know that they are infected. Furthermore, HBV can survive on surfaces for more than seven days and still retain the ability to cause infection. Think about that as your infant crawls around the floor of the gym at their daycare center putting everything within reach straight into their mouth.
Why newborns?
So now we’ve come full circle. As I stated at the beginning of the post, many parents are hesitant to consent to a vaccine that they believe isn’t really necessary in such a young child. They may question the risk of exposure to HBV because all they know about it comes from sources like Dr. Bob Sears:
Let’s take a look at the two different schedules. One of the main differences that the CDC schedule dictates is they suggest the hepatitis B vaccine be given the day a baby’s born, one month later, and then six months later. Now, if you look at hepatitis B, it’s a sexually transmitted disease. The only way a baby can catch it is through blood or body-fluid exposure, and that’s extremely unlikely to happen for any baby or young child in the United States.
So what I did on my schedule is, I took a more logical look at hepatitis B, and I realized that babies have no risk of catching this disease, so let’s not do the hep B vaccine while a baby’s young and small and more vulnerable. Let’s do a hepatitis B vaccine when a child’s more of a preschool age, where he or she is going to be entering school and be running around with a lot of other kids, and there could be some blood or body-fluid exposures in those kinds of situations. To me, that’s just a more logical time frame to do the hepatitis B vaccine. And some parents would even take it a step further and decide to delay their children’s hep B vaccine until their children are teenagers and the real risks of hepatitis B, such as sexual activity or [intravenous] drug abuse, come into play.
His rationale amounts to waiting until they are completely past the stage where children have the highest risk of developing chronic infection and ultimately dying of liver disease or cancer. And babies are exposed to blood and body fluid, as are toddlers who haven’t started preschool, when they have siblings or are in daycare. We do test mothers for HBV activity during pregnancy but no test is perfect and information transfer from the OB or lab to the newborn service can be lost or accidentally altered.
There are 25,000 infants born to mothers that carry the virus every year in the United States that we know of. If something goes wrong and a mother is falsely labeled as negative or unknown status, that baby can have up to a 90% chance of acute infection depending on what phase she is in (immune active with high viral load has the highest risk). If infected, most will develop chronic infection and of those chronically infected 25% will die because of it.
Sears is spreading dangerous misinformation but he’s not the worst of the fearmongering anti-vaccine crowd. Our friends Mercola and the NVIC unsurprisingly take it much further. Perhaps I’ll cover their nonsense in a future post.
In addition to serving as a safety net and protecting those most vulnerable to the devastating potential outcomes of this infection, we also recommend the newborn dose because it increases the likelihood that the child will go on to get the full series of 3-4 shots and be fully protected. And protected kids can’t spread the infection to the unprotected. And despite claims from the usual suspects of antivaccine rhetoric, the safety and efficacy of this vaccine is firmly established.
Conclusion: Vaccination can be scary, but it is necessary; it is necesscary
We expect a lot from parents in the newborn nursery. They are asked to allow their little bundle of joy to go through a long list of interventions that take the baby away from their sight and can cause discomfort: antibiotic eye ointment, vitamin K injections, heel sticks for metabolic screening, hearing testing, jaundice levels, screening for heart defects, and finally, the hepatitis B vaccine. And that’s in a perfectly healthy baby. Considering this, and the lack of good public understanding of hepatitis B and the need for immunizing the very young, I’m not surprised that many refuse.
But these concerns, as understandable as they are, are unfounded. The vaccine is extremely safe, and the benefit far outweighs any small degree of risk. Protection from hepatitis B infection, which thanks to the success of the vaccine is now uncommon in the U.S., is still very important considering the potentially life-threatening complications. Complications which are significantly more likely to occur in patients infected when they are infants.
