Tag: Choosing Wisely

The American Chiropractic Association Answers Crislip’s Call, Joins the Choosing Wisely Campaign
The Choosing Wisely campaign has invited the largest chiropractic organization in the United States to publish a list of interventions to avoid. The results, while not entirely without merit, consist of redundant or unnecessary recommendations. And there is a glaring absence of recommendations to avoid any of the blatant pseudoscience commonly practiced by chiropractors.
How accurately do physicians estimate risk and benefit?
A new study suggests that physicians tend to overestimate the benefits of treatments, tests, and screening tests, while also underestimating harms.

On “integrative medicine” and walking and chewing gum at the same time
Evidence matters. Science matters. However, when advocates of "integrating" quackery into medicine via the vehicle of "integrative medicine" invoke weak science and poor quality evidence in conventional medicine in response to criticism, what they are really doing is deflecting attention away from their quackery. More importantly, advocates of science-based medicine are capable of walking and chewing gum at the same time. We...
Choosing Wisely: Changing medical practice is hard
One of the hardest things to do in medicine is to change practice in the face of scientific evidence that what you're doing isn't working. Quacks never change, but medicine does. The change might be slower and messier than we would like, but change does happen. Choosing Wisely is an initiative designed to bring about change by discouraging the use of interventions...
Less benefit, more risk. Our assumptions about health treatments are probably wrong.
I’m a health professional, but sometimes a patient as well. And like most patients, I generally don’t want health decisions being made without my input. Yes, I want the best medical information, and the advice of medical professionals, but ultimately I want to make my own decisions about my care. That’s the norm in health care today, but relatively new in the...
In the Spirit of Choosing Wisely
Oh, loneliness and cheeseburgers are a dangerous mix. – Comic Book Guy Same can be said of viral syndromes and Thanksgiving. My brain has been in an interferon-induced haze for the last week that is not lifting anytime soon. Tell me about the rabbits, George. But no excuses. I have been reading the works of Chuck Wendig over at Terrible Minds. (Really,...
Separating Fact from Fiction in Pediatric Medicine: Infant Gastroesophageal Reflux
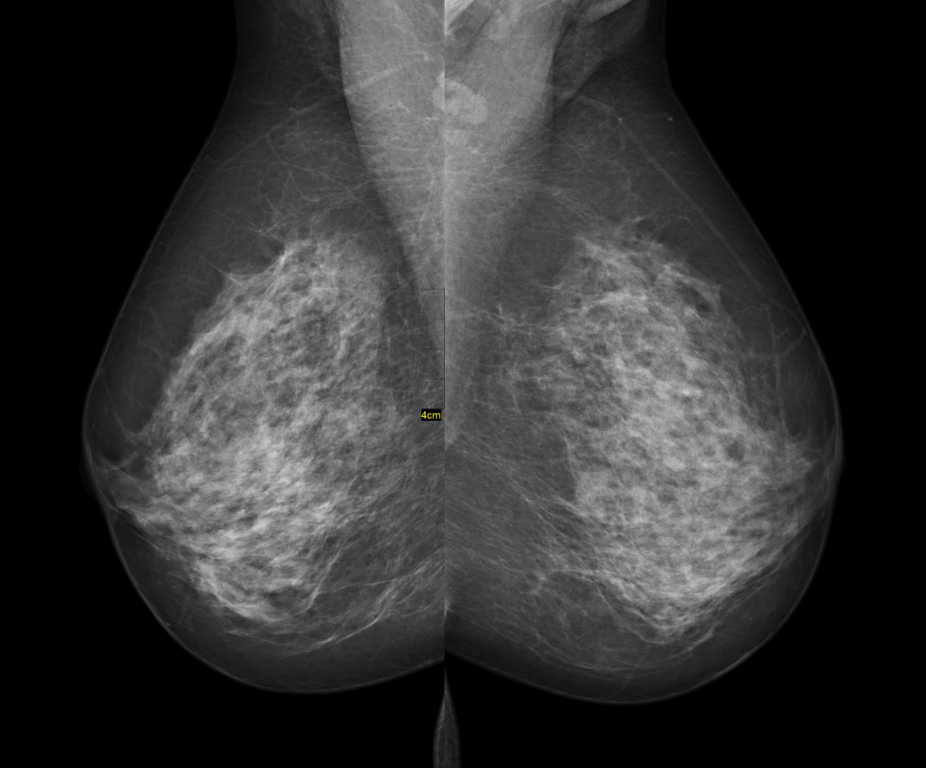
By now, regular SBM readers should be aware of the Choosing Wisely initiative. Just in case, Choosing Wisely is a campaign developed by the ABIM Foundation to bring together experts from a variety of medical specialties in order to identify common practices that should be questioned by patients and providers, if not outright discontinued. Their ultimate goal was not to establish treatment...
Doctors Are Not “Only Out to Make Money”
There’s an old joke about the doctor whose son graduates from medical school and joins his practice. After a while the son tells his father, “You know old Mrs. Jones? You’ve been treating her rash for years and she never got better. I prescribed a new steroid cream and her rash is gone!” The father responds, “You idiot! That rash put you...
An experiment in paying through the nose for “unnecessary care”
Rats. Harriet stole what was going to be the title of this post! This is going to be something completely different than what I usually write about. Well, maybe not completely different, but different from the vast majority of my posts. As Dr. Snyder noted on Friday, it’s easy to find new woo-filled claims or dangerous, evidence-lacking trends to write about. Heck,...
The Overuse of Antibiotics for Viral Infections in Children
“For every complex problem there is an answer that is clear, simple, and wrong.” -H. L. Mencken As I sit in an apartment full of unpacked boxes and grumpy children, only a few days removed from driving 1,600 miles to a 3rd floor walk-up and a better life just outside of Boston, I find the task of writing a post somewhat daunting....

