Tag: complementary and alternative medicine

If You Think Doctors Don’t Do Prevention, Think Again
One of the common criticisms we hear from alternative and integrative medicine proponents is that doctors don’t do anything to prevent illnesses and have no interest in prevention. They claim that doctors are only trained to hand out pills to treat existing illnesses. Sometimes they even accuse them of deliberately covering up cures and wanting to perpetuate illnesses like cancer so they...

“Complementary and Integrative Health” at the VA: Integrating pseudoscience into the care of veterans
In return for their service to our country, veterans deserve the best science-based medical care that we as a nation can provide. Unfortunately, the VA is integrating quackery into its medical care even more enthusiastically than medical academia.
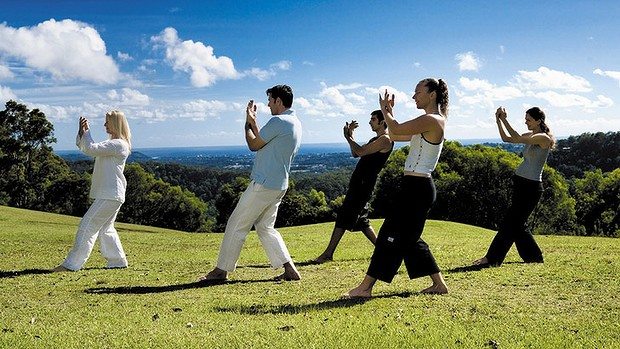
Tai Chi versus physical therapy for osteoarthritis of the knee: How CAM “rebranding” works
“Complementary and alternative medicine” (CAM), now more frequently referred to as “integrative medicine” by its proponents, consists of a hodge-podge of largely unrelated treatments that range from seemingly reasonable (e.g., diet and exercise) to pure quackery (e.g., acupuncture, reiki and other “energy medicine”) that CAM proponents are trying furiously to “integrate” as coequals into science-based medicine. They do this because they have...

CAM use and chemotherapy: A negative correlation
"Complementary and alternative medicine" (CAM) is represented as safe because it is administered alongside conventional medicine, despite the fact that for the vast majority of CAM modalities there is little or no evidence for efficacy. However, as a new study shows, cancer patients who use CAM tend to be more likely to refuse conventional cancer treatment.
A Harris Poll on “Alternative Medicine”
Mark Twain popularized the phrase, “There are three kinds of lies: lies, damned lies, and polls and surveys.” (He may have said “statistics” at the end, but I think this version works as well.) A new Harris Poll on “alternative medicine” nicely demonstrates some of the problems with polls. The biggest problem is how you frame the questions. You can dramatically affect...
April Fool Cannot Surpass SCAM
It’s April Fools’ day in the US of A. One of the internet traditions is to come up with a story that is weird or unlikely, but not so weird or unlikely that it is not believable, in order to fool people that the story is real. I gave it the old SBM try, I really did, but I couldn’t do it....

More drugs, more supplements, and potentially more problems
Early in my career I was fortunate to be offered a role as a hospital pharmacist, working on an inpatient ward along with physicians, nurses, and a number of other health professionals. My responsibilities included conducting a detailed medication review with each newly admitted patient. We would sit together, often with family members, going through what was sometimes a literal garbage bag...

The hijacking of evidence-based medicine
A hero of the blog, John Ioannidis, worries that evidence-based medicine has been hijacked, and when Ioannidis says something we at SBM listen. But has EBM been "hijacked"?
Is it ethical to sell complementary and alternative medicine?
Complementary and alternative medicine may be legal to sell - but is it ethical to sell?


About Herbs: an app to avoid
Medicine has an intellectual hierarchy. Supposedly the best and the brightest are in the academic medical centers and are the thought leaders in their field. Those of us lower in the hierarchy are well aware of some of the warts present on our betters, but I would expect those at the top would adhere to the highest intellectual and ethical standards. People...