Tag: Ted Kaptchuk

The Magic Feather Effect: Placebos and the Power of Belief in Alternative Medicine
In her book The Magic Feather Effect, journalist Melanie Warner covers placebo research, shows that alternative medicine is placebo medicine, takes a "try it yourself" approach, and gives belief and anecdotes more credit than they deserve.

Are placebo effects genetically determined?
We frequently write about placebo effects here at SBM because understanding placebo effects is essential to understanding a lot of clinical trial science and, most relevant to the topics of this blog, how those promoting unscientific medicine misunderstand and misuse placebo effects to promote quackery. Last week, The NYT published an article asking if placebo effects are genetically determined. The evidence supporting...
Academic Consortium plan: force medical residents to practice integrative medicine
“Integrative medicine” (IM) is an ideological movement within medicine driven in large part by those whose livelihoods depend on its continued existence. This includes both those with positions in academic medicine and individual practitioners who use the IM brand to attract patients. Despite IM and its antecedents (alternative, complementary, alternative and complementary, complementary and integrative) having been around for about a quarter...
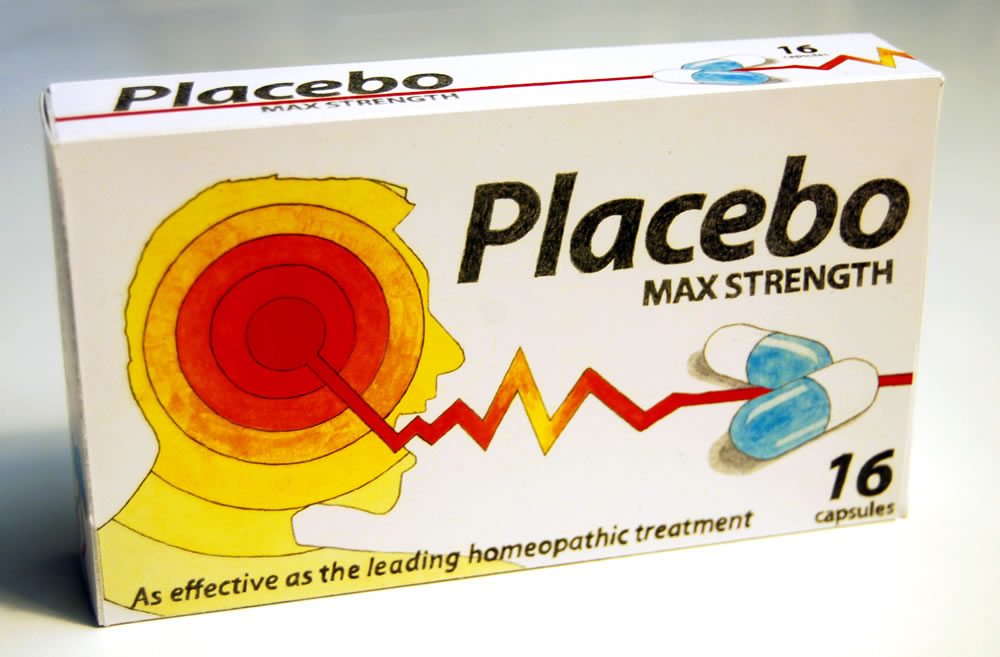
American Journal of Public Health article touts “potential public health benefits” of homeopathy
An article in the April, 2016 issue of the American Journal of Public Health caught my eye: “Homeopathy Use by US Adults: Results of a National Survey.” I was pleased to see that homeopathy use is actually quite low. The 2012 National Health Survey found that only 2.1% of U.S. adults used homeopathy in the last 12 months, although that was a...
Cure Is About Caring, Not Curing: Placebos, Alternative Medicine, and Patient Comfort
In a recent post, Dr. Gorski criticized two articles by Jo Marchant on placebos and alternative medicine. He mentioned that she had a book coming out and suggested I might want to review it. The title is Cure: A Journey into the Science of Mind Over Body. I don’t know of any evidence that the mind has ever cured a disease, so...
Is “harnessing the power of placebo” worthwhile to treat anything?
We frequently write about placebo effects here on Science-Based Medicine. The reason is simple. They are an important topic in medicine and, at least as importantly, understanding placebo effects is critical to understanding the exaggerated claims of advocates of “complementary and alternative medicine” (CAM), now more frequently called “integrative medicine” (i.e., integrating pseudoscience with science). Over the years, I (and, of course,...
What is Science?
Consider these statements: …there is an evidence base for biofield therapies. (citing the Cochrane Review of Touch Therapies) The larger issue is what constitutes “pseudoscience” and what information is worthy of dissemination to the public. Should the data from our well conducted, rigorous, randomized controlled trial [of ‘biofield healing’] be dismissed because the mechanisms are unknown or because some scientists do not...
Woo-omics
Every so often, I come across studies that leave me scratching my head. Sometimes, these studies are legitimate scientific studies that have huge flaws or come from an assumption that is very off-base. Other times, they involve what Harriet Hall has termed “tooth fairy science,” wherein the tools of science are used to study a phenomenon that is fantastical, whose very existence...


Placebo Effect Revisited
The New York Times and Ted Kaptchuk feed into more confusion about placebo effects.