Medicine is an uncertain business. It is an applied science, applying the results of basic science knowledge and clinical studies to patients who are individuals with differing heredity, environment, and history. It is commonly assumed that modern science-based doctors know what they are doing, but quite often they don’t know for certain. Different doctors interpret the same evidence differently; there is uncertainty about how valid the studies’ conclusions are and there is still considerable uncertainty and disagreement about things like guidelines for screening mammography and statin prescriptions.
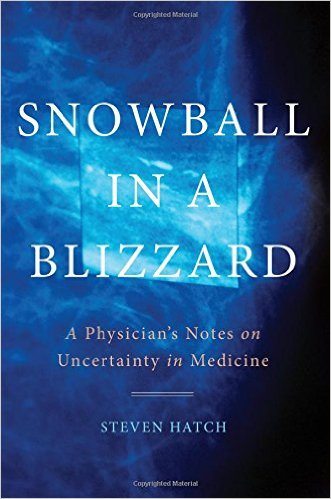
Snowball in a Blizzard by Steven Hatch, MD, is a book about uncertainty in medicine. The title refers to the difficulty of interpreting a mammogram, trying to pick out the shadows that signify cancer from a veritable blizzard of similar shadows.
Dr. Hatch starts with a clinical vignette. An elderly woman is in the ICU, and doctors on rounds are discussing her case and debating how to proceed. Her daughter asks, “So, you don’t know why she’s sick?” The doctor says he isn’t sure. “Do you think she should get a CAT scan?” He says he’s not sure; it would help pin down a diagnosis, but there is a risk that the contrast material might damage her ailing kidneys, perhaps irreversibly. “Do you think she needs antibiotics?” “Yes, I’m pretty sure, at least until we have another explanation that would indicate we can safely stop them.” As with practically everything in medicine, it’s complicated.
Dr. Hatch says:
Uncertainty lies at the heart of what physicians do on a daily basis. Sometimes they are entirely aware of it, and sometimes they fail to appreciate it. Sometimes it prominently features in discussions between doctor and patient. And sometimes it is completely misunderstood. The purpose of this book is to show the reader not only that this is so, but how it is so as well.
And he does a superb job. He provides numerous examples and clear explanations, covering many of the topics we have addressed on Science-Based Medicine. Very little in his book will be new to our regular readers, but he ties a lot of information together into a convenient package. He explains the many ways in which clinical research can yield misleading results, the difference between absolute and relative risk, the difference between correlation and causation, the number needed to treat (NNT), predictive value, the process of developing treatment guidelines, how the precision of new diagnostic technology is often mistaken for certainty, the dangers of false positive tests, the inability of doctors to predict how long an individual patient has to live, the hazards of unnecessary tests and overdiagnosis, how evolution prepared us to find narrative more compelling than statistics, confirmation bias, how our skill at pattern recognition makes us see patterns that are not real, pseudodiseases, the rationale for controlled trials with randomization and blinding, media malfeasance, illogical conspiracy theories, and much more.
He boils down the things we know for certain about maintaining our health to three principles: exercise more, eat less, and do not smoke. “Everything else is commentary.”
He provides a wealth of examples:
- The Rosenhan experiment where fake patients were treated as schizophrenics, highlighting the uncertainty of psychiatric diagnosis.
- PSA screening: the debate boils down to one life saved for every 1,000 men screened over 10 years versus many lives impacted by invasive procedures and unnecessary treatment.
- Mammography: the data on the balance of benefits and harms for women under the age of 50, and how politics and misunderstandings made people question the unanimous consensus guidelines of experts.
- Blood pressure treatment: how uncertainty led to genuine controversy among the experts.
- Chronic Lyme Disease (CLD): it probably isn’t real, and there is clear evidence that prolonged antibiotic treatment does no good. The experts agreed unanimously, but a group of CLD advocates influenced public opinion. An independent panel “whose scientific integrity and objectivity was deemed unimpeachable by both parties” agreed with the scientific consensus. But the CLD advocates still managed to get legislation passed, using government bureaucracy to overthrow the scientific findings. Hatch tells the depressing story in all its excruciating detail.
- Controversies over statins, antidepressants, and blood pressure drugs: he explains why assessing the benefit/risk ratio is tricky. The benefits are greater for the more severely affected patients. Lowering systolic blood pressure from 170 to 140 clearly saves lives; lowering it from 150 to 140, not so much.
- How a treatment with uncertain benefits (DES to prevent miscarriage) was found to probably cause cancer in the children of mothers who took it during pregnancy.
- The hormone replacement debate and how the study results were misrepresented to the public, with media-induced hysteria (“if you value your life, don’t even be in the same room as a bottle of hormones.”)
- The HPV vaccine manufactroversy, where the media imagined a controversy that didn’t exist, based on misleading reports of adverse effects and deaths from the VAERS database. He points out that when you do anything to 10 million people, even give them a glass of water, some of those people will develop serious medical problems (that they were going to develop anyway).
Conclusion: Uncertainty and hope
There is a lot of discouraging news here, but there is also hope. By understanding the principles in this book, patients can better judge the uncertainties of what they hear. He praises HealthNewsReview.org, a website that can help consumers make sense out of media reports. They found that one in three news stories is a mere regurgitation of a press release that lacks critical information. He doesn’t mention Science-Based Medicine, which we think is another valuable source of reliable information; but he does cite Orac on page 199. Medicine is full of uncertainties, but doctors and patients can work in partnership to understand where a diagnosis or treatment falls on the uncertainty spectrum and that information can help them make rational decisions for individual health care.