If you’re a regular reader of this blog, I’ll bet you’re not a regular consumer of vitamins or supplements. I’m in that group. Aside from sporadic vitamin D in winter, I don’t take any vitamins or supplements routinely, nor do I give any to my children. Your reasons may be close to mine: There is little to no evidence suggesting that dietary deficiencies are widespread, nor is there good evidence to suggest that vitamin supplements are beneficial in the absence of deficiency. I don’t have any need for an other supplements, nor am I confident in the scientific evidence for many of them.This position of “no supplements” is a cautious and conservative one, but is based on a consideration of the scientific evidence. I view decisions about healthcare as evaluations of risk and benefit, and then cost if necessary. Given supplementation (with some exceptions) has no demonstrable benefits and, in some cases, a little risk, the odds favour not supplementing in most cases. Add in costs, and it’s even less attractive as a routine health strategy.
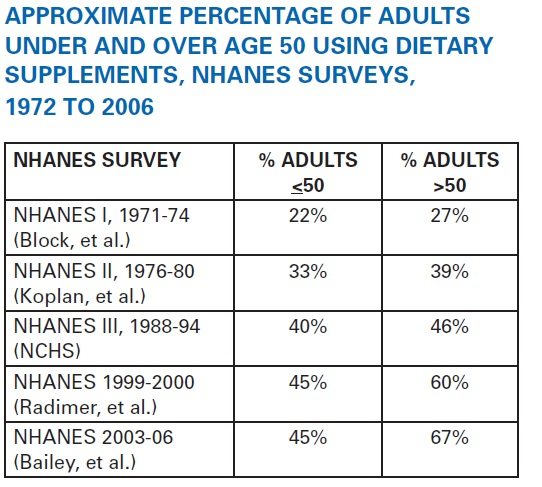
Yet a decision not to take vitamins or supplements regularly is becoming a minority position. Supplement use has grown over the past 40 years among Americans, with the National Health and Nutrition Examination Survey (NHANES) showing steadily increasing utilization among younger and older adults:
Supplement makers promote an image of being small, ethical, and natural — the exact opposite of evil Big Pharma. Yet the numbers show this is big business: a $30 billion (USD, 2011) industry which (as has been noted regularly at this blog) has limited regulatory oversight. The result is a marketplace with products listing exaggerated claims that aren’t supported by credible evidence. Yet industry surveys suggest 85% of Americans are confident in the safety, quality, and effectiveness of these products.
Given the (lack of) good evidence showing benefit, why are consumers so fond of these products that they willingly shed out $30 billion per year for supplements? It’s a question I regularly ask myself when consulting with patients who enquire about supplements as a complement to, or as a substitute for, more conventional treatments. It’s a testament to the marketing of these products that they are (from my own observations) perceived as being safe and effective, in contrast to drug products. The reason that I’m not promoting them, I’m sometimes told, is because I’m not trained in “botanicals” or “herbals,” unlike the friendly neighbourhood naturopath, who routinely recommends a long list of supplements, in contrast with my typical advice to see a medical doctor, or to make basic lifestyle and dietary changes first.
As a pharmacist I have a simple goal with my patients: improve health by improving medication use. I don’t distinguish between drugs, vitamins, and supplements. If they’re being taken for a therapeutic use, they’re fair game. I do this in part by interpreting the scientific evidence to support patient self-care decisions. So as an advocate for science-based medicine, I admit to finding the surging popularity of supplement use a bit frustrating. I’ve seen people spend $100 or more per month on a variety of supplements, most of which are either unproven, or proven ineffective. At the same time, they may reject or defer strategies backed by better evidence. Now $30 billion could likely be used much more effectively for health care if redirected towards the strategies that offer more health “bang for the buck”. So if the goal is to change behaviors, the motivations need to be understood. And I can’t rely on my own biased sample — I need a more systematic analysis.
Happily, consumer patterns and motivations have been studied. Published earlier this month in what used to be called the Archives of Internal Medicine (now called JAMA Internal Medicine) was Why US Adults Use Dietary Supplements by Reagan L. Bailey and colleagues from the Office of Dietary Supplements at the National Institutes of Health. It also relies on the NHANES dataset, a representative survey of US civilians which began collecting specific information on reasons for supplement use in 2007. Data are collected through interviews, and a Dietary Supplement Questionnaire was used to gather detailed information on each participant’s use of vitamins and other supplements. This survey reports the results from 11,956 adults (children, young adults (< 20 years), and all pregnant and lactating women were excluded from analysis). Here’s the snapshot of the participants:
- 49% of adults used a supplement of some kind in the prior 30 days: 54% of women, 43% of men.
- Supplement use increased with age: 34% aged 20-39, 50% age 40-59, and 67% over age 60
- Non-Hispanic whites use more supplements (54%) than Non-Hispanic blacks (38%) or Hispanics (33%)
- Supplement use is greater in “never” (51%) or “former” (59%) smokers compared to current smokers (30-36%)
- Supplement use is much more common in those with health insurance (53%) than those without (31%)
- Supplement use parallels reported exercise, from “low” (43%) to “moderate” (54%) to “high” (56%).
- Supplement use was higher among those that reported “excellent” or “very good” health (55%) versus “good” (47%) or fair/poor (44%)
So far this is as expected: supplement users tend to be wealthier and healthier than non-users. It’s the “healthy user” effect which shows up throughout epidemiological studies, confounding evaluations of outcomes. That is, we shouldn’t assume supplement use make you healthier, any more than assuming that supplement use makes you wealthier.
Here are the most common reasons for taking supplements:

The most common motivations for taking supplements were to “improve” (45%) or to “maintain” (33%) health, consistently reported between men and women. Bone health is next, with a large gender split between men (11%) and women (36%). Most of the other reasons given are equally common, with significant differences in only a few categories: Men reported more interest in supplements for heart health (18% vs. 13%) while women reported more supplementation for sleep, skin, and hair health, as well as anemia. The frustrating (and fallacious) “to boost immunity” came in at 15%, revealing just how widespread the perception is that our immunity can be “boosted” and that it can be accomplished with supplements. Motivation for site-specific use (vision, heart, bones) increased with age of the user.
The “enhanced energy” rationale for supplements was cited only 11% of the time — less common than I expected.
Knowing the motivations, let’s take a look at the types of supplements comsumed, reported in Table 3. It’s a distribution with a long tail: multivitamins/minerals are tops, with an overall prevalence of 32%. Calcium is next, at 12%, followed by omega-3 supplements/fish oils (10%), then “botanicals” (a category of herbals, probiotics, melatonin, and coenzyme q10) and the individual supplements and other categories.
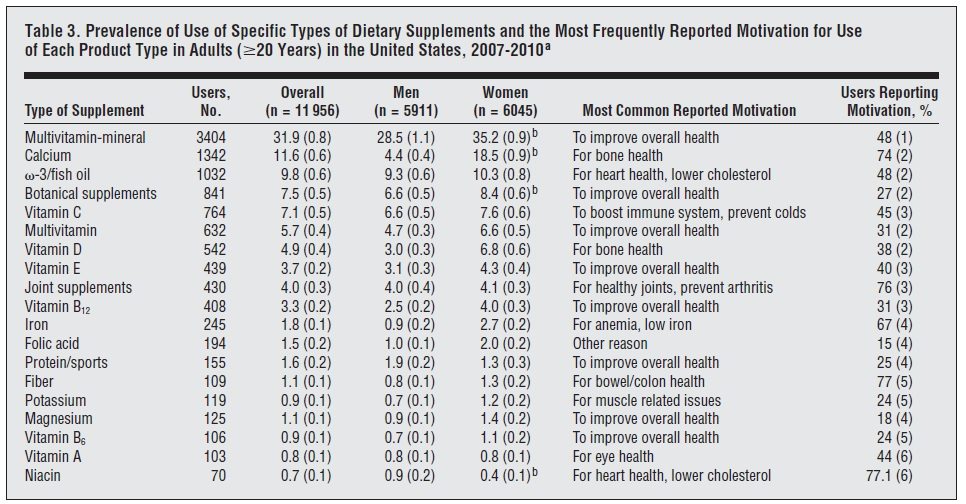
The authors note that 23% of the supplements reported as being used were recommended by a health professional (not defined), whose top recommendations matched the top supplements reported overall. This suggests that over 75% of supplement decisions are being made without (or despite) the recommendation of a health professional.
Other studies
A related survey, also recently published in JAMA Internal Medicine, Users’ Views of Dietary Supplements, gives additional insight to the NHANES survey on motivations for use of supplements. Blendon and colleagues at the Harvard School of Public Health conducted a telephone survey of 1579 people aged 18 or older. This survey asked specifically about dietary supplements but not vitamins or mineral, and identified 584 supplement users. 38% reported taking any supplement in the past two years, and 13% reported taking a supplement regularly — which appears in the ballpark of the NHANES study, if you pull out vitamins. Fish oil/omega-3 oils were the most common consumed (again, consistent with NHANES) with 24% consuming the product in the past two years. Reasons reported for taking supplements included:
- “to feel better” (41%)
- “to improve your overall energy levels” (41%)
- “to boost your immune system” (36%)
- “digestive issues” (28%)
- “lower cholesterol” (21%)
Over 80% reported it was important to have access to supplements. Interestingly, users were asked how government-sponsored efficacy studies would influence their decision to take a supplement. Amazingly, only 25% of users said they would stop using a supplement if it was evaluated to be ineffective. Also interesting: 36% of supplement users had not told their physician about their supplement use, while 31% reported a physician or nurse had recommended their supplement use.
A third study reveals largely consistent information on popularity. From the Military Nutrition Division of the US Army, it’s entitled, Confidence in the efficacy and safety of dietary supplements among United States active duty army personnel, and was published in BMC Complementary and Alternative Medicine in 2012. This was a survey of 990 soldiers in 2006-07 at 11 military bases that focused on motivations, not specific products taken. A dietician or other health professional administered the questionnaire directly and asked for usage of supplements as defined by DSHEA. The sample group was mainly male (87%), white (70%), and young (41% were aged 18-24). Just over half (53%) reported using supplements at least once per week during the prior 6 weeks. Usage was observed to be highest among those older in age, better educated, and holding higher ranks, and reporting good/excellent health.
Here’s the evaluation of efficacy:
Two-thirds (67%) of all participants were somewhat confident or extremely/very confident in the efficacy of supplements, which increased to 86% among users. The majority of non-users (62% were not at all confident in supplement efficacy. Those who reported excellent fitness or dietary habits were much more likely to be very/extremely confident in supplement efficacy.
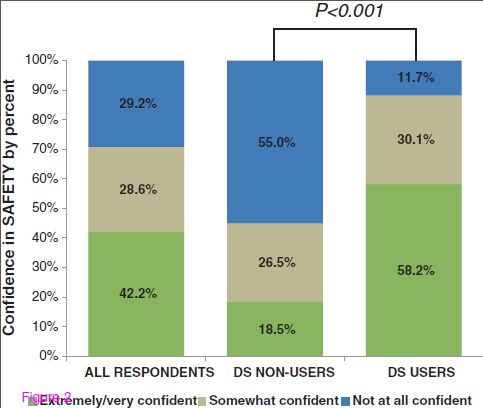
Here’s the evaluation of safety:
The patterns are largely similar. 71% of all respondents were somewhat or extremely/very confident in supplement safety, increasing to 88% among users. Again, the majority of non-users (55%) lacked confidence in the safety of supplements. The same patterns with self-reported excellent fitness/dietary habits and confidence in safety were also observed.
When asked about regulation, few understood the current regulatory structure, with nearly half indicating they didn’t know if there were requirements the supplements work as advertised. Belief that supplements must be safe for consumption was more common among users (38%) than non-users (25%).
On balance, the survey reveals that soldiers that use supplements are confident in their efficacy and safety, and that this confidence is highest among those that believe current regulations require supplements to be both safe and effective.
What does it mean?
Survey on supplement consumption report widespread use, which seems to be based on perceptions that these products are both safe and effective. While supplement use of all kinds is common, it’s multivitamin/minerals that really push the overall consumption rates up. Take that away, and regular usage of other kinds of supplements drops down to just over 10% of the population. When looked at over longer time frames, however, the Harvard survey suggests that 40% do take some form of non-vitamin supplement at least intermittently.
The reasons for taking supplements varies. In the case of multivitamins, it seems to be based around the belief that their consumption will offer meaningful benefits. Yet on balance, there is little evidence to support general supplementation, and in the absence of a deficiency, no evidence multivitamins will boost mood or energy levels. For the most common reasons cited for supplements, expectations are generalized and fairly non-specific. Many may be taking multivitamins as an insurance policy — not a strategy that I’d routinely endorse, given the evidence, but one that is not uncommon. And certainly there is some vitamin and supplement use that is appropriate and evidence-based.
Most of the decision-making around vitamin and supplement use appears to occur without the input of a health professional, raising questions about the rationale for use. And perhaps not surprisingly, few subsequently tell their health professionals about their supplement use. Medical evidence may not be a factor in decisions to take these products. Instead they may be based on perceptions or attitudes that they’re beneficial, perhaps because of confidence in regulations that allow their sale, or the resulting marketing that exaggerates expected benefits. What’s most surprising is that the scientific evidence may not matter at all. It’s said that you can’t reason people out of a decision they didn’t reason themselves into. Perhaps that’s the case with supplements. Certainly it illustrates the need for a more thoughtful (and yes, science-based) approach to promoting health behavior change in individuals. For health professionals interested in improving the safe and appropriate use of vitamins and supplements, and reducing unnecessary or inappropriate use, we need better strategies to promote change.
References
Bailey R.L. Why US Adults Use Dietary Supplements, JAMA Internal Medicine, 1. DOI: 10.1001/jamainternmed.2013.2299
Blendon R.J. (2013). Users’ Views of Dietary Supplements, JAMA Internal Medicine, 173 (1) 74. DOI: 10.1001/2013.jamainternmed.311
Carvey C.E., Farina E.K. & Lieberman H.R. (2012). Confidence in the efficacy and safety of dietary supplements among United States active duty army personnel, BMC Complementary and Alternative Medicine, 12 (1) 182. DOI: 10.1186/1472-6882-12-182